Abstract
Crit Care Sci. 2024;36:e20240176en
DOI 10.62675/2965-2774.20240176-en
To systematically review the effect of the prone position on endotracheal intubation and mortality in nonintubated COVID-19 patients with acute respiratory distress syndrome.
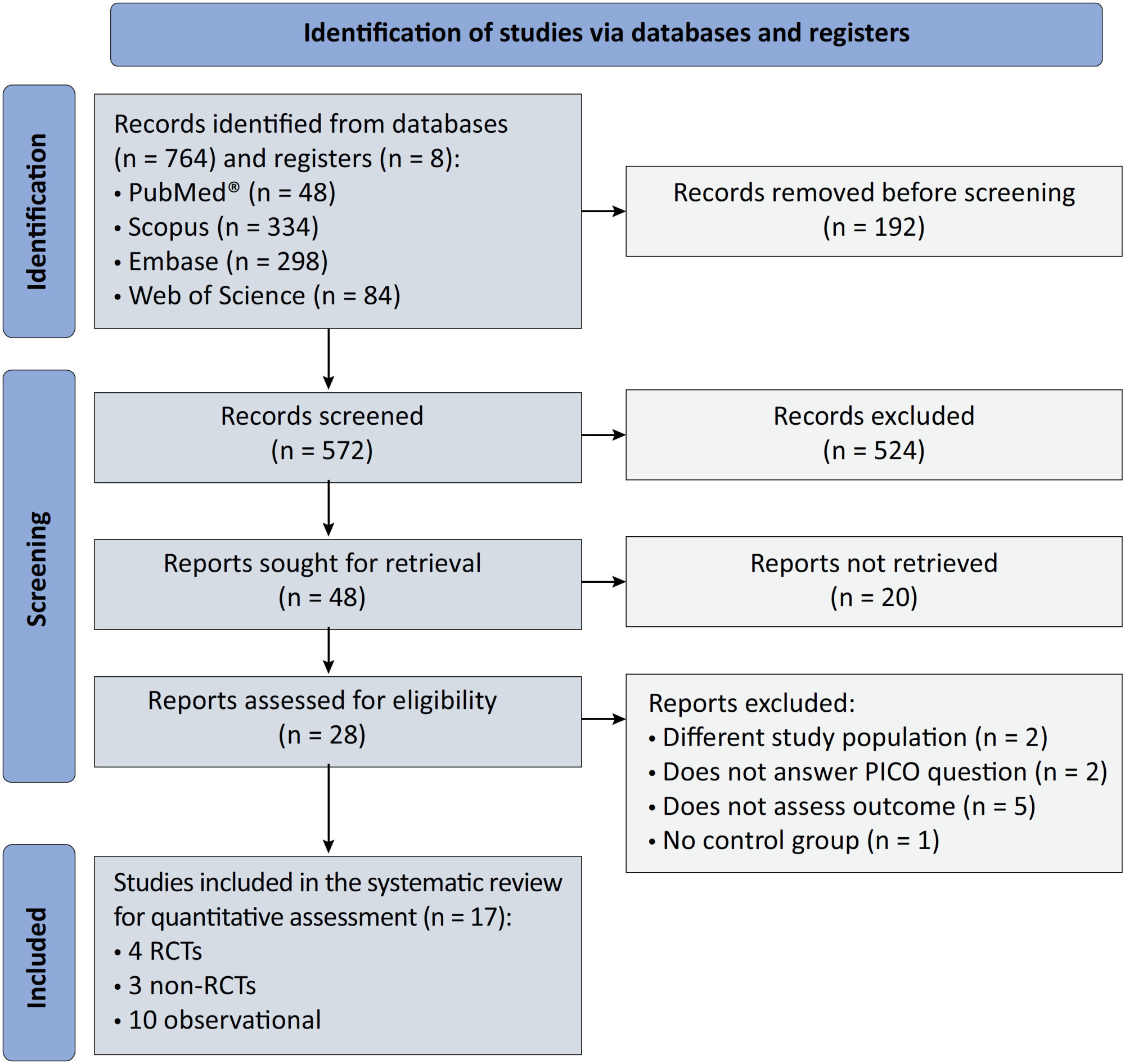
We registered the protocol (CRD42021286711) and searched for four databases and gray literature from inception to December 31, 2022. We included observational studies and clinical trials. There was no limit by date or the language of publication. We excluded case reports, case series, studies not available in full text, and those studies that included children < 18-years-old.
We included ten observational studies, eight clinical trials, 3,969 patients, 1,120 endotracheal intubation events, and 843 deaths. All of the studies had a low risk of bias (Newcastle-Ottawa Scale and Risk of Bias 2 tools). We found that the conscious prone position decreased the odds of endotracheal intubation by 44% (OR 0.56; 95%CI 0.40 - 0.78) and mortality by 43% (OR 0.57; 95%CI 0.39 - 0.84) in nonintubated COVID-19 patients with acute respiratory distress syndrome. This protective effect on endotracheal intubation and mortality was more robust in those who spent > 8 hours/day in the conscious prone position (OR 0.43; 95%CI 0.26 - 0.72 and OR 0.38; 95%CI 0.24 - 0.60, respectively). The certainty of the evidence according to the GRADE criteria was moderate.
The conscious prone position decreased the odds of endotracheal intubation and mortality, especially when patients spent over 8 hours/day in the conscious prone position and treatment in the intensive care unit. However, our results should be cautiously interpreted due to limitations in evaluating randomized clinical trials, nonrandomized clinical trials and observational studies. However, despite systematic reviews with meta-analyses of randomized clinical trials, we must keep in mind that these studies remain heterogeneous from a clinical and methodological point of view.
Abstract
Crit Care Sci. 2023;35(4):345-354
DOI 10.5935/2965-2774.20230162-pt
The optimal target for blood glucose concentration in critically ill patients is unclear. We will perform a systematic review and meta-analysis with aggregated and individual patient data from randomized controlled trials, comparing intensive glucose control with liberal glucose control in critically ill adults.
MEDLINE®, Embase, the Cochrane Central Register of Clinical Trials, and clinical trials registries (World Health Organization, clinical trials.gov). The authors of eligible trials will be invited to provide individual patient data. Published trial-level data from eligible trials that are not at high risk of bias will be included in an aggregated data meta-analysis if individual patient data are not available.
Inclusion criteria: randomized controlled trials that recruited adult patients, targeting a blood glucose of ≤ 120mg/dL (≤ 6.6mmol/L) compared to a higher blood glucose concentration target using intravenous insulin in both groups. Excluded studies: those with an upper limit blood glucose target in the intervention group of > 120mg/dL (> 6.6mmol/L), or where intensive glucose control was only performed in the intraoperative period, and those where loss to follow-up exceeded 10% by hospital discharge.
In-hospital mortality during index hospital admission. Secondary endpoints: mortality and survival at other timepoints, duration of invasive mechanical ventilation, vasoactive agents, and renal replacement therapy. A random effect Bayesian meta-analysis and hierarchical Bayesian models for individual patient data will be used.
This systematic review with aggregate and individual patient data will address the clinical question, ‘what is the best blood glucose target for critically ill patients overall?’
Abstract
Crit Care Sci. 2023;35(3):302-310
DOI 10.5935/2965-2774.20230141-pt
To evaluate the accuracy of the persistent AKI risk index (PARI) in predicting acute kidney injury within 72 hours after admission to the intensive care unit, persistent acute kidney injury, renal replacement therapy, and death within 7 days in patients hospitalized due to acute respiratory failure.
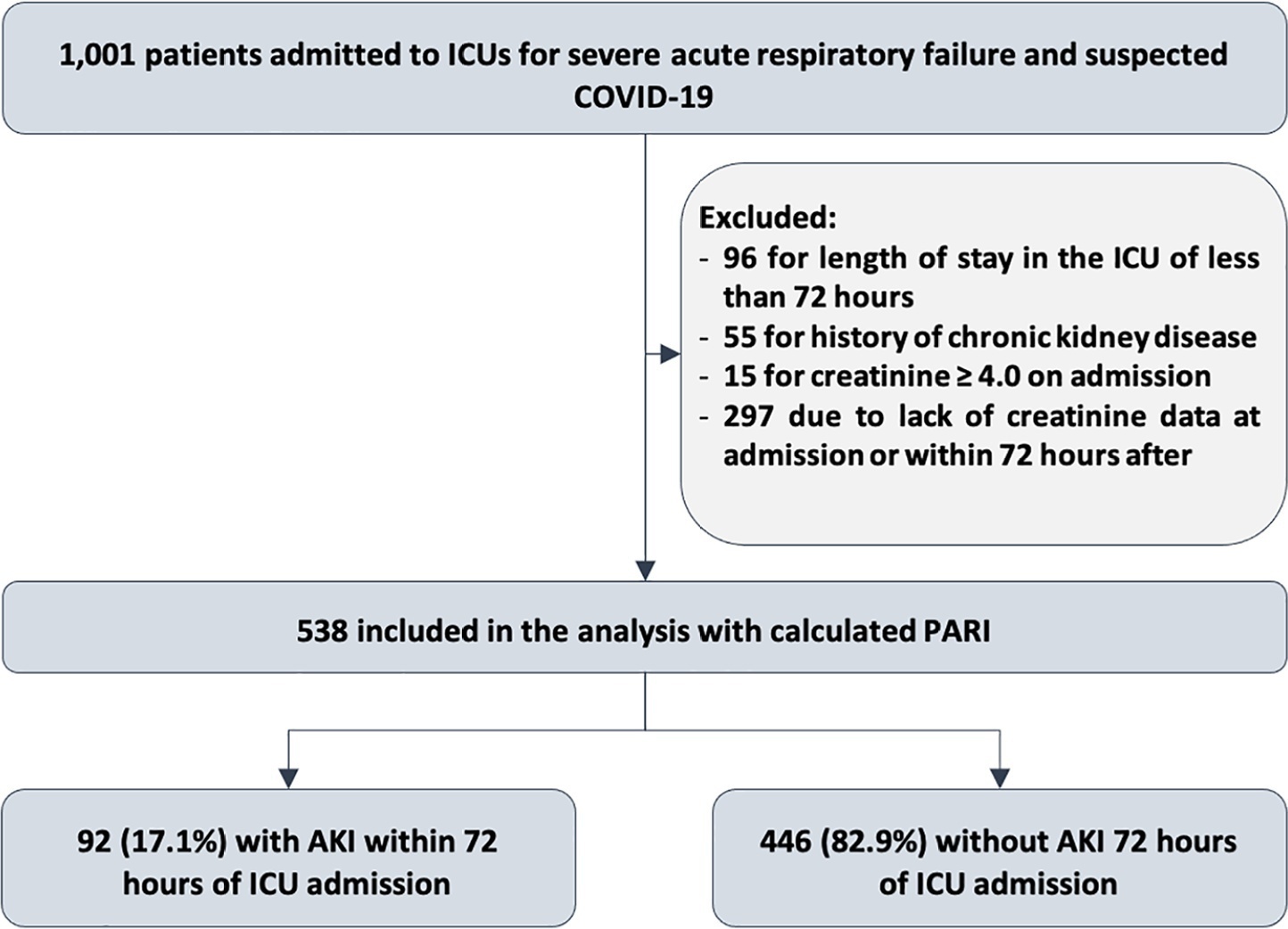
This study was done in a cohort of diagnoses of consecutive adult patients admitted to the intensive care unit of eight hospitals in Curitiba, Brazil, between March and September 2020 due to acute respiratory failure secondary to suspected COVID-19. The COVID-19 diagnosis was confirmed or refuted by RT-PCR for the detection of SARS-CoV-2. The ability of PARI to predict acute kidney injury at 72 hours, persistent acute kidney injury, renal replacement therapy, and death within 7 days was analyzed by ROC curves in comparison to delta creatinine, SOFA, and APACHE II.
Of the 1,001 patients in the cohort, 538 were included in the analysis. The mean age was 62 ± 17 years, 54.8% were men, and the median APACHE II score was 12. At admission, the median SOFA score was 3, and 83.3% had no renal dysfunction. After admission to the intensive care unit, 17.1% had acute kidney injury within 72 hours, and through 7 days, 19.5% had persistent acute kidney injury, 5% underwent renal replacement therapy, and 17.1% died. The PARI had an area under the ROC curve of 0.75 (0.696 - 0.807) for the prediction of acute kidney injury at 72 hours, 0.71 (0.613 - 0.807) for renal replacement therapy, and 0.64 (0.565 - 0.710) for death.
The PARI has acceptable accuracy in predicting acute kidney injury within 72 hours and renal replacement therapy within 7 days of admission to the intensive care unit, but it is not significantly better than the other scores.
Abstract
Crit Care Sci. 2023;35(2):187-195
DOI 10.5935/2965-2774.20230378-pt
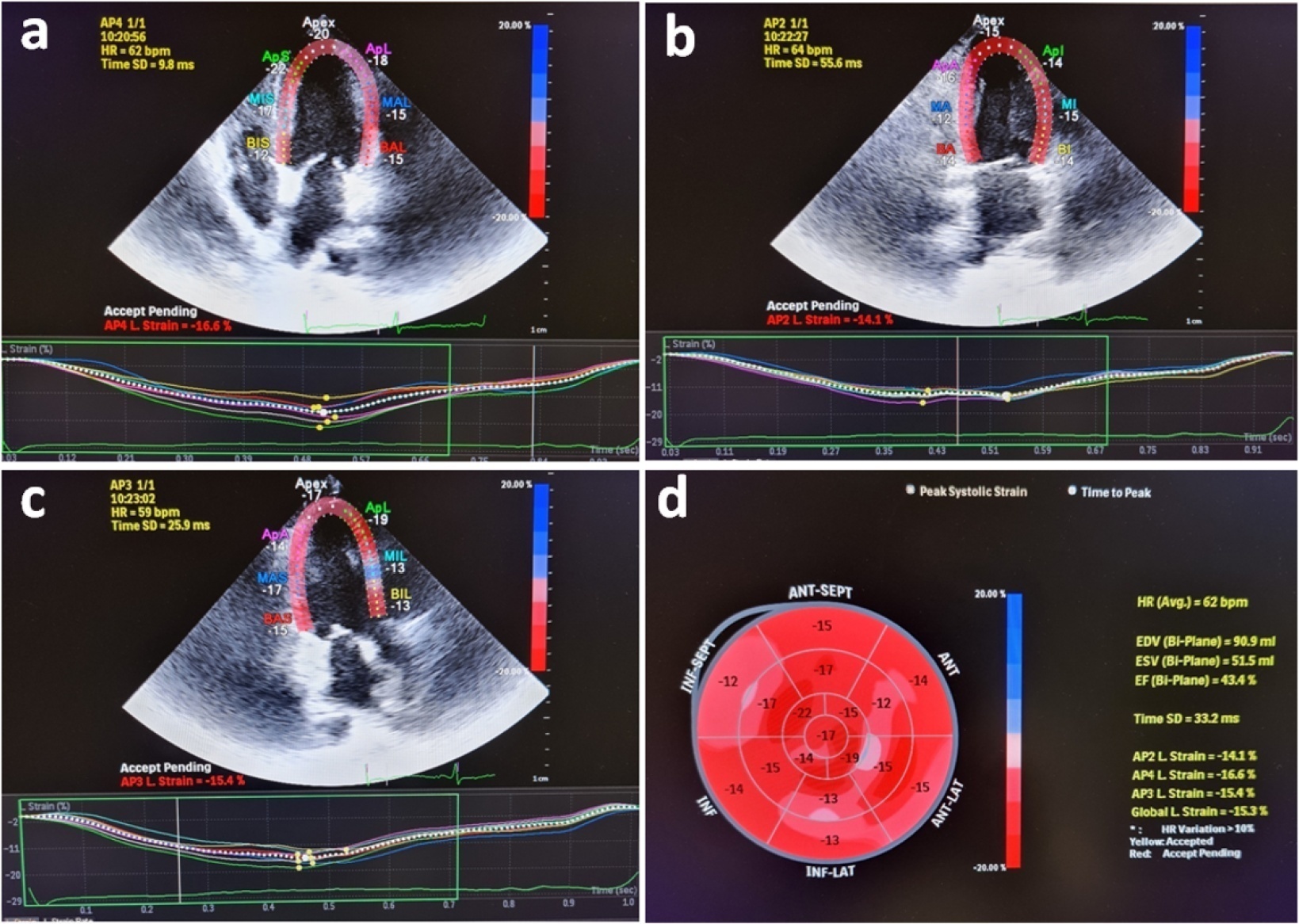
Evaluation of left ventricular systolic function using speckle tracking echocardiography is more sensitive than conventional echocardiographic measurement in detecting subtle left ventricular dysfunction in septic patients. Our purpose was to investigate the predictive significance of left ventricular global longitudinal strain in normotensive septic intensive care patients.
This observational, prospective cohort study included septic normotensive adults admitted to the intensive care unit between June 1, 2021, and August 31, 2021. Left ventricular systolic function was measured using speckle-tracking echocardiography within 24 hours of admission.
One hundred fifty-two patients were enrolled. The intensive care unit mortality rate was 27%. Left ventricular global longitudinal strain was less negative, which indicated worse left ventricular function in non-survivors than survivors (median [interquartile range], -15.2 [-17.2 - -12.5] versus -17.3 [-18.8 - -15.5]; p < 0.001). The optimal cutoff value for left ventricular global longitudinal strain was -17% in predicting intensive care unit mortality (area under the curve, 0.728). Patients with left ventricular global longitudinal strain > -17% (less negative than -17%, which indicated worse left ventricular function) showed a significantly higher mortality rate (39.2% versus 13.7%; p < 0.001). According to multivariate analysis, left ventricular global longitudinal strain was an independent predictor of intensive care unit mortality [OR (95%CI), 1.326 (1.038 - 1.693); p = 0.024], along with invasive mechanical ventilation and Glasgow coma scale, APACHE II, and SOFA risk scores.
Impaired left ventricular global longitudinal strain is associated with mortality and provided predictive data in normotensive septic intensive care patients.
Abstract
Crit Care Sci. 2023;35(2):217-225
DOI 10.5935/2965-2774.20230289-pt
To analyze the effect of CytoSorb® on mortality, interleukin levels, vasopressor use and adverse events in patients with sepsis.
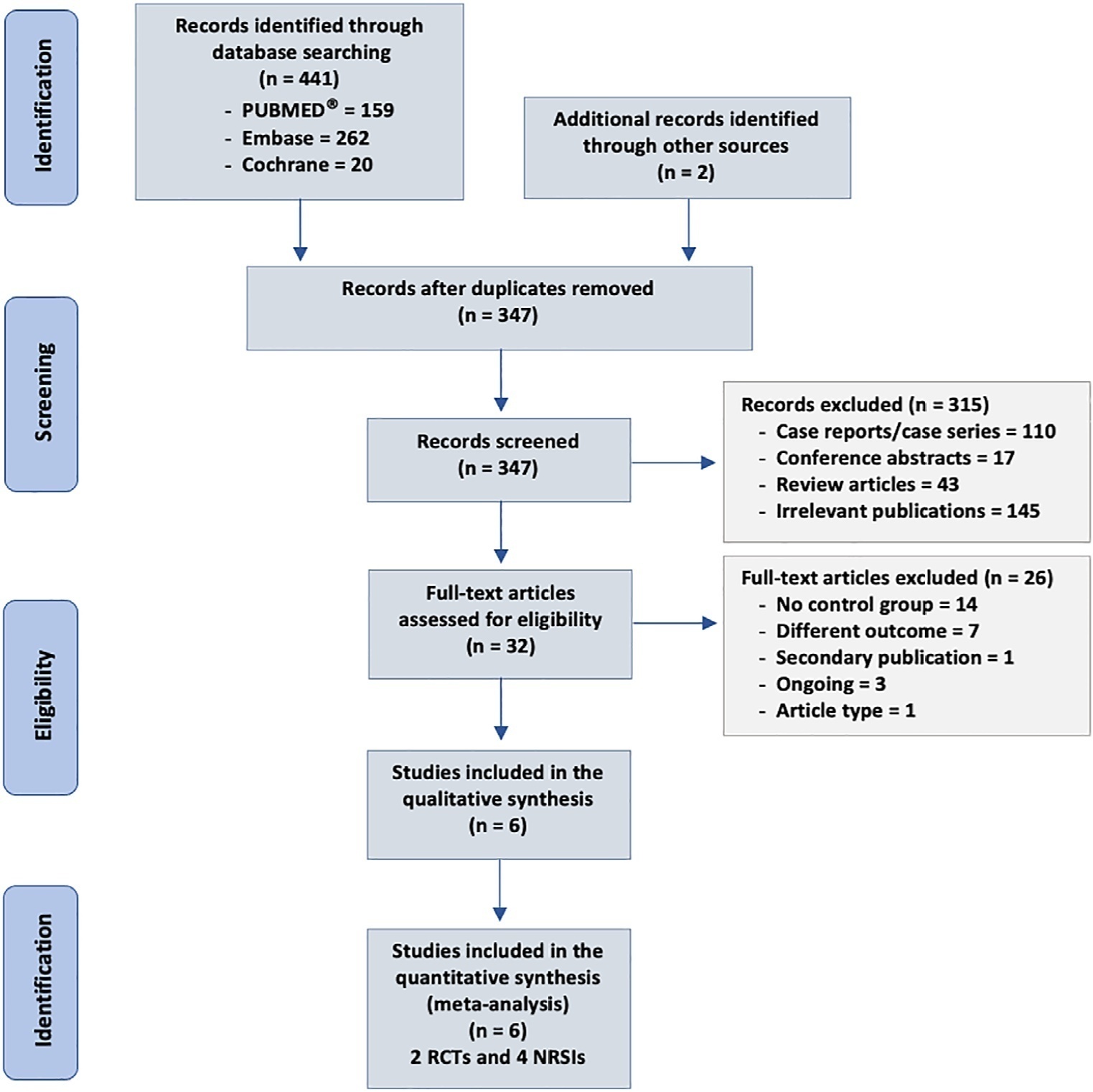
We searched MEDLINE®, Embase and the Cochrane Library for randomized controlled trials and cohort studies that reported the use of CytoSorb® among septic patients. The primary outcome was mortality, and secondary outcomes included the use of vasopressors, levels of inflammatory markers, predicted versus observed mortality, length of stay in the intensive care unit, and adverse events.
We included 6 studies enrolling 413 patients, and assessment for risk of bias indicated variations in study quality from high to moderate. The overall mortality rate was 45%, and no significant effect on mortality was found at 28 - 30 days (RR 0.98 [0.12 - 8.25] for the randomized clinical trial and RR 0.74 [0.49 - 1.13] for cohort studies). We did not perform a metanalysis for other outcomes due to the small number of studies found or the lack of data.
Our study found very low certainty evidence, due to imprecision, risk of bias, and heterogeneity, thereby showing no benefit of CytoSorb® use in terms of mortality at 28 - 30 days. We cannot recommend the use of CytoSorb® in septic or septic shock patients outside clinical trials. Further high-quality randomized trials with a common intervention arm are needed to evaluate the influence of CytoSorb® in this population.
Abstract
Crit Care Sci. 2023;35(1):19-30
DOI 10.5935/2965-2774.20230203-pt
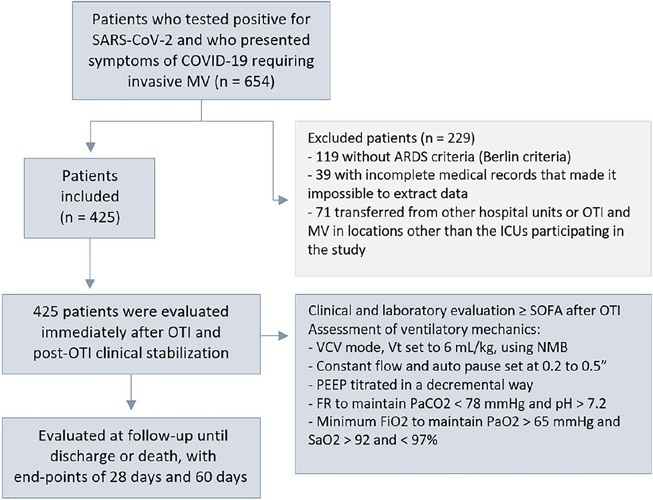
To evaluate the factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19.
This was a retrospective, multicenter cohort study that included 425 mechanically ventilated adult patients with COVID-19 admitted to 4 intensive care units. Clinical data comprising the SOFA score, laboratory data and mechanical characteristics of the respiratory system were collected in a standardized way immediately after the start of invasive mechanical ventilation. The risk factors for death were analyzed using Cox regression to estimate the risk ratios and their respective 95%CIs.
Body mass index (RR 1.17; 95%CI 1.11 - 1.20; p < 0.001), SOFA score (RR 1.39; 95%CI 1.31 - 1.49; p < 0.001) and driving pressure (RR 1.24; 95%CI 1.21 - 1.29; p < 0.001) were considered independent factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19. Respiratory system compliance (RR 0.92; 95%CI 0.90 - 0.93; p < 0.001) was associated with lower mortality. The comparative analysis of the survival curves indicated that patients with respiratory system compliance (< 30mL/cmH2O), a higher SOFA score (> 5 points) and higher driving pressure (> 14cmH2O) were more significantly associated with the outcome of death at 28 days and 60 days.
Patients with a body mass index > 32kg/m2, respiratory system compliance < 30mL/cmH2O, driving pressure > 14cmH2O and SOFA score > 5.8 immediately after the initiation of invasive ventilatory support had worse outcomes, and independent risk factors were associated with higher mortality in this population.
Abstract
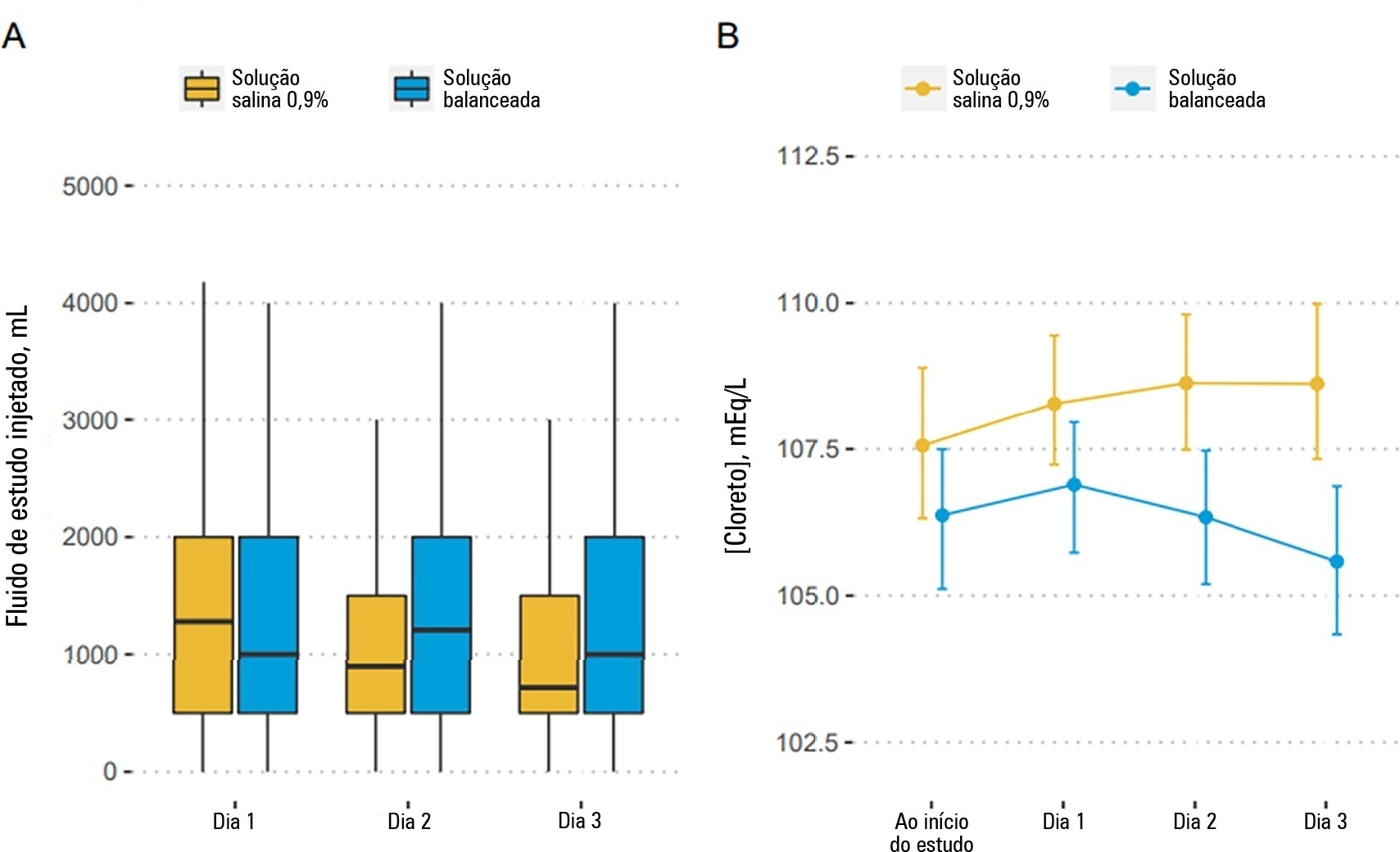
Rev Bras Ter Intensiva. 2022;34(4):410-417
DOI 10.5935/0103-507X.20220261-en
To describe the effects of balanced solution use on the short-term outcomes of patients with traumatic brain injury enrolled in BaSICS trial.
Patients were randomized to receive either 0.9% saline or balanced solution during their intensive care unit stay. The primary endpoint was 90-day mortality, and the secondary outcomes were days alive and free of intensive care unit stay at 28 days. The primary endpoint was assessed using Bayesian logistic regression. The secondary endpoint was assessed using a Bayesian zero-inflated beta binomial regression.
We included 483 patients (236 in the 0.9% saline arm and 247 in the balanced solution arm). A total of 338 patients (70%) with a Glasgow coma scale score ≤ 12 were enrolled. The overall probability that balanced solutions were associated with higher 90-day mortality was 0.98 (OR 1.48; 95%CrI 1.04 - 2.09); this mortality increment was particularly noticeable in patients with a Glasgow coma scale score below 6 at enrollment (probability of harm of 0.99). Balanced solutions were associated with -1.64 days alive and free of intensive care unit at 28 days (95%CrI -3.32 - 0.00) with a probability of harm of 0.97.
There was a high probability that balanced solutions were associated with high 90-day mortality and fewer days alive and free of intensive care units at 28 days.
Abstract
Rev Bras Ter Intensiva. 2022;34(2):220-226
DOI 10.5935/0103-507X.20220019-en
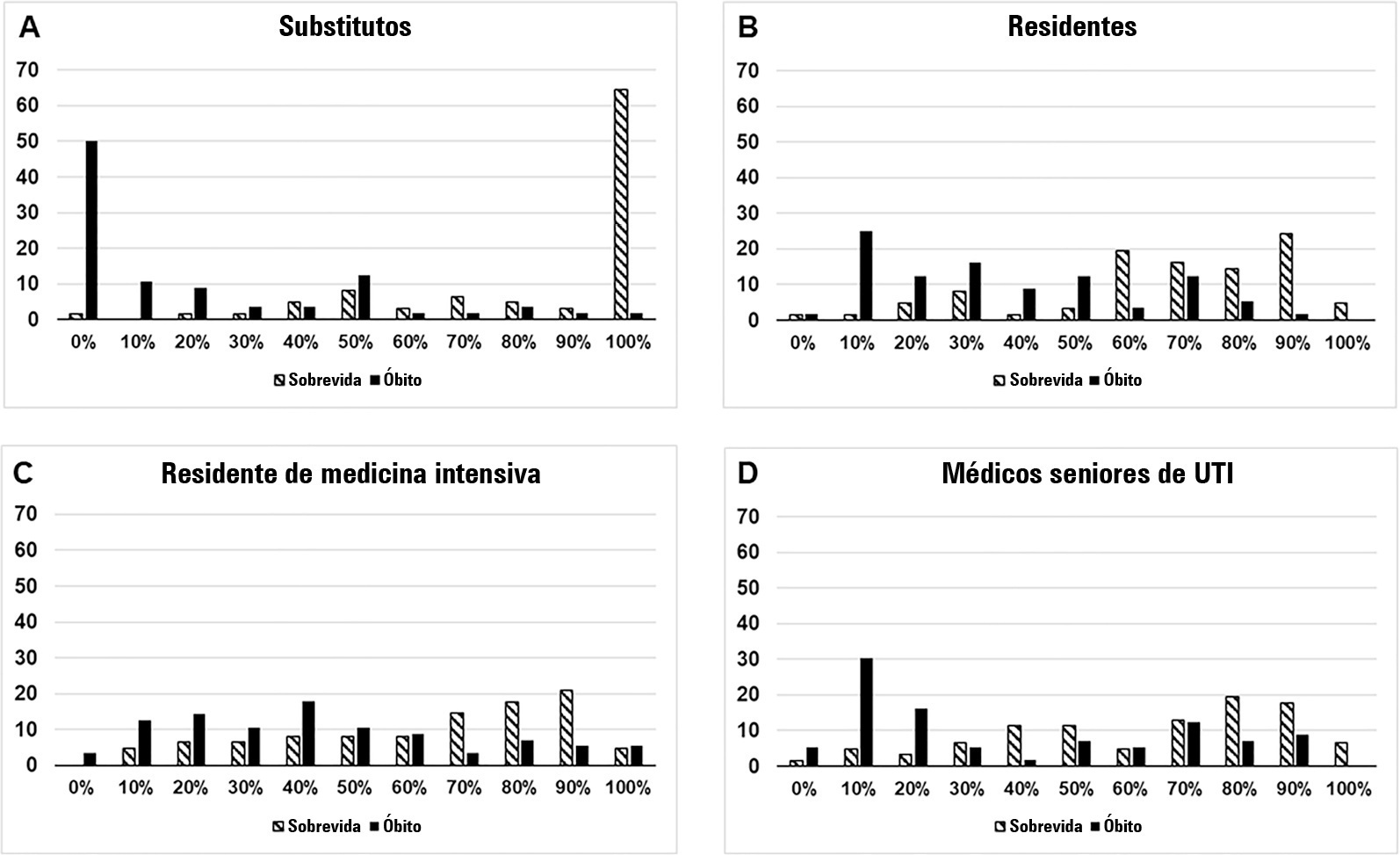
To compare the predictive performance of residents, senior intensive care unit physicians and surrogates early during intensive care unit stays and to evaluate whether different presentations of prognostic data (probability of survival versus probability of death) influenced their performance.
We questioned surrogates and physicians in charge of critically ill patients during the first 48 hours of intensive care unit admission on the patient’s probability of hospital outcome. The question framing (i.e., probability of survival versus probability of death during hospitalization) was randomized. To evaluate the predictive performance, we compared the areas under the ROC curves (AUCs) for hospital outcome between surrogates and physicians’ categories. We also stratified the results according to randomized question framing.
We interviewed surrogates and physicians on the hospital outcomes of 118 patients. The predictive performance of surrogate decisionmakers was significantly lower than that of physicians (AUC of 0.63 for surrogates, 0.82 for residents, 0.80 for intensive care unit fellows and 0.81 for intensive care unit senior physicians). There was no increase in predictive performance related to physicians’ experience (i.e., senior physicians did not predict outcomes better than junior physicians). Surrogate decisionmakers worsened their prediction performance when they were asked about probability of death instead of probability of survival, but there was no difference for physicians.
Different predictive performance was observed when comparing surrogate decision-makers and physicians, with no effect of experience on health care professionals’ prediction. Question framing affected the predictive performance of surrogates but not of physicians.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) ICU (25) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)