Abstract
Rev Bras Ter Intensiva. 2022;34(4):461-468
DOI 10.5935/0103-507X.20220132-en
To investigate the influence of a passive mobilization session on endothelial function in patients with sepsis.
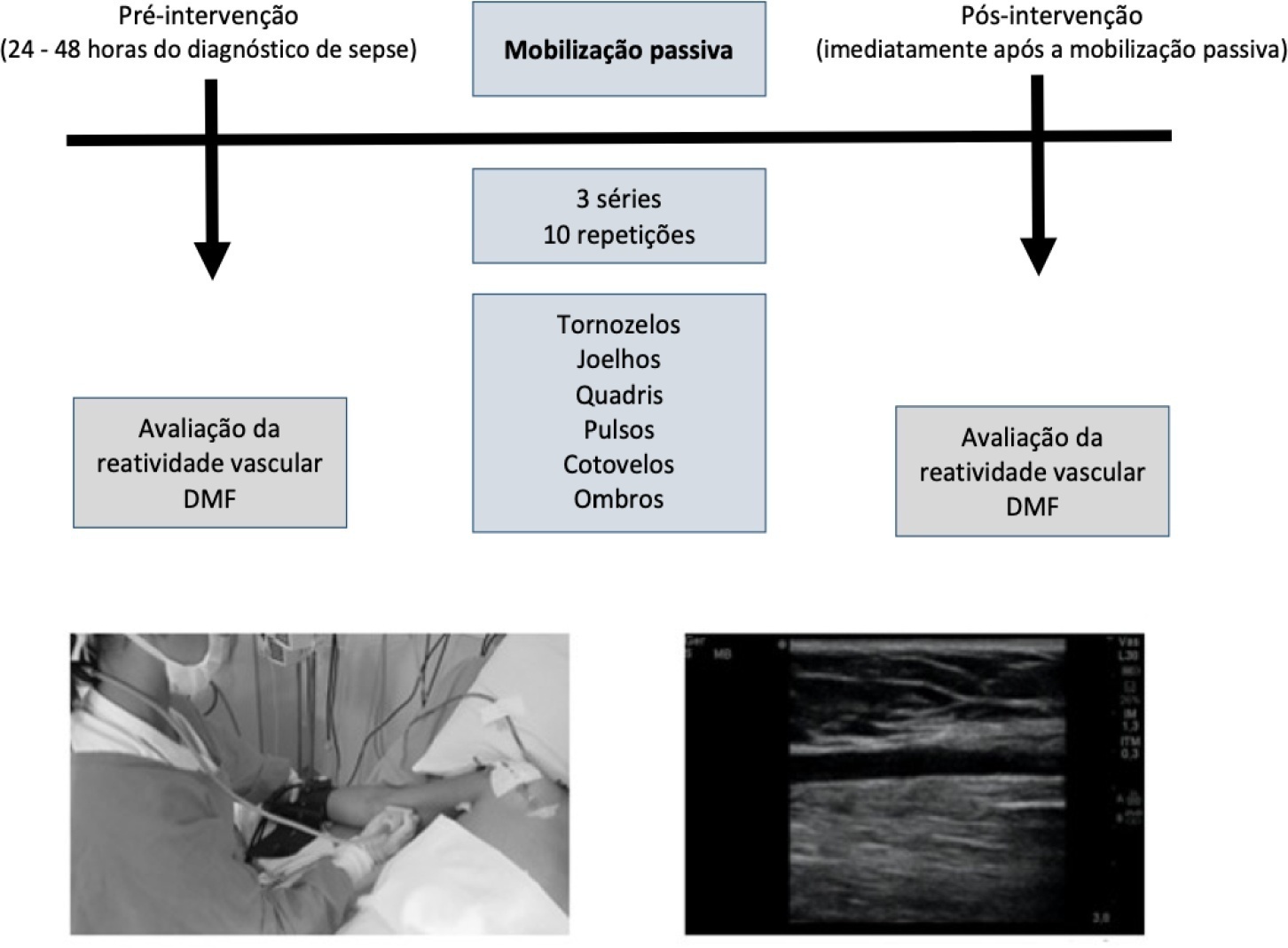
This was a quasi-experimental double-blind and single-arm study with a pre- and postintervention design. Twenty-five patients with a diagnosis of sepsis who were hospitalized in the intensive care unit were included. Endothelial function was assessed at baseline (preintervention) and immediately postintervention by brachial artery ultrasonography. Flow mediated dilatation, peak blood flow velocity and peak shear rate were obtained. Passive mobilization consisted of bilateral mobilization (ankles, knees, hips, wrists, elbows and shoulders), with three sets of ten repetitions each, totaling 15 minutes.
After mobilization, we found increased vascular reactivity function compared to preintervention: absolute flow-mediated dilatation (0.57mm ± 0.22 versus 0.17mm ± 0.31; p < 0.001) and relative flow-mediated dilatation (17.1% ± 8.25 versus 5.08% ± 9.16; p < 0.001). Reactive hyperemia peak flow (71.8cm/s ± 29.3 versus 95.3cm/s ± 32.2; p < 0.001) and shear rate (211s ± 113 versus 288s ± 144; p < 0.001) were also increased.
A passive mobilization session increases endothelial function in critical patients with sepsis. Future studies should investigate whether a mobilization program can be applied as a beneficial intervention for clinical improvement of endothelial function in patients hospitalized due to sepsis.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):565-571
DOI 10.5935/0103-507X.20210073
To identify the factors associated with functional status decline in intensive care unit patients.
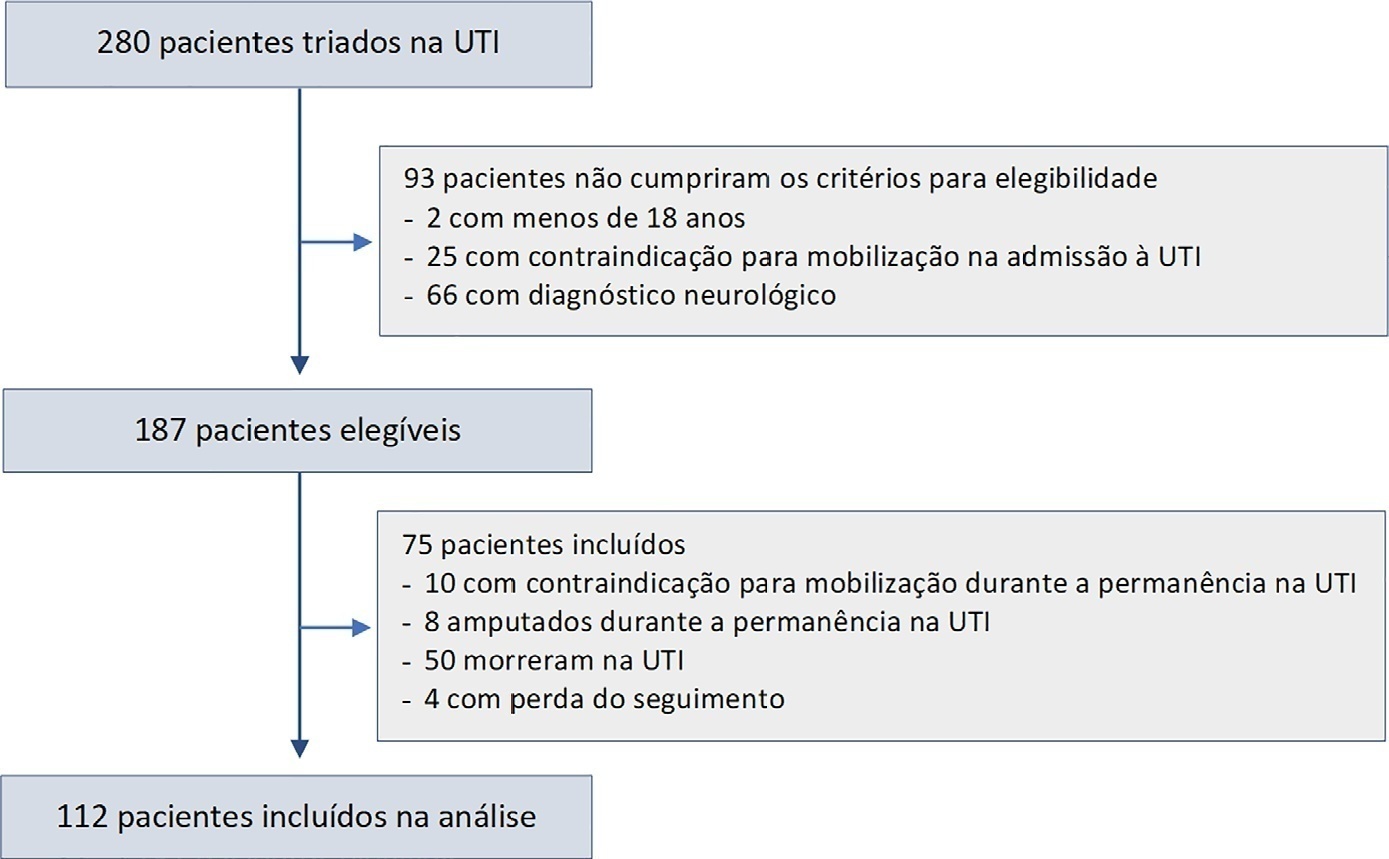
In this prospective study, patients in an intensive care unit aged 18 years or older without neurological disease or contraindications to mobilization were included. The exclusion criteria were patients who spent fewer than 4 days in the intensive care unit or died during the study period. Accelerometry was used to assess the physical activity level of patients. We recorded age, SAPS 3, days on mechanical ventilation, drugs used, comorbidities, and functional status after intensive care unit discharge. After intensive care unit discharge, the patients were assigned to a dependent group or an independent group according to their Barthel index. Logistic regression and the odds ratio were used in the analyses.
Sixty-three out of 112 included patients were assigned to the dependent group. The median Charlson comorbidity index was 3 (2 - 4). The mean SAPS 3 score was 53 ± 11. The patients spent 94 ± 4% of the time spent in inactivity and 4.8 ± 3.7% in light activities. The odds ratio showed that age (OR = 1.08; 95%CI 1.04 - 1.13) and time spent in inactivity (OR = 1.38; 95%CI 1.14 - 1.67) were factors associated with functional status decline. Time spent in light activity was associated with a better functional status (OR = 0.73; 95%CI 0.60 - 0.89).
Age and time spent in inactivity during intensive care unit stay are associated with functional status decline. On the other hand, performing light activities seems to preserve the functional status of patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):434-443
DOI 10.5935/0103-507X.20190084
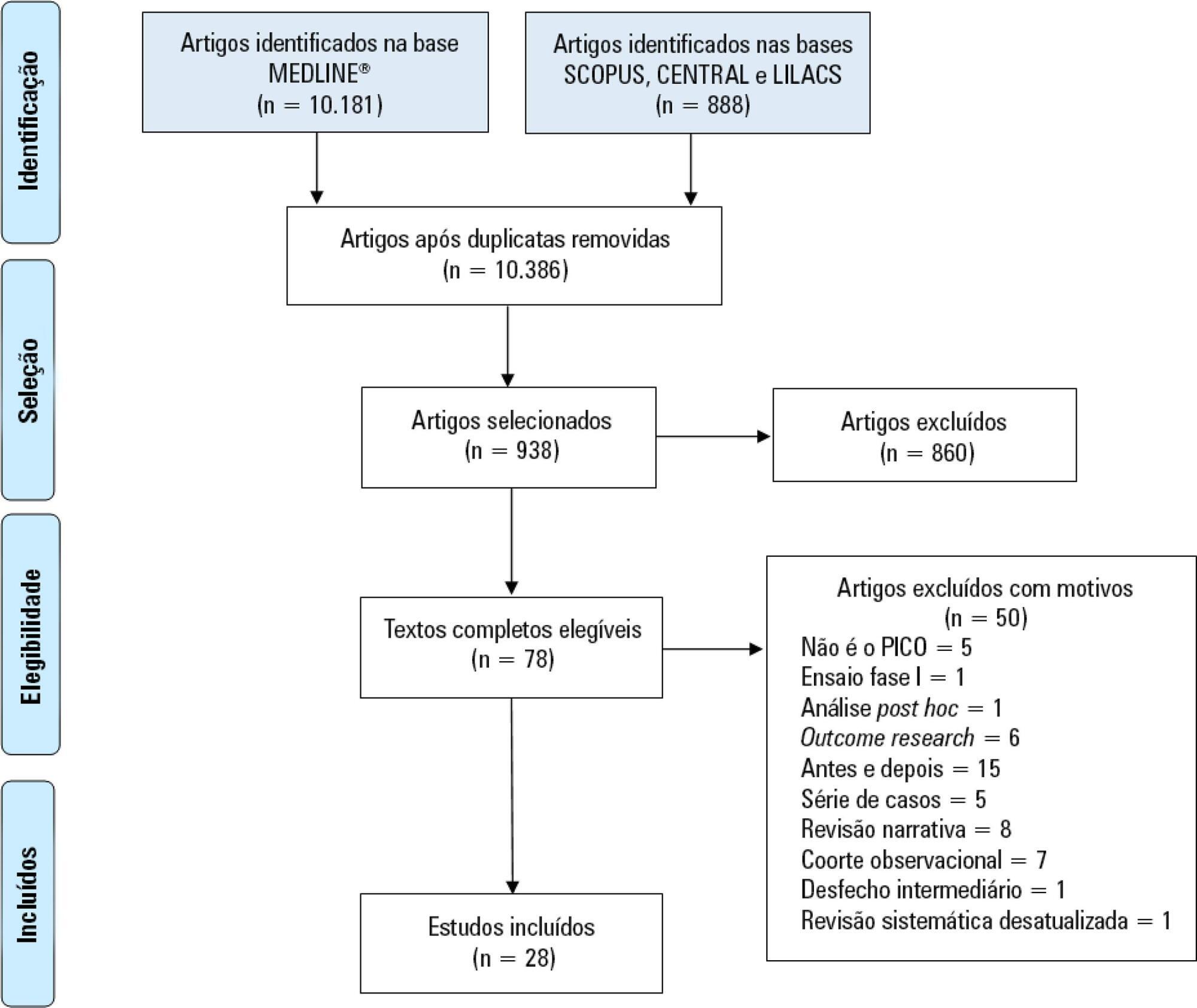
Immobility can cause several complications, including skeletal muscle atrophy and weakness, that influence the recovery of critically ill patients. This effect can be mitigated by early mobilization. Six key questions guided this research: Is early mobilization safe? Which patients are candidates for early mobilization? What are the contraindications? What is the appropriate dose, and how should it be defined? What results are obtained? What are the prognostic indicators for the use of early mobilization? The objective of this guideline was to produce a document that would provide evidence-based recommendations and suggestions regarding the early mobilization of critically ill adult patients, with the aim of improving understanding of the topic and making a positive impact on patient care. This guideline was based on a systematic review of articles conducted using the PICO search strategy, as recommended by the Guidelines Project of the Associação Médica Brasileira. Randomized clinical trials, prognostic cohort studies, and systematic reviews with or without meta-analysis were selected, and the evidence was classified according to the Oxford Center for Evidence-based Medicine Levels of Evidence. For all the questions addressed, enough evidence was found to support safe and well-defined early mobilization, with prognostic indicators that support and recommend the technique. Early mobilization is associated with better functional outcomes and should be performed whenever indicated. Early mobilization is safe and should be the goal of the entire multidisciplinary team.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):529-535
DOI 10.5935/0103-507X.20190066
To measure and compare the functionality of patients after discharge from the intensive care unit and at the time of hospital discharge.
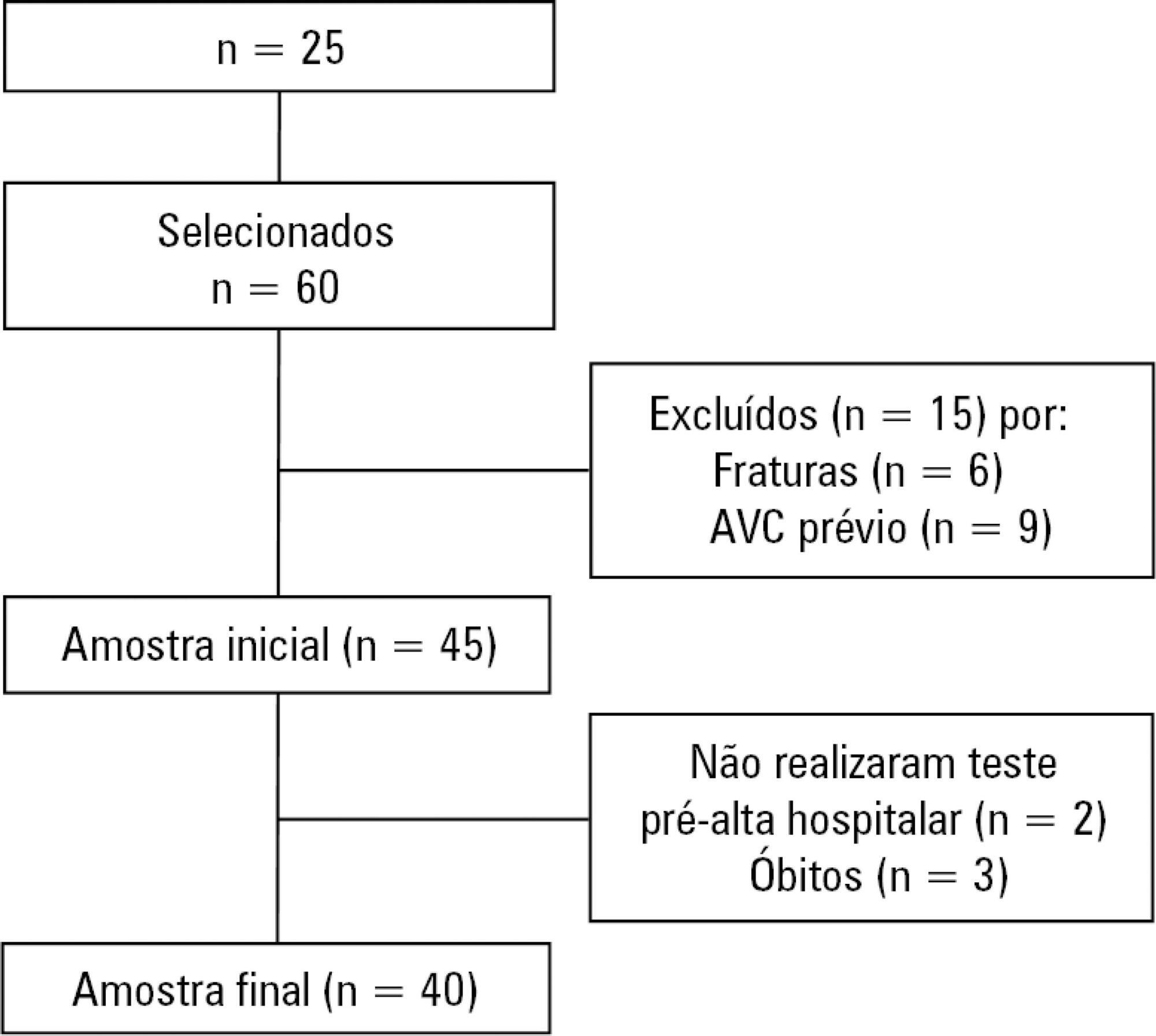
Quantitative study of a prospective cohort performed between August of 2016 and December of 2017 at a university hospital. A 10-meter walk test was performed at 2 timepoints: after discharge from the intensive care unit and prior to hospital discharge. The data were analyzed using Student's t-test and Pearson or Spearman correlation. Statistical Package for Social Science (SPSS) version 21.0 was used for the analysis, and p ≤ 0.05 was adopted as the level of significance.
Forty patients, with a mean age of 57.1 ± 12.2 years and with a predominance of males (60%), were evaluated. For the post-intensive care unit test, a mean speed of 0.48m/s was observed, and for the pre-hospital discharge test, there was an increase to 0.71m/s, evidencing functional evolution during the hospital stay (p < 0.001).
There was significant improvement in walking speed at the time of hospital discharge when compared to the walking speed at the time of intensive care unit discharge.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):161-169
DOI 10.5935/0103-507X.20150028
Evaluation of the functional outcomes of patients undergoing an early rehabilitation protocol for critically ill patients from admission to discharge from the intensive care unit.
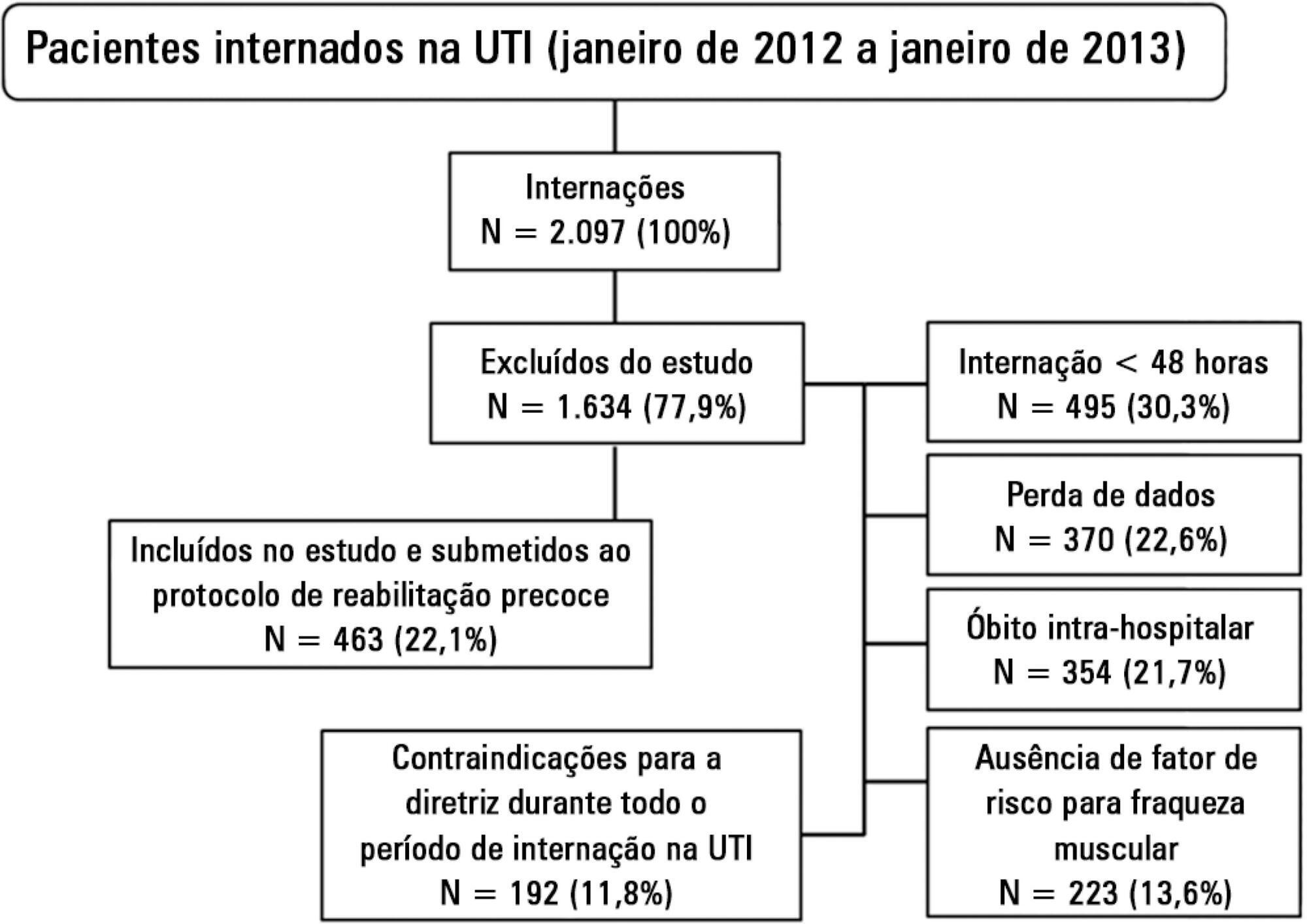
A retrospective cross-sectional study was conducted that included 463 adult patients with clinical and/or surgical diagnosis undergoing an early rehabilitation protocol. The overall muscle strength was evaluated at admission to the intensive care unit using the Medical Research Council scale. Patients were allocated to one of four intervention plans according to the Medical Research Council score, the suitability of the plan’s parameters, and the increasing scale of the plan expressing improved functional status. Uncooperative patients were allocated to intervention plans based on their functional status. The overall muscle strength and/or functional status were reevaluated upon discharge from the intensive care unit by comparison between the Intervention Plans upon admission (Planinitial) and discharge (Planfinal). Patients were classified into three groups according to the improvement of their functional status or not: responsive 1 (Planfinal > Planinitial), responsive 2 (Planfinal = Planinitial) and unresponsive (Planfinal < Planinitial).
In total, 432 (93.3%) of 463 patients undergoing the protocol responded positively to the intervention strategy, showing maintenance and/or improvement of the initial functional status. Clinical patients classified as unresponsive were older (74.3 ± 15.1 years of age; p = 0.03) and had longer lengths of intensive care unit (11.6 ± 14.2 days; p = 0.047) and hospital (34.5 ± 34.1 days; p = 0.002) stays.
The maintenance and/or improvement of the admission functional status were associated with shorter lengths of intensive care unit and hospital stays. The results suggest that the type of diagnosis, clinical or surgical, fails to define the positive response to an early rehabilitation protocol.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):93-98
DOI 10.5935/0103-507X.20130019
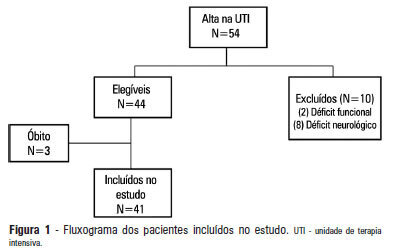
OBJECTIVE: 1) To evaluate the functional independence measures immediately after discharge from an intensive care unit and to compare these values with the FIMs 30 days after that period. 2) To evaluate the possible associated risk factors. METHODS: The present investigation was a prospective cohort study that included individuals who were discharged from the intensive care unit and underwent physiotherapy in the unit. Functional independence was evaluated using the functional independence measure immediately upon discharge from the intensive care unit and 30 days thereafter via a phone call. The patients were admitted to the Hospital Santa Clara intensive care unit during the period from May 2011 to August 2011. RESULTS: During the predetermined period of data collection, 44 patients met the criteria for inclusion in the study. The mean age of the patients was 55.4±10.5 years. Twenty-seven of the subjects were female, and 15 patients were admitted due to pulmonary disease. The patients exhibited an functional independence measure of 84.1±24.2. When this measure was compared to the measure at 30 days after discharge, there was improvement across the functional independence variables except for that concerned with sphincter control. There were no significant differences when comparing the gender, age, clinical diagnosis, length of stay in the intensive care unit, duration of mechanical ventilation, and the presence of sepsis during this period. CONCLUSION: Functional independence, as evaluated by the functional independence measure scale, was improved at 30 days after discharge from the intensive care unit, but it was not possible to define the potentially related factors.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):39-43
DOI 10.1590/S0103-507X2013000100008
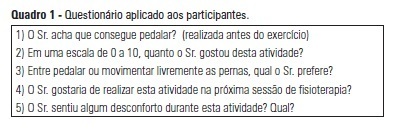
OBJECTIVE: The objective of this study was to use a cycle ergometer to assess cardiorespiratory changes during active exercise and to verify patients' satisfaction with this type of activity. METHODS: A single intervention involving active lower limb exercise was performed with a cycle ergometer (without load) for 5 minutes. The following variables were measured before, during and immediately after exercise: heart rate, blood pressure, respiratory rate, peripheral oxygen saturation and the Borg dyspnea scale score. Following the exercise, the patients answered a questionnaire to evaluate their satisfaction with this type of activity. RESULTS: A total of 38 patients (65% male) with a mean age of 48 ± 16 years old participated in the study. Enrolled patients presented a sequential organ failure assessment (SOFA) score of 2 (0 - 5 scale). During the exercise, 16% of the patients used ventilation support and 55% of them were breathing at room air. A comparison of the initial and final values of the variables indicated increases in the heart rate (92±17 beats/min vs. 95±18 beats/min; p<0.05), the respiratory rate (19 ± 8 breaths/min vs. 23±8 breaths/min; p<0.05) and the Borg dyspnea scale score (1.3±1.8 vs. 2.8±2.2; p<0.05). In addition, 85% of the patients reported enjoying the activity. Only 25% of the patients reported some discomfort, and 100% of the patients wanted to repeat this type of activity in future treatments. CONCLUSION: During the cycle ergometer exercises, minor cardiorespiratory changes were observed in the patients. The evaluated patients reported high satisfaction with this type of activity.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)