Abstract
Crit Care Sci. 2023;35(2):117-146
DOI 10.5935/2965-2774.20230310-pt
Echocardiography in critically ill patients has become essential in the evaluation of patients in different settings, such as the hospital. However, unlike for other matters related to the care of these patients, there are still no recommendations from national medical societies on the subject. The objective of this document was to organize and make available expert consensus opinions that may help to better incorporate echocardiography in the evaluation of critically ill patients. Thus, the Associação de Medicina Intensiva Brasileira, the Associação Brasileira de Medicina de Emergência, and the Sociedade Brasileira de Medicina Hospitalar formed a group of 17 physicians to formulate questions relevant to the topic and discuss the possibility of consensus for each of them. All questions were prepared using a five-point Likert scale. Consensus was defined a priori as at least 80% of the responses between one and two or between four and five. The consideration of the issues involved two rounds of voting and debate among all participants. The 27 questions prepared make up the present document and are divided into 4 major assessment areas: left ventricular function, right ventricular function, diagnosis of shock, and hemodynamics. At the end of the process, there were 17 positive (agreement) and 3 negative (disagreement) consensuses; another 7 questions remained without consensus. Although areas of uncertainty persist, this document brings together consensus opinions on several issues related to echocardiography in critically ill patients and may enhance its development in the national scenario.
Abstract
Crit Care Sci. 2023;35(2):187-195
DOI 10.5935/2965-2774.20230378-pt
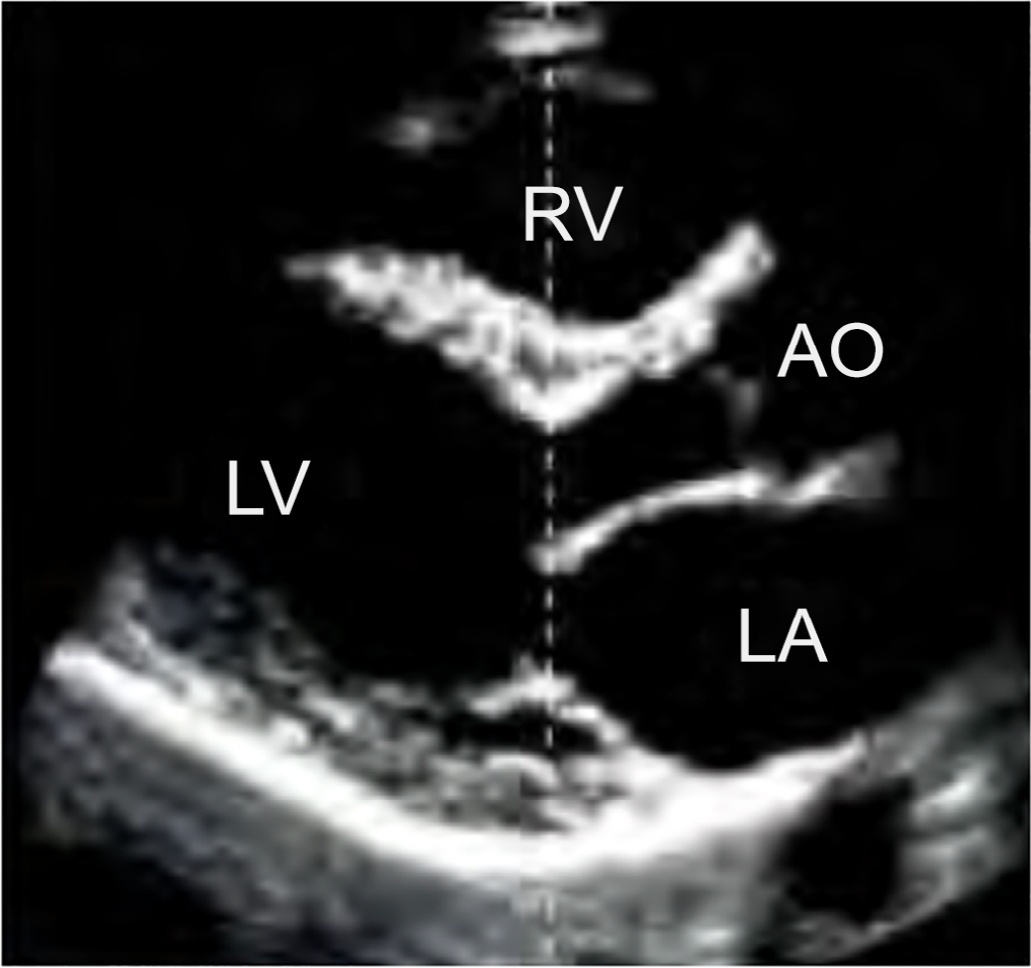
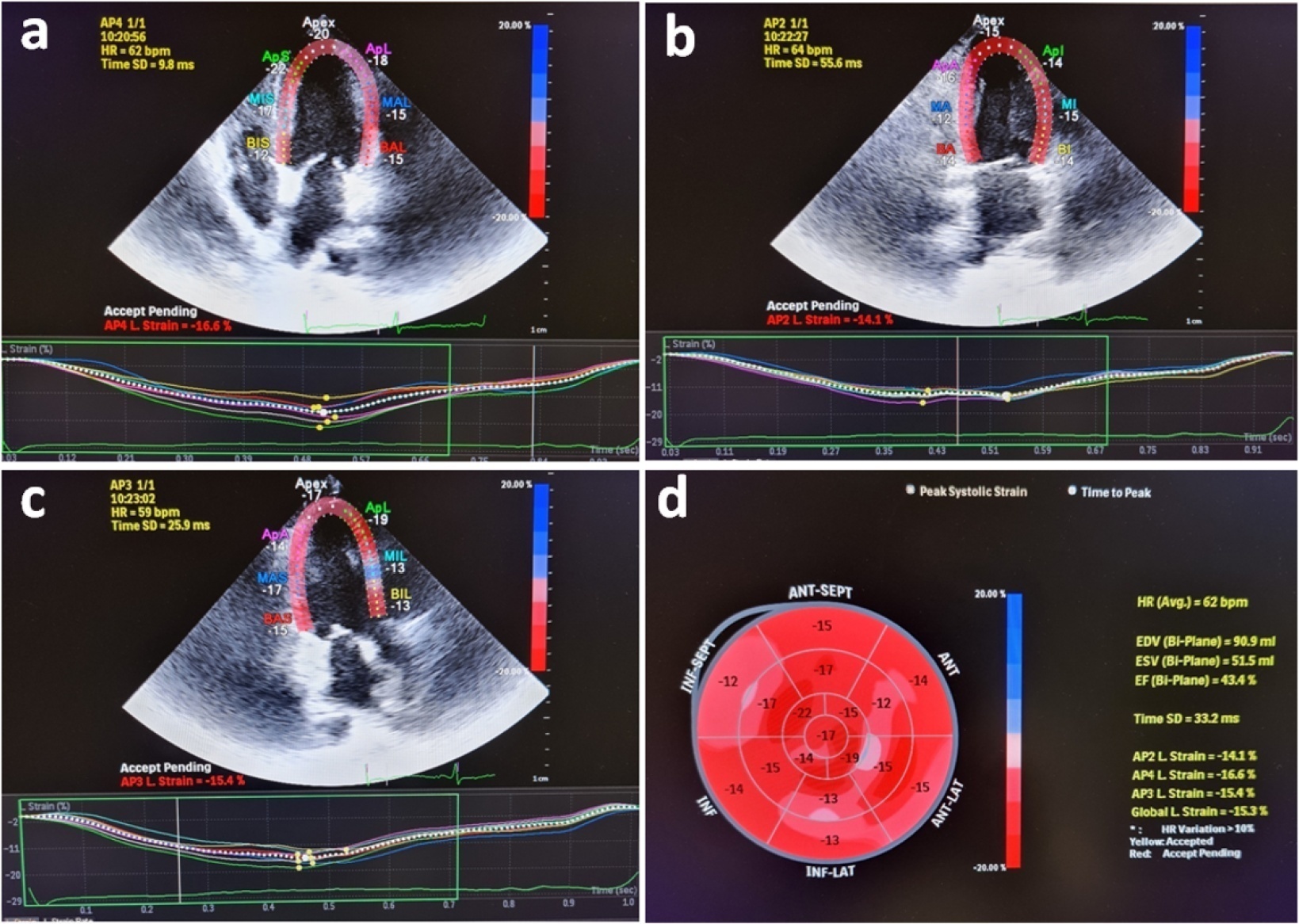
Evaluation of left ventricular systolic function using speckle tracking echocardiography is more sensitive than conventional echocardiographic measurement in detecting subtle left ventricular dysfunction in septic patients. Our purpose was to investigate the predictive significance of left ventricular global longitudinal strain in normotensive septic intensive care patients.
This observational, prospective cohort study included septic normotensive adults admitted to the intensive care unit between June 1, 2021, and August 31, 2021. Left ventricular systolic function was measured using speckle-tracking echocardiography within 24 hours of admission.
One hundred fifty-two patients were enrolled. The intensive care unit mortality rate was 27%. Left ventricular global longitudinal strain was less negative, which indicated worse left ventricular function in non-survivors than survivors (median [interquartile range], -15.2 [-17.2 - -12.5] versus -17.3 [-18.8 - -15.5]; p < 0.001). The optimal cutoff value for left ventricular global longitudinal strain was -17% in predicting intensive care unit mortality (area under the curve, 0.728). Patients with left ventricular global longitudinal strain > -17% (less negative than -17%, which indicated worse left ventricular function) showed a significantly higher mortality rate (39.2% versus 13.7%; p < 0.001). According to multivariate analysis, left ventricular global longitudinal strain was an independent predictor of intensive care unit mortality [OR (95%CI), 1.326 (1.038 - 1.693); p = 0.024], along with invasive mechanical ventilation and Glasgow coma scale, APACHE II, and SOFA risk scores.
Impaired left ventricular global longitudinal strain is associated with mortality and provided predictive data in normotensive septic intensive care patients.
Abstract
Rev Bras Ter Intensiva. 2022;34(1):96-106
DOI 10.5935/0103-507X.20220004-en
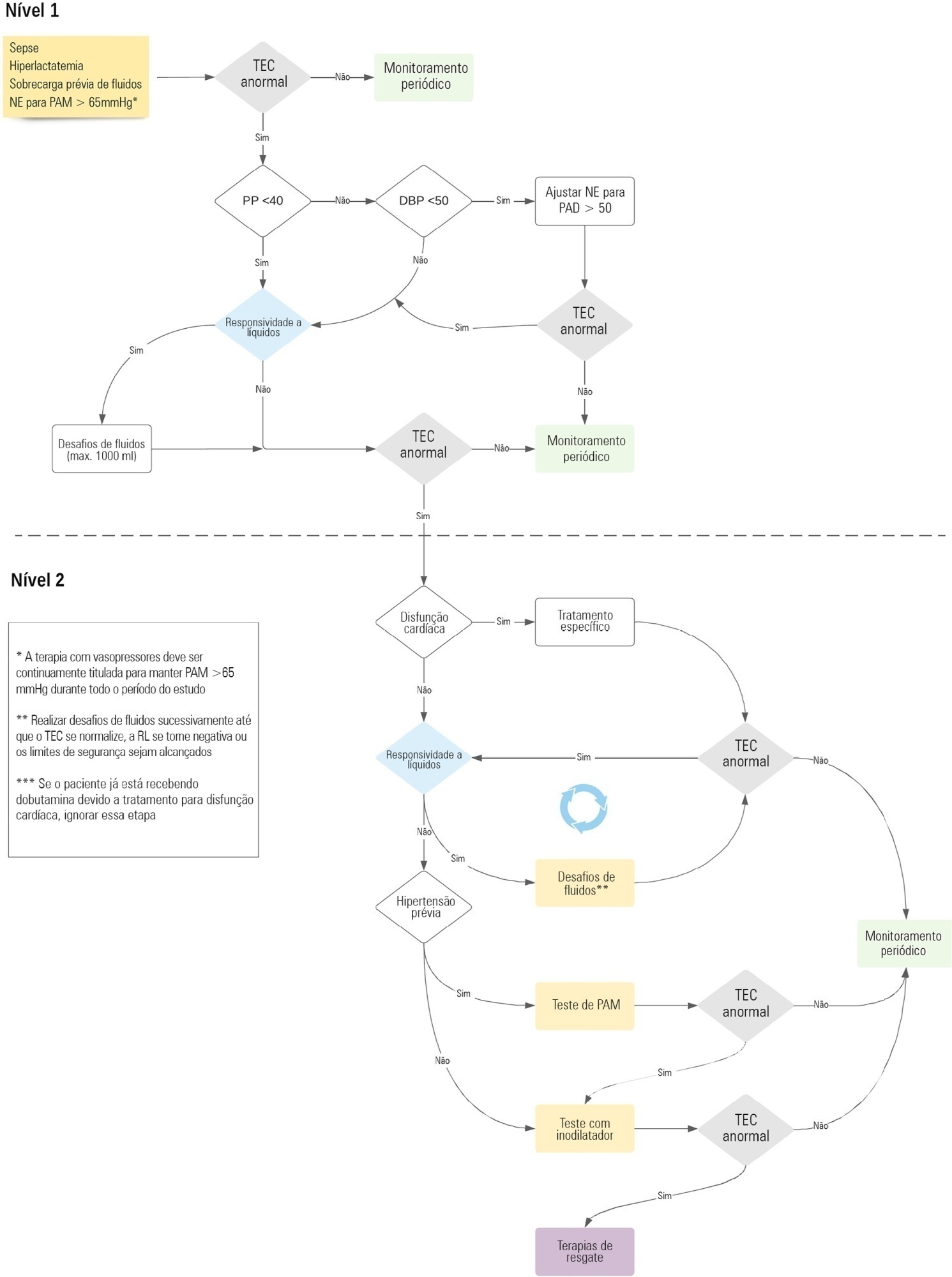
Early reversion of sepsis-induced tissue hypoperfusion is essential for survival in septic shock. However, consensus regarding the best initial resuscitation strategy is lacking given that interventions designed for the entire population with septic shock might produce unnecessary fluid administration. This article reports the rationale, study design and analysis plan of the ANDROMEDA-2 study, which aims to determine whether a peripheral perfusion-guided strategy consisting of capillary refill time-targeted resuscitation based on clinical and hemodynamic phenotypes is associated with a decrease in a composite outcome of mortality, time to organ support cessation, and hospital length of stay compared to standard care in patients with early (< 4 hours of diagnosis) septic shock.
The ANDROMEDA-2 study is a multicenter, multinational randomized controlled trial. In the intervention group, capillary refill time will be measured hourly for 6 hours. If abnormal, patients will enter an algorithm starting with pulse pressure assessment. Patients with pulse pressure less than 40mmHg will be tested for fluid responsiveness and receive fluids accordingly. In patients with pulse pressure > 40mmHg, norepinephrine will be titrated to maintain diastolic arterial pressure > 50mmHg. Patients who fail to normalize capillary refill time after the previous steps will be subjected to critical care echocardiography for cardiac dysfunction evaluation and subsequent management. Finally, vasopressor and inodilator tests will be performed to further optimize perfusion. A sample size of 1,500 patients will provide 88% power to demonstrate superiority of the capillary refill time-targeted strategy.
If hemodynamic phenotype-based, capillary refill time-targeted resuscitation demonstrates to be a superior strategy, care processes in septic shock resuscitation can be optimized with bedside tools.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):474-482
DOI 10.5935/0103-507X.20190073
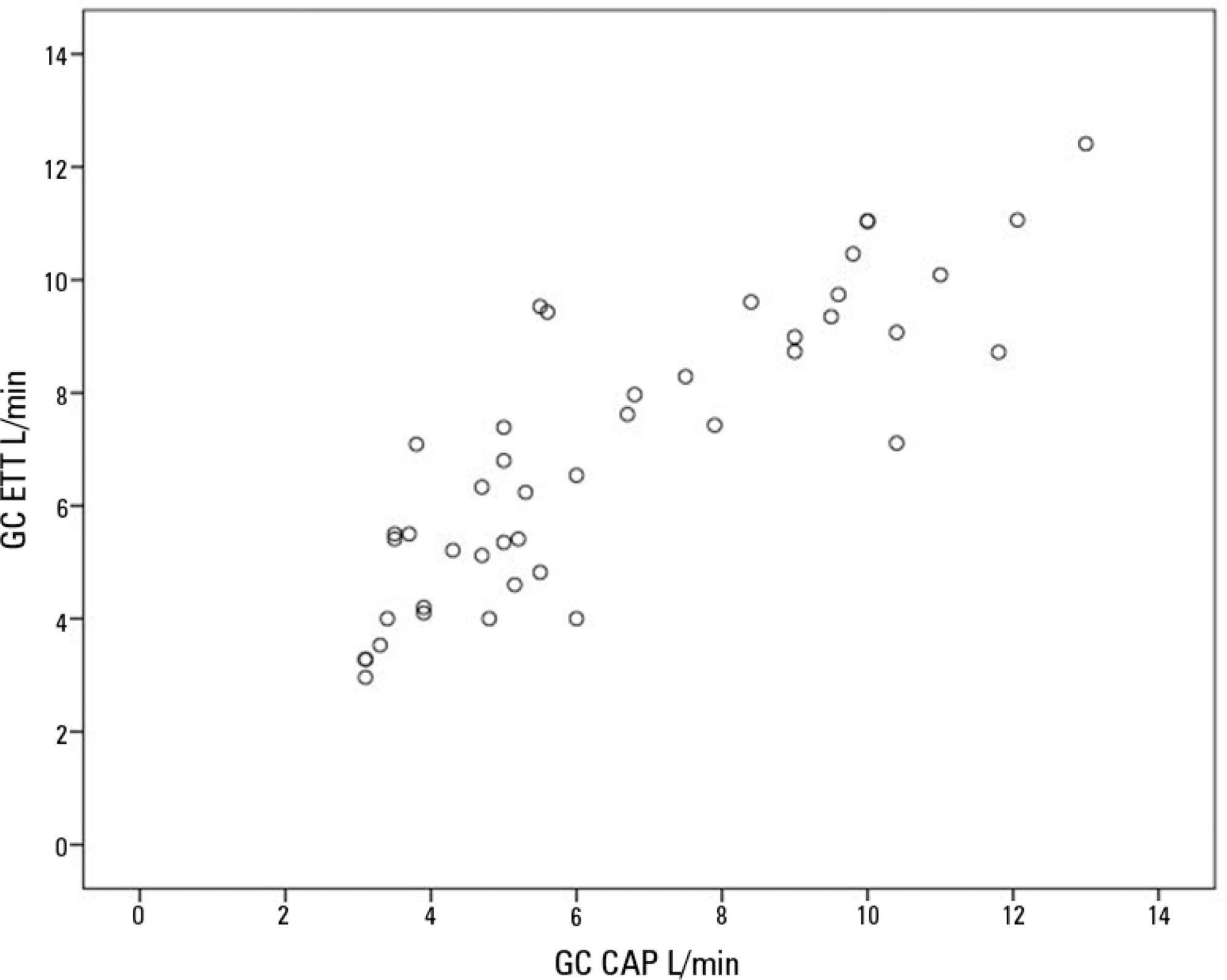
To compare cardiac output measurements by transthoracic echocardiography and a pulmonary artery catheter in mechanically ventilated patients with high positive end-expiratory pressure. To evaluate the effect of tricuspid regurgitation.
Sixteen mechanically ventilated patients were studied. Cardiac output was measured by pulmonary artery catheterization and transthoracic echocardiography. Measurements were performed at different levels of positive end-expiratory pressure (10cmH2O, 15cmH2O, and 20cmH2O). The effect of tricuspid regurgitation on cardiac output measurement was evaluated. The intraclass correlation coefficient was studied; the mean error and limits of agreement were studied with the Bland-Altman plot. The error rate was calculated.
Forty-four pairs of cardiac output measurements were obtained. An intraclass correlation coefficient of 0.908 was found (p < 0.001). The mean error was 0.44L/min for cardiac output values between 5 and 13L/min. The limits of agreement were 3.25L/min and -2.37L/min. With tricuspid insufficiency, the intraclass correlation coefficient was 0.791, and without tricuspid insufficiency, 0.935. Tricuspid insufficiency increased the error rate from 32% to 52%.
In patients with high positive end-expiratory pressure, cardiac output measurement by transthoracic echocardiography is comparable to that with a pulmonary artery catheter. Tricuspid regurgitation influences the intraclass correlation coefficient. In patients with high positive end-expiratory pressure, the use of transthoracic echocardiography to measure cardiac output is comparable to invasive measures.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):312-317
DOI 10.5935/0103-507X.20190056
To investigate the influence of respiratory distress syndrome management on clinical and echocardiographic parameters used for hemodynamic evaluation in ≤ 32- week newborns.
Thirty-three ≤ 32-week newborns were prospectively evaluated and subjected to invasive mechanical ventilation. The need for exogenous surfactant and clinical and echocardiographic parameters in the first 24 hours of life was detailed in this group of patients.
The mean airway pressure was significantly higher in newborn infants who required inotropes [10.8 (8.8 - 23) cmH2O versus 9 (6.2 - 12) cmH2O; p = 0.04]. A negative correlation was found between the mean airway pressure and velocity-time integral of the pulmonary artery (r = -0.39; p = 0.026), right ventricular output (r = -0.43; p = 0.017) and measurements of the tricuspid annular plane excursion (r = -0.37; p = 0.036). A negative correlation was found between the number of doses of exogenous surfactant and the right ventricular output (r = -0.39; p = 0.028) and pulmonary artery velocity-time integral (r = -0.35; p = 0.043).
In ≤ 32-week newborns under invasive mechanical ventilation, increases in the mean airway pressure and number of surfactant doses are correlated with the worsening of early cardiac function. Therefore, more aggressive management of respiratory distress syndrome may contribute to the hemodynamic instability of these patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):240-247
DOI 10.5935/0103-507X.20190039
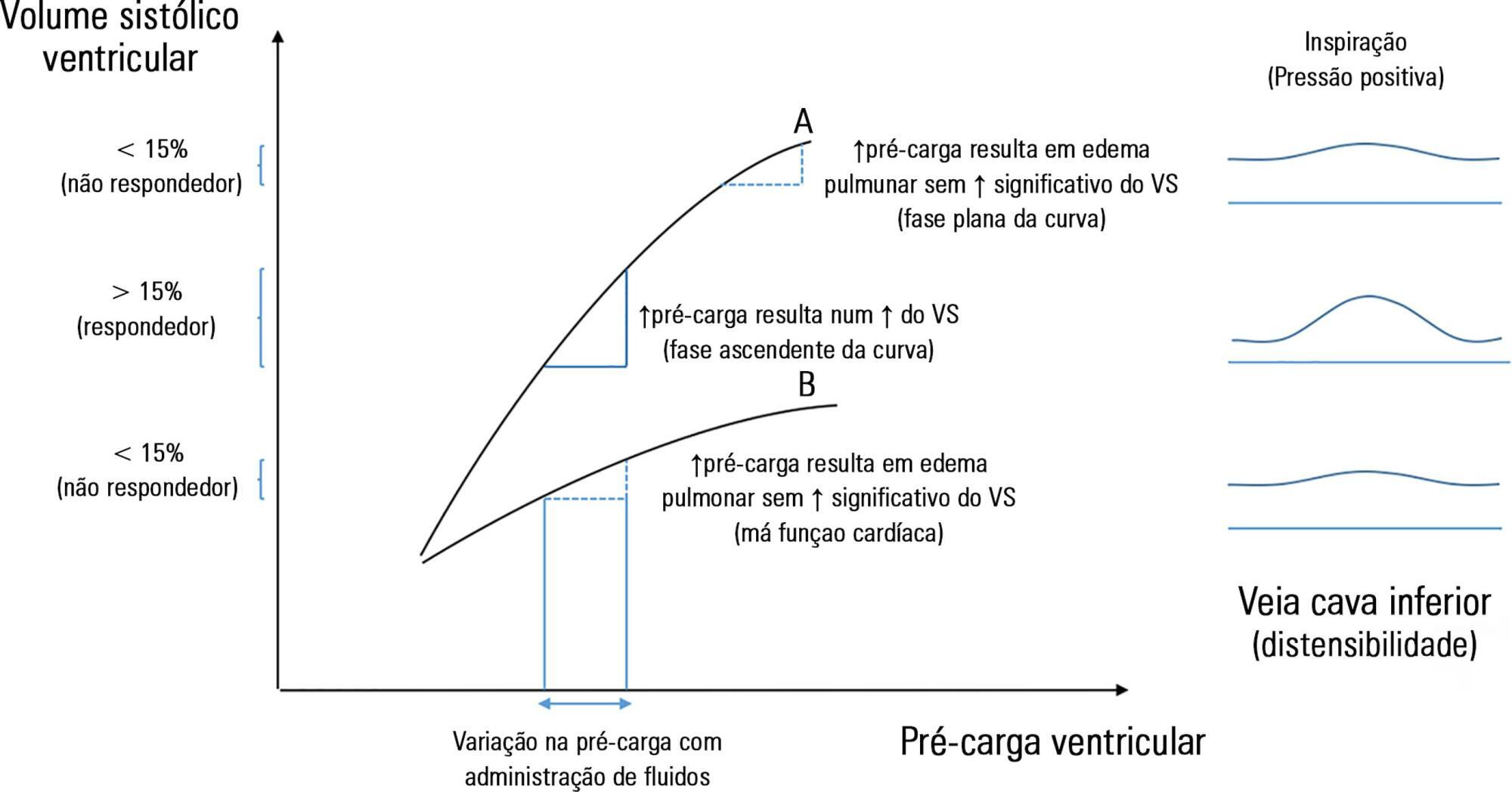
The fluid resuscitation of patients with acute circulatory failure aims to increase systolic volume and consequently improve cardiac output for better tissue oxygenation. However, this effect does not always occur because approximately half of patients do not respond to fluids. The evaluation of fluid responsiveness before their administration may help to identify patients who would benefit from fluid resuscitation and avoid the risk of fluid overload in the others. The dynamic parameters of fluid responsiveness evaluation are promising predictive factors. Of these, the echocardiographic measurement of the respiratory variation in the inferior vena cava diameter is easy to apply and has been used in the hemodynamic evaluation of intensive care unit patients. However, the applicability of this technique has many limitations, and the present studies are heterogeneous and inconsistent across specific groups of patients. We review the use of the inferior vena cava diameter respiratory variation, measured via transthoracic echocardiography, to decide whether to administer fluids to patients with acute circulatory failure in the intensive care unit. We explore the benefits and limitations of this technique, its current use, and the existing evidence.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):262-265
DOI 10.5935/0103-507X.20190034
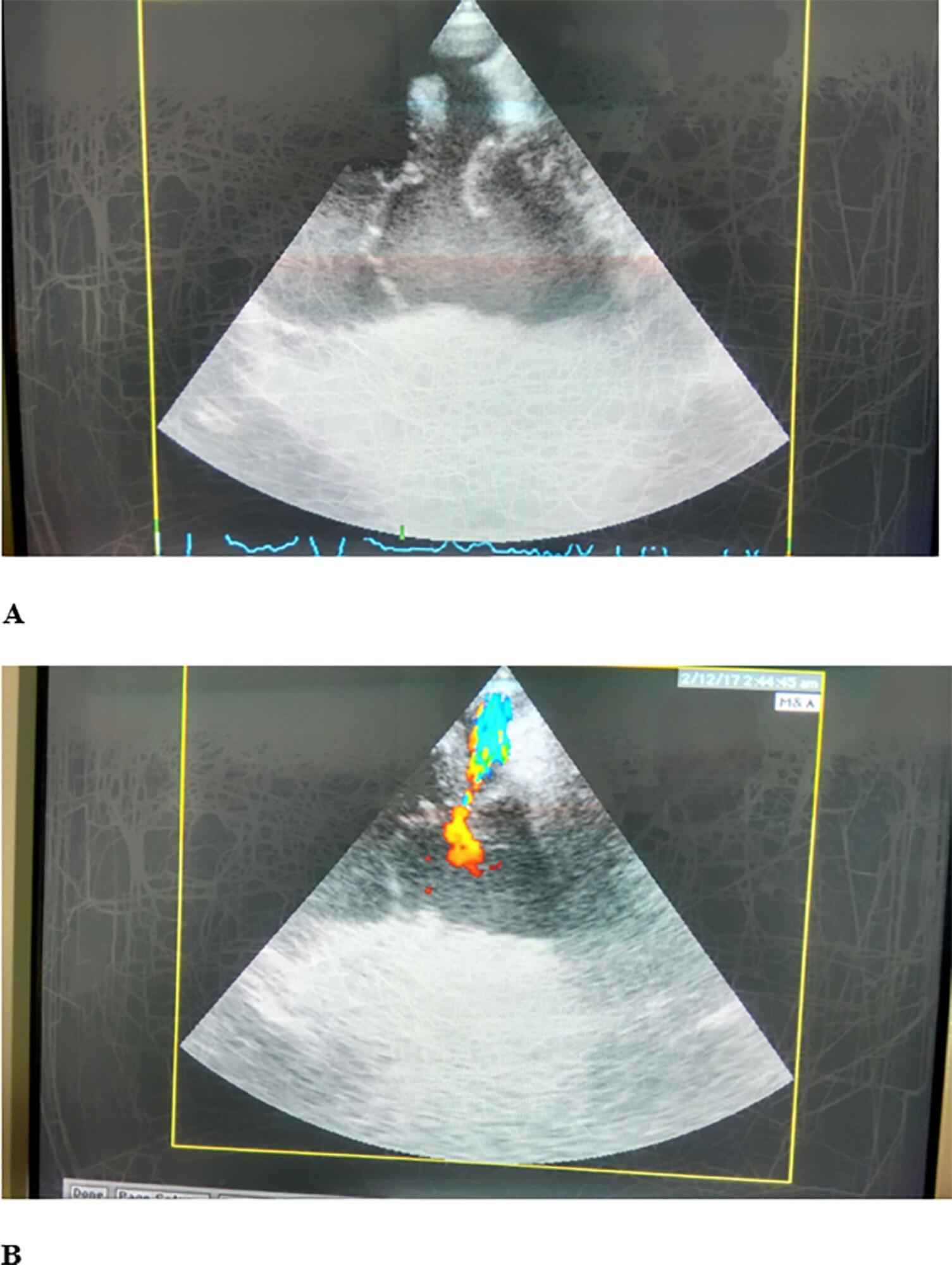
Cardiac trauma often occurs in motor vehicle accidents. A 50-year-old female driver was transported to our hospital with multiple trauma after a high-speed car accident. After admission to the intensive care unit, cardiac ultrasound examination revealed traumatic tricuspid valve papillary muscle rupture and patent foramen ovale, while Lancisi's sign was noted on physical examination. Surgical treatment was performed with valve annuloplasty and closure of the patent foramen ovale and a covert right atrial defect that was detected intraoperatively.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):460-470
DOI 10.5935/0103-507X.20180067
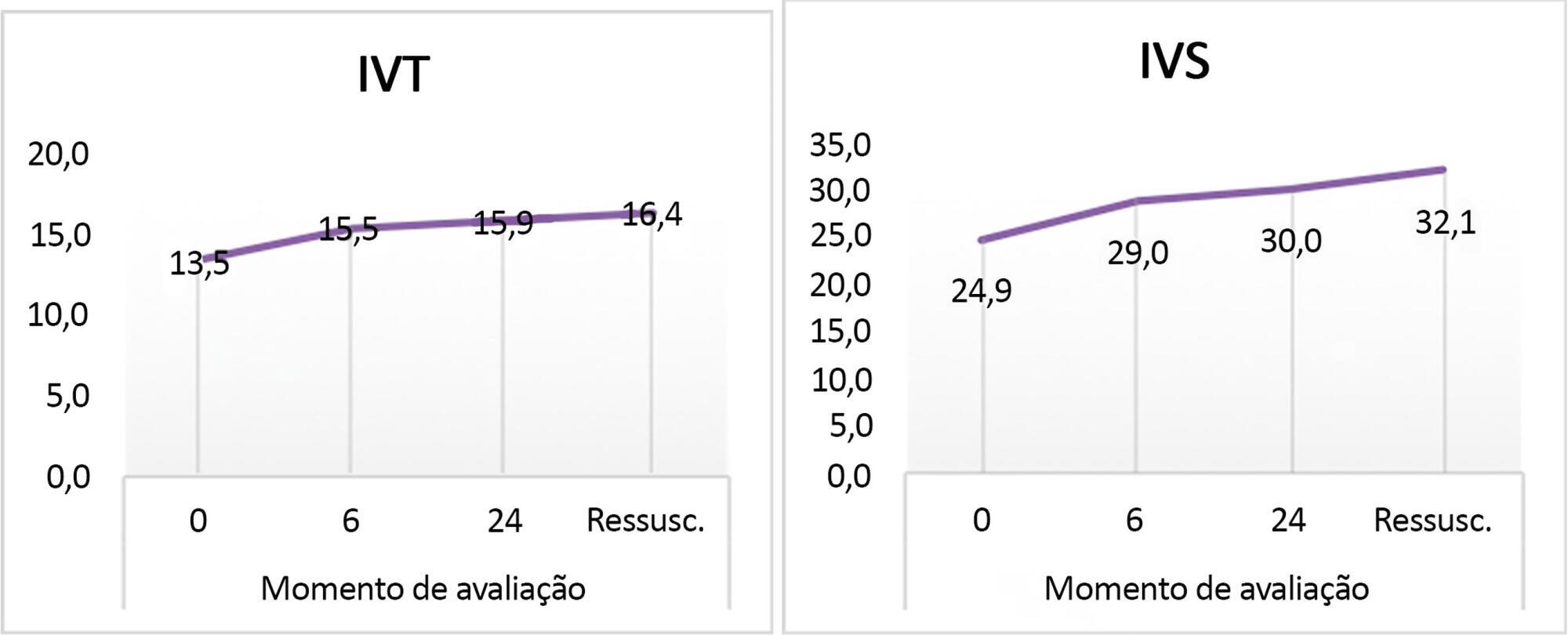
Follow-up of cardiac index and systemic vascular resistance index by bedside echocardiography until resuscitation.
A set of hemodynamic parameters was obtained, including cardiac output, stroke volume, cardiac index, systemic vascular resistance index, velocity time integral, myocardial performance index, capillary refill time, and heart rate at 0 hours after fluid boluses before the start of inotropes, and followed up after 6 hours and 24 hours.
Included were 45 patients with community-acquired septic shock. Septic foci were gastroenteritis (24%), intestinal perforation requiring emergency surgery (24%), pneumonia (20%), central nervous system infection (22%) and soft tissue infection (8%). Klebsiella and Enterobacter were the most frequent isolates. We estimated the factors affecting the cardiac index: high central venous pressure at zero time (r = 0.33, p = 0.024) and persistently high heart rate at hour 6 (r = 0.33, p = 0.03). The systemic vascular resistance index was high in most patients at 0 and 24 hours and at the time of resuscitation and inversely affected the cardiac index as well as affecting the velocity time integral (r = -0.416, -0.61, 0.55 and -0.295). Prolonged capillary refill time was a clinical predictor of the low velocity time integral at 24 hours (r = -0.4). The mortality was 27%. Lower systemic vascular resistance index and higher cardiac output were observed in nonsurviving patients.
There was a persistently high systemic vascular resistance index in cold shock patients that influenced the stroke volume index, cardiac index, and velocity time integral. The use of echocardiograms for hemodynamic measurements is important in pediatric septic shock patients to adjust dilators, and vasopressor doses and achieve resuscitation targets in a timely manner.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)