Abstract
Crit Care Sci. 2023;35(4):386-393
DOI 10.5935/2965-2774.20230190-pt
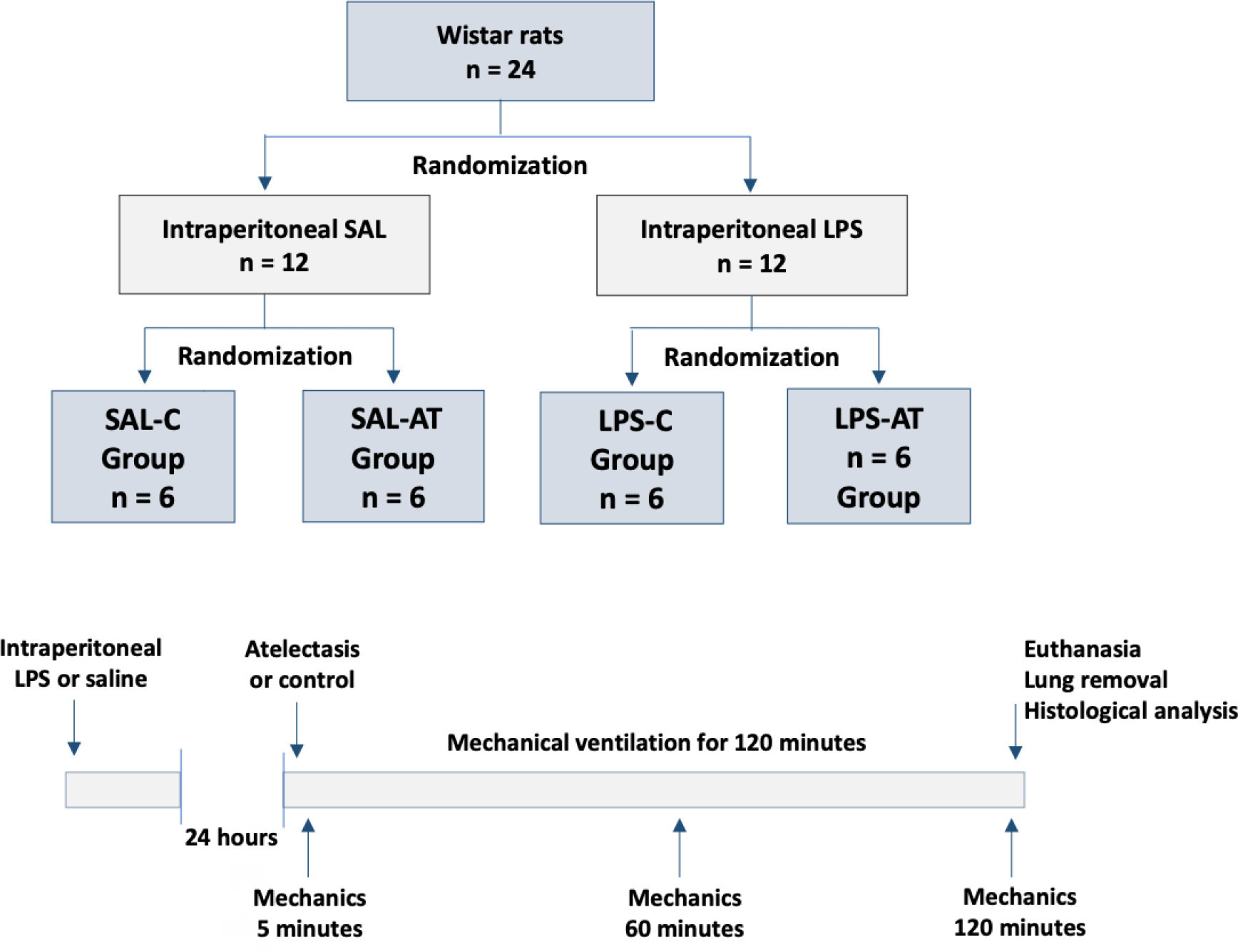
To assess the effect of atelectasis during mechanical ventilation on the periatelectatic and normal lung regions in a model of atelectasis in rats with acute lung injury induced by lipopolysaccharide.
Twenty-four rats were randomized into the following four groups, each with 6 animals: the Saline-Control Group, Lipopolysaccharide Control Group, Saline-Atelectasis Group, and Lipopolysaccharide Atelectasis Group. Acute lung injury was induced by intraperitoneal injection of lipopolysaccharide. After 24 hours, atelectasis was induced by bronchial blocking. The animals underwent mechanical ventilation for two hours with protective parameters, and respiratory mechanics were monitored during this period. Thereafter, histologic analyses of two regions of interest, periatelectatic areas and the normally-aerated lung contralateral to the atelectatic areas, were performed.
The lung injury score was significantly higher in the Lipopolysaccharide Control Group (0.41 ± 0.13) than in the Saline Control Group (0.15 ± 0.51), p < 0.05. Periatelectatic regions showed higher lung injury scores than normally-aerated regions in both the Saline-Atelectasis (0.44 ± 0.06 x 0.27 ± 0.74 p < 0.05) and Lipopolysaccharide Atelectasis (0.56 ± 0.09 x 0.35 ± 0.04 p < 0.05) Groups. The lung injury score in the periatelectatic regions was higher in the Lipopolysaccharide Atelectasis Group (0.56 ± 0.09) than in the periatelectatic region of the Saline-Atelectasis Group (0.44 ± 0.06), p < 0.05.
Atelectasis may cause injury to the surrounding tissue after a period of mechanical ventilation with protective parameters. Its effect was more significant in previously injured lungs.
Abstract
Crit Care Sci. 2023;35(2):177-186
DOI 10.5935/2965-2774.20230348-pt
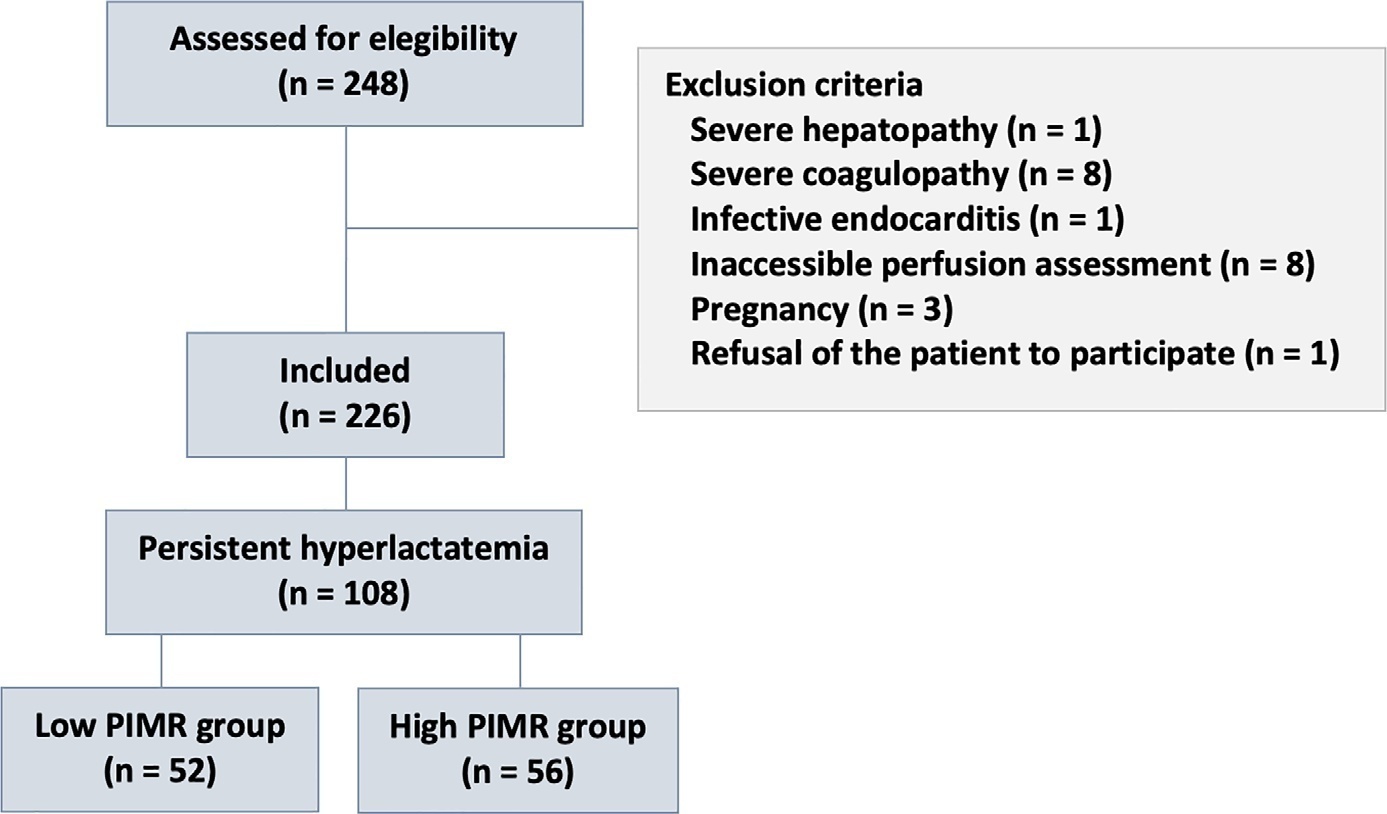
To measure the prognostic value of peripheral ischemic microvascular reserve in the context of persistent sepsis-induced hyperlactatemia and measure its influence on the temporal dynamics of lactate and the strength of association between these variables.
This post hoc analysis of the peripheral perfusion index/postocclusive reactive hyperemia trial, an observational cohort study that enrolled patients with sepsis who persisted with lactate levels ≥ 2mmol/L after fluid resuscitation (with or without shock). Peripheral ischemic microvascular reserve was evaluated using the association of the peripheral perfusion index and postocclusive reactive hyperemia techniques. The cutoff point of ∆ peripheral perfusion index peak values (%) defined the groups with low (≤ 62%) and high peripheral ischemic microvascular reserve (> 62%).
A total of 108 consecutive patients with persistent sepsis-induced hyperlactatemia were studied. The high peripheral ischemic microvascular reserve group showed higher 28-day mortality than the low peripheral ischemic microvascular reserve group (p < 0.01). The temporal dynamics of lactate within the first 48 hours showed a rapid decrease in lactate levels in the low peripheral ischemic microvascular reserve group (p < 0.01). However, this result was not reproduced in the linear mixed effects model. A weak correlation between peripheral ischemic microvascular reserve (%) and lactate level (mmol/L) was observed within the first 24 hours (r = 0.23; p < 0.05).
The prognostic value of high peripheral ischemic microvascular reserve was confirmed in the context of persistent sepsis-induced hyperlactatemia. Although there was a weak positive correlation between peripheral ischemic microvascular reserve value and lactate level within the first 24 hours of sepsis diagnosis, the low peripheral ischemic microvascular reserve group appeared to have a faster decrease in lactate over the 48 hours of follow-up.
Abstract
Crit Care Sci. 2023;35(2):187-195
DOI 10.5935/2965-2774.20230378-pt
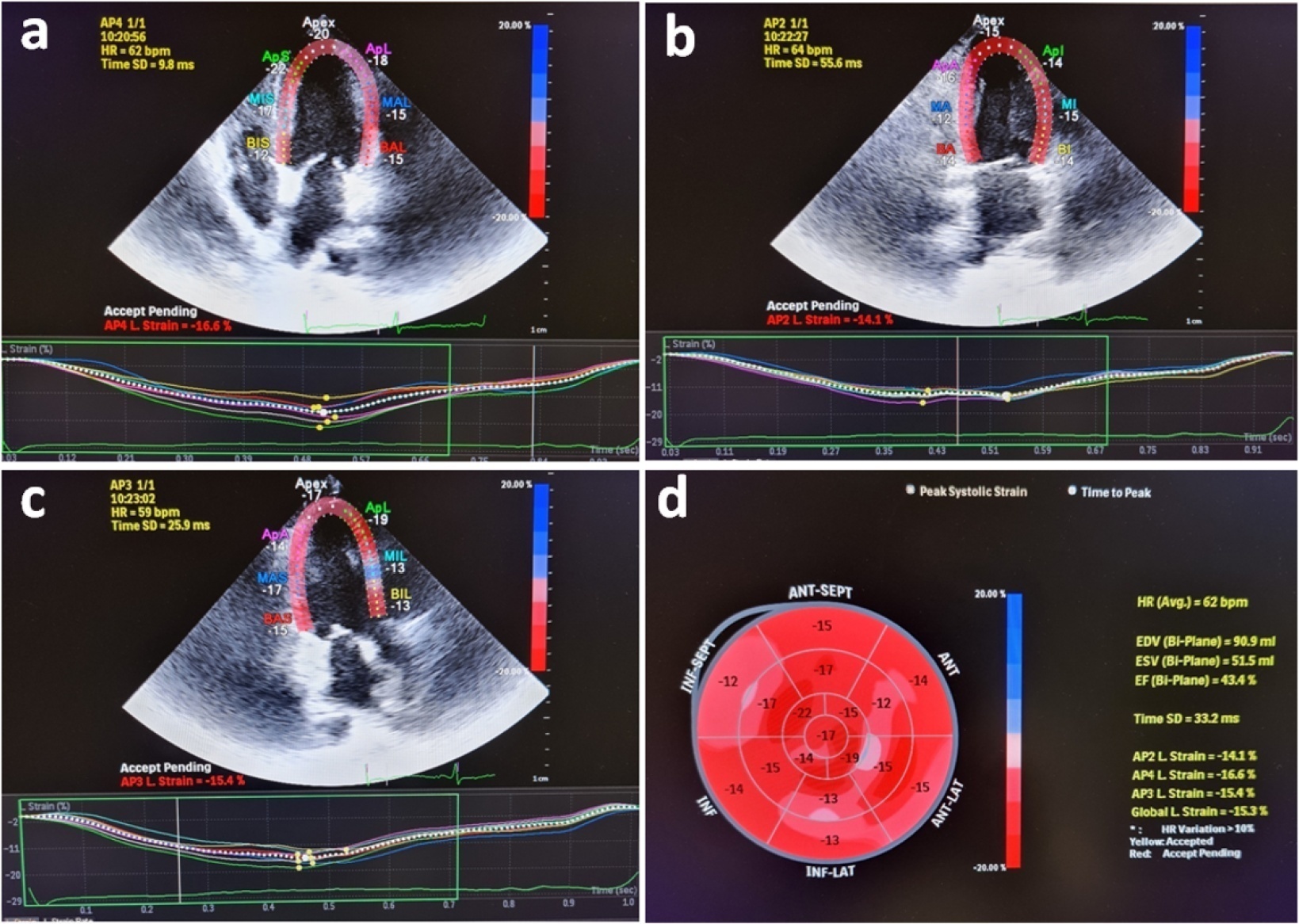
Evaluation of left ventricular systolic function using speckle tracking echocardiography is more sensitive than conventional echocardiographic measurement in detecting subtle left ventricular dysfunction in septic patients. Our purpose was to investigate the predictive significance of left ventricular global longitudinal strain in normotensive septic intensive care patients.
This observational, prospective cohort study included septic normotensive adults admitted to the intensive care unit between June 1, 2021, and August 31, 2021. Left ventricular systolic function was measured using speckle-tracking echocardiography within 24 hours of admission.
One hundred fifty-two patients were enrolled. The intensive care unit mortality rate was 27%. Left ventricular global longitudinal strain was less negative, which indicated worse left ventricular function in non-survivors than survivors (median [interquartile range], -15.2 [-17.2 - -12.5] versus -17.3 [-18.8 - -15.5]; p < 0.001). The optimal cutoff value for left ventricular global longitudinal strain was -17% in predicting intensive care unit mortality (area under the curve, 0.728). Patients with left ventricular global longitudinal strain > -17% (less negative than -17%, which indicated worse left ventricular function) showed a significantly higher mortality rate (39.2% versus 13.7%; p < 0.001). According to multivariate analysis, left ventricular global longitudinal strain was an independent predictor of intensive care unit mortality [OR (95%CI), 1.326 (1.038 - 1.693); p = 0.024], along with invasive mechanical ventilation and Glasgow coma scale, APACHE II, and SOFA risk scores.
Impaired left ventricular global longitudinal strain is associated with mortality and provided predictive data in normotensive septic intensive care patients.
Abstract
Crit Care Sci. 2023;35(2):217-225
DOI 10.5935/2965-2774.20230289-pt
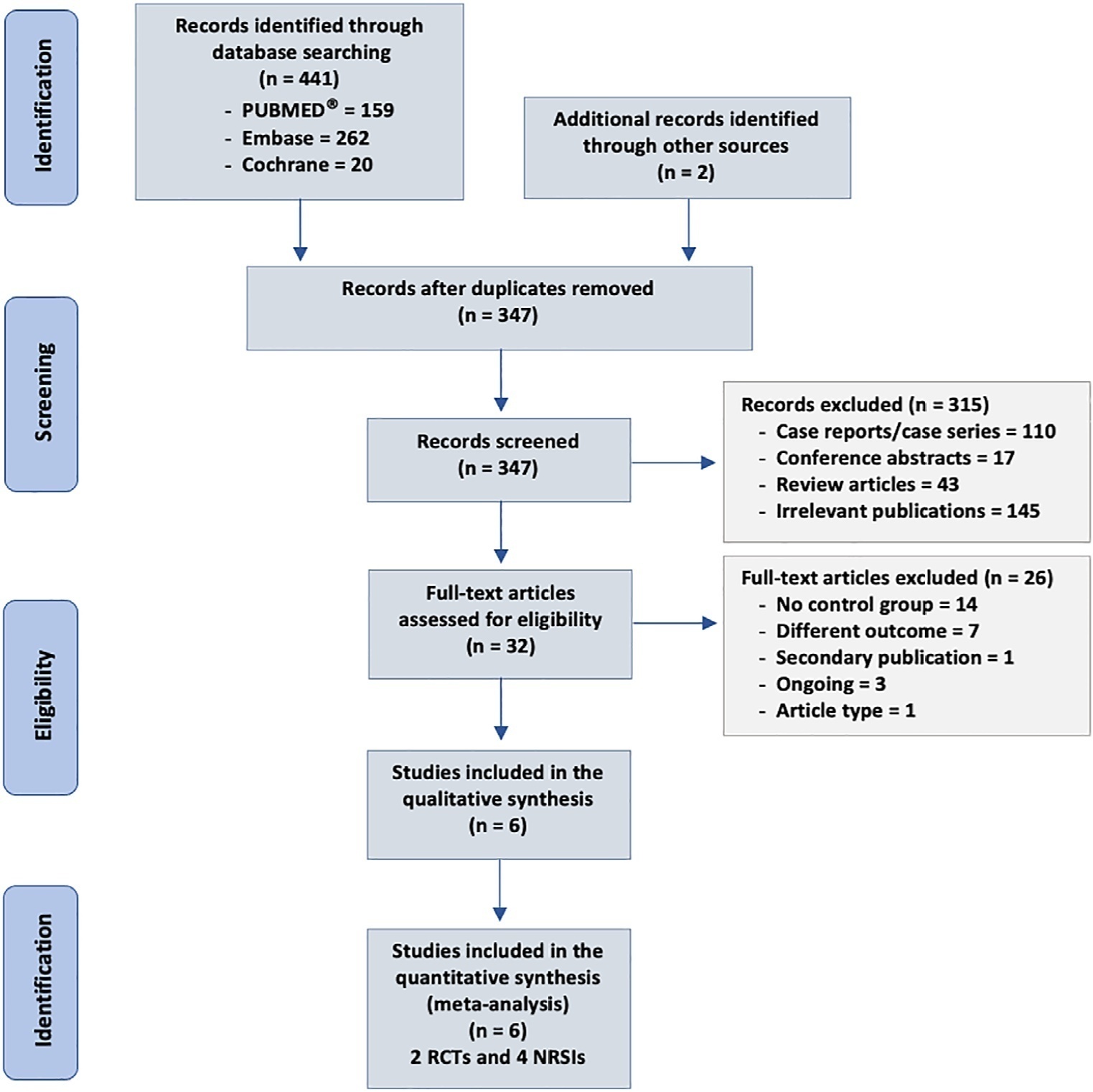
To analyze the effect of CytoSorb® on mortality, interleukin levels, vasopressor use and adverse events in patients with sepsis.
We searched MEDLINE®, Embase and the Cochrane Library for randomized controlled trials and cohort studies that reported the use of CytoSorb® among septic patients. The primary outcome was mortality, and secondary outcomes included the use of vasopressors, levels of inflammatory markers, predicted versus observed mortality, length of stay in the intensive care unit, and adverse events.
We included 6 studies enrolling 413 patients, and assessment for risk of bias indicated variations in study quality from high to moderate. The overall mortality rate was 45%, and no significant effect on mortality was found at 28 - 30 days (RR 0.98 [0.12 - 8.25] for the randomized clinical trial and RR 0.74 [0.49 - 1.13] for cohort studies). We did not perform a metanalysis for other outcomes due to the small number of studies found or the lack of data.
Our study found very low certainty evidence, due to imprecision, risk of bias, and heterogeneity, thereby showing no benefit of CytoSorb® use in terms of mortality at 28 - 30 days. We cannot recommend the use of CytoSorb® in septic or septic shock patients outside clinical trials. Further high-quality randomized trials with a common intervention arm are needed to evaluate the influence of CytoSorb® in this population.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):461-468
DOI 10.5935/0103-507X.20220132-en
To investigate the influence of a passive mobilization session on endothelial function in patients with sepsis.
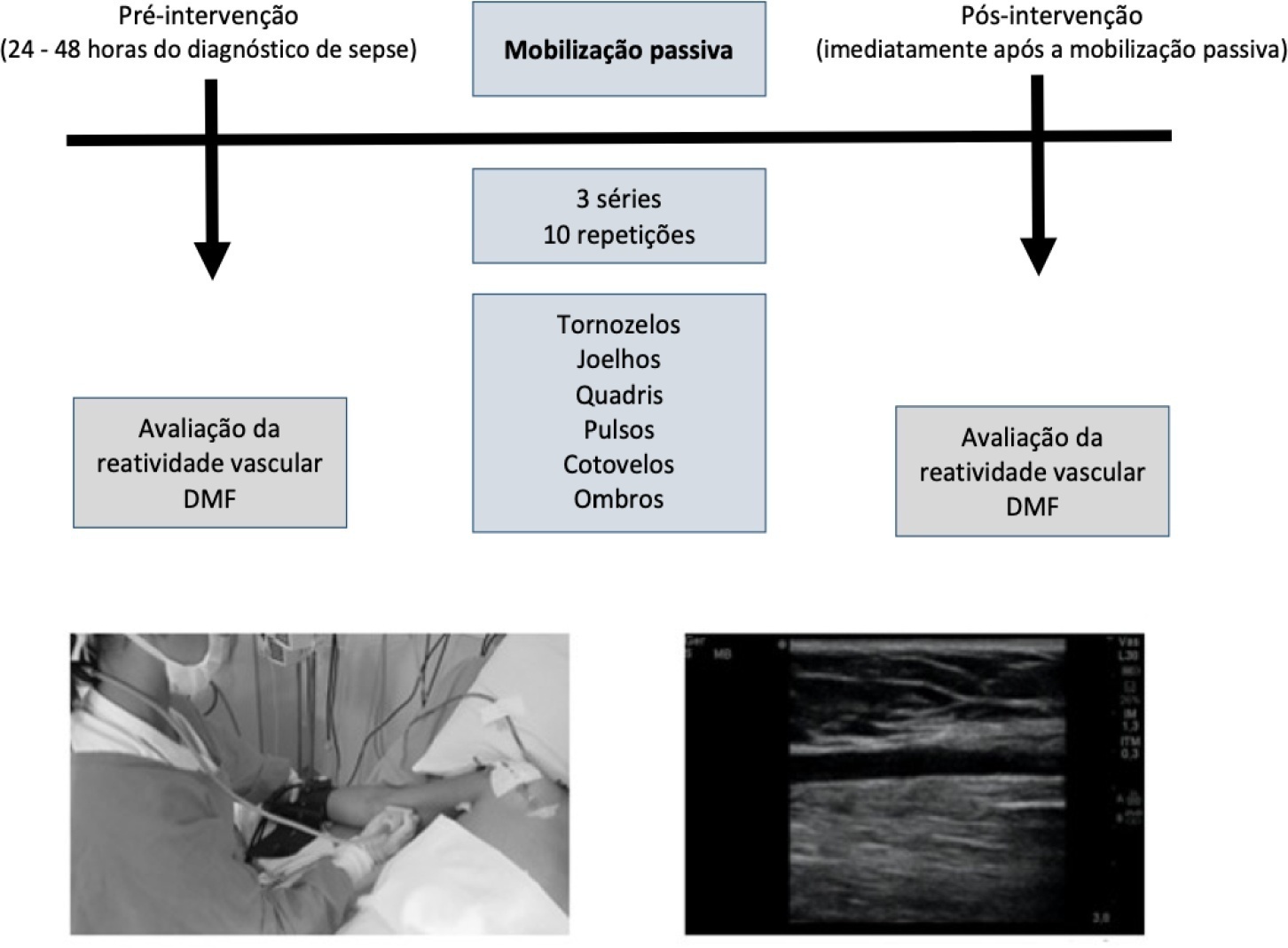
This was a quasi-experimental double-blind and single-arm study with a pre- and postintervention design. Twenty-five patients with a diagnosis of sepsis who were hospitalized in the intensive care unit were included. Endothelial function was assessed at baseline (preintervention) and immediately postintervention by brachial artery ultrasonography. Flow mediated dilatation, peak blood flow velocity and peak shear rate were obtained. Passive mobilization consisted of bilateral mobilization (ankles, knees, hips, wrists, elbows and shoulders), with three sets of ten repetitions each, totaling 15 minutes.
After mobilization, we found increased vascular reactivity function compared to preintervention: absolute flow-mediated dilatation (0.57mm ± 0.22 versus 0.17mm ± 0.31; p < 0.001) and relative flow-mediated dilatation (17.1% ± 8.25 versus 5.08% ± 9.16; p < 0.001). Reactive hyperemia peak flow (71.8cm/s ± 29.3 versus 95.3cm/s ± 32.2; p < 0.001) and shear rate (211s ± 113 versus 288s ± 144; p < 0.001) were also increased.
A passive mobilization session increases endothelial function in critical patients with sepsis. Future studies should investigate whether a mobilization program can be applied as a beneficial intervention for clinical improvement of endothelial function in patients hospitalized due to sepsis.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):367-373
DOI 10.5935/0103-507X.20220102-en
To evaluate the mechanisms attributed to the prognostic value of peripheral ischemic microvascular reserve in patients with sepsis.
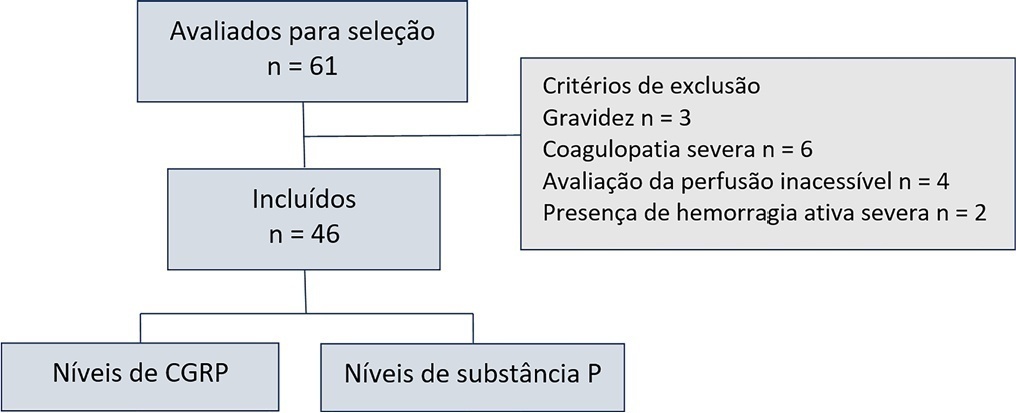
This observational cohort study enrolled 46 consecutive septic patients in the intensive care unit between November 2020 and October 2021. After fluid resuscitation, the peripheral ischemic microvascular reserve was evaluated using the association of postocclusion reactive hyperemia with the peripheral perfusion index. Additionally, peripheral venous blood samples were used to evaluate the neuropeptide calcitonin gene-related peptide and substance P levels in the upper limb before and immediately after postocclusion reactive hyperemia
There was no statistically significant correlation (p > 0.05) between basal values (pg/mL) or variations from neuropeptide levels (%) and the peripheral ischemic microvascular reserve (%).
Although calcitonin gene-related peptide and substance P may have a prognostic role in sepsis, these neuropeptides do not appear to contribute to peripheral ischemic microvascular reserve.
Abstract
Rev Bras Ter Intensiva. 2022;34(1):96-106
DOI 10.5935/0103-507X.20220004-en
Early reversion of sepsis-induced tissue hypoperfusion is essential for survival in septic shock. However, consensus regarding the best initial resuscitation strategy is lacking given that interventions designed for the entire population with septic shock might produce unnecessary fluid administration. This article reports the rationale, study design and analysis plan of the ANDROMEDA-2 study, which aims to determine whether a peripheral perfusion-guided strategy consisting of capillary refill time-targeted resuscitation based on clinical and hemodynamic phenotypes is associated with a decrease in a composite outcome of mortality, time to organ support cessation, and hospital length of stay compared to standard care in patients with early (< 4 hours of diagnosis) septic shock.
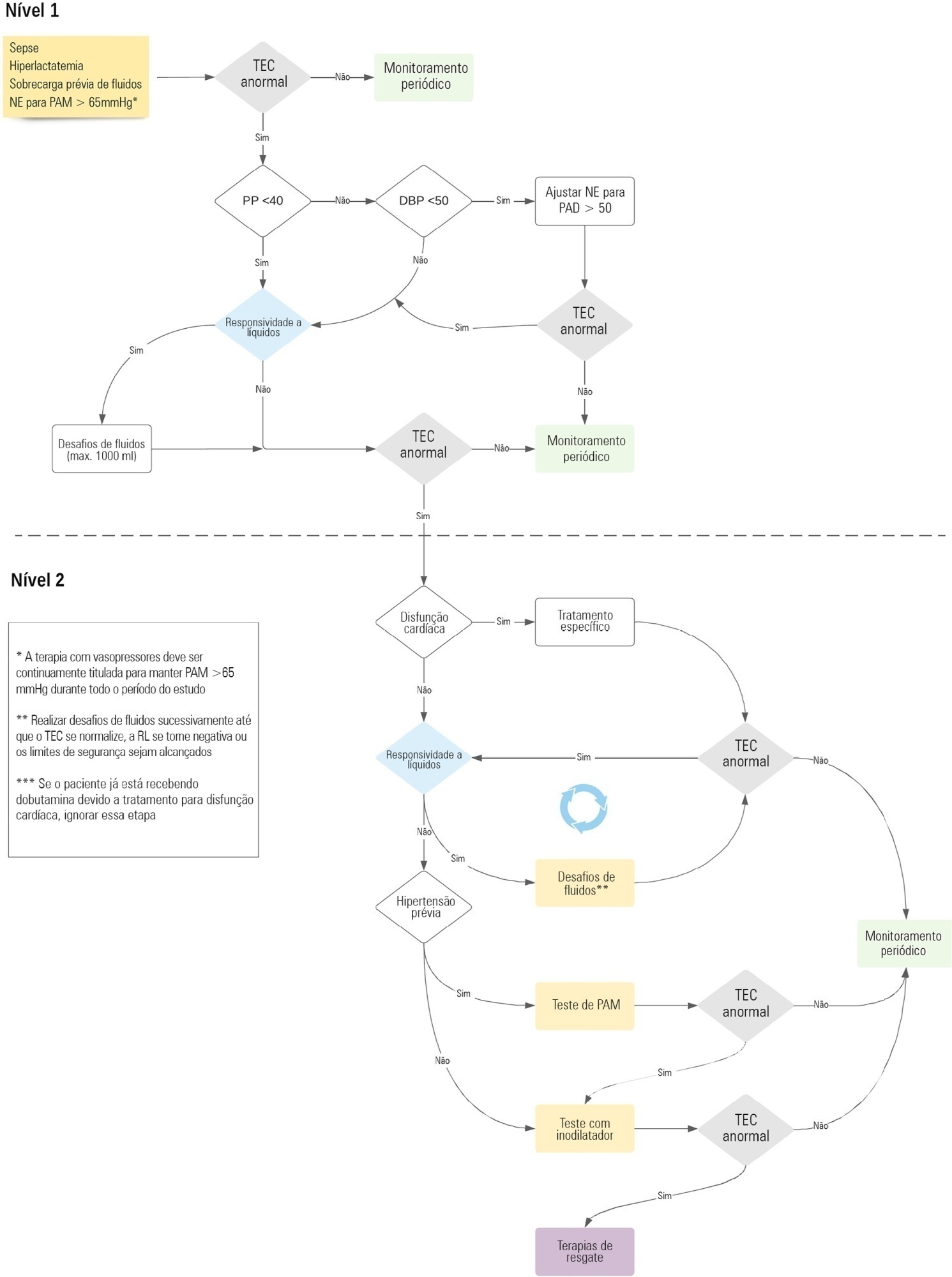
The ANDROMEDA-2 study is a multicenter, multinational randomized controlled trial. In the intervention group, capillary refill time will be measured hourly for 6 hours. If abnormal, patients will enter an algorithm starting with pulse pressure assessment. Patients with pulse pressure less than 40mmHg will be tested for fluid responsiveness and receive fluids accordingly. In patients with pulse pressure > 40mmHg, norepinephrine will be titrated to maintain diastolic arterial pressure > 50mmHg. Patients who fail to normalize capillary refill time after the previous steps will be subjected to critical care echocardiography for cardiac dysfunction evaluation and subsequent management. Finally, vasopressor and inodilator tests will be performed to further optimize perfusion. A sample size of 1,500 patients will provide 88% power to demonstrate superiority of the capillary refill time-targeted strategy.
If hemodynamic phenotype-based, capillary refill time-targeted resuscitation demonstrates to be a superior strategy, care processes in septic shock resuscitation can be optimized with bedside tools.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):549-556
DOI 10.5935/0103-507X.20210083
To analyze the correlation between glycocalyx disruption measured via the serum syndecan-1 level and organ dysfunctions assessed by the PELOD-2 score and to evaluate its association with mortality in pediatric sepsis.
We performed a prospective observational study in a tertiary public hospital. Sixty-eight pediatric patients diagnosed with sepsis according to International Pediatric Sepsis Consensus Conference criteria were consecutively recruited. We performed measurements of day 1 and day 5 serum syndecan-1 levels and PELOD-2 score components. Patients were followed up to 28 days following sepsis diagnosis.
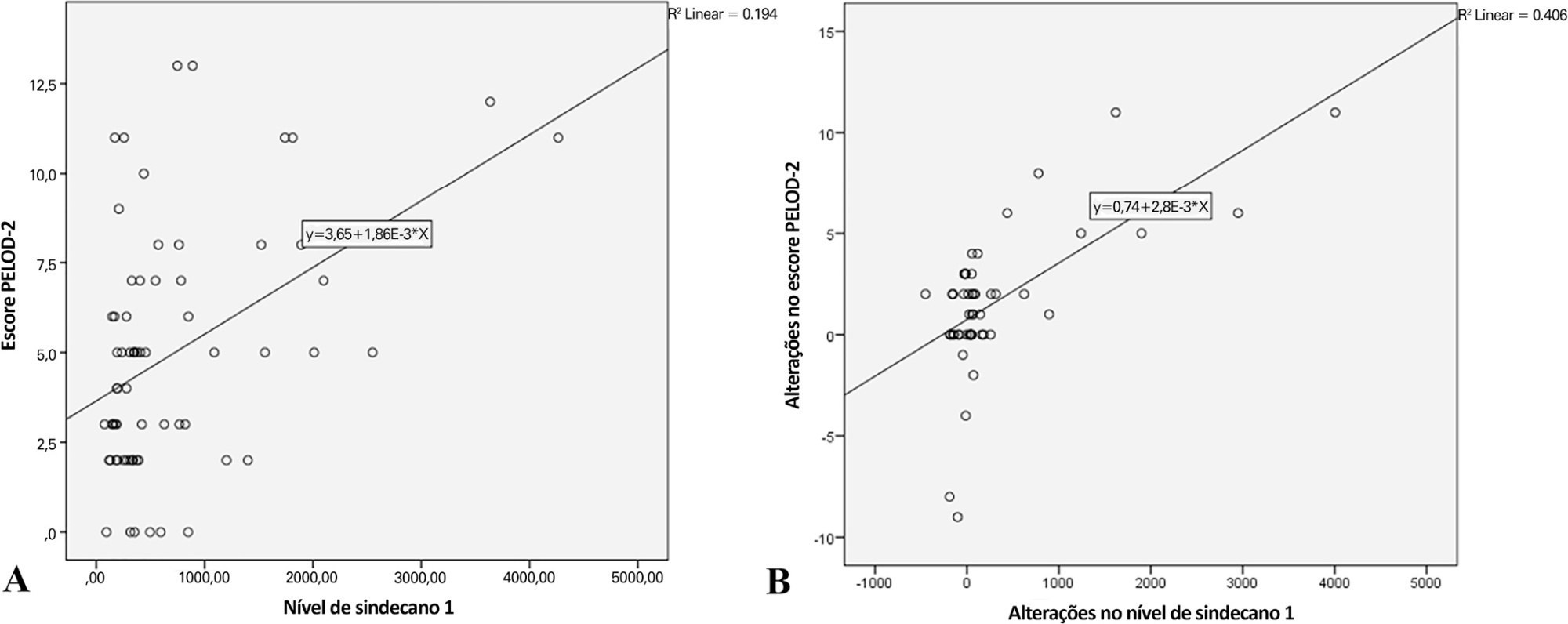
Overall, the syndecan-1 level was increased in all subjects, with a significantly higher level among septic shock patients (p = 0.01). The day 1 syndecan-1 level was positively correlated with the day 1 PELOD-2 score with a correlation coefficient of 0.35 (p = 0.003). Changes in syndecan-1 were positively correlated with changes in the PELOD-2 score, with a correlation coefficient of 0.499 (p < 0.001) during the first five days. Using the cutoff point of day 1 syndecan-1 ≥ 430ng/mL, organ dysfunction (PELOD-2 score of ≥ 8) could be predicted with an AUC of 74.3%, sensitivity of 78.6%, and specificity of 68.5% (p = 0.001).
The day 1 syndecan-1 level was correlated with the day 1 PELOD-2 score but not 28-day mortality. Organ dysfunction (PELOD-2 ≥ 8) could be predicted by the syndecan-1 level in the first 24 hours of sepsis, suggesting its significant pathophysiological involvement in sepsis-associated organ dysfunction.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) ICU (25) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)