Abstract
Crit Care Sci. 2024;36:e20240284en
DOI 10.62675/2965-2774.20240284-en
To examine the physical function and respiratory muscle strength of patients - who recovered from critical COVID-19 – after intensive care unit discharge to the ward on Days one (D1) and seven (D7), and to investigate variables associated with functional impairment.
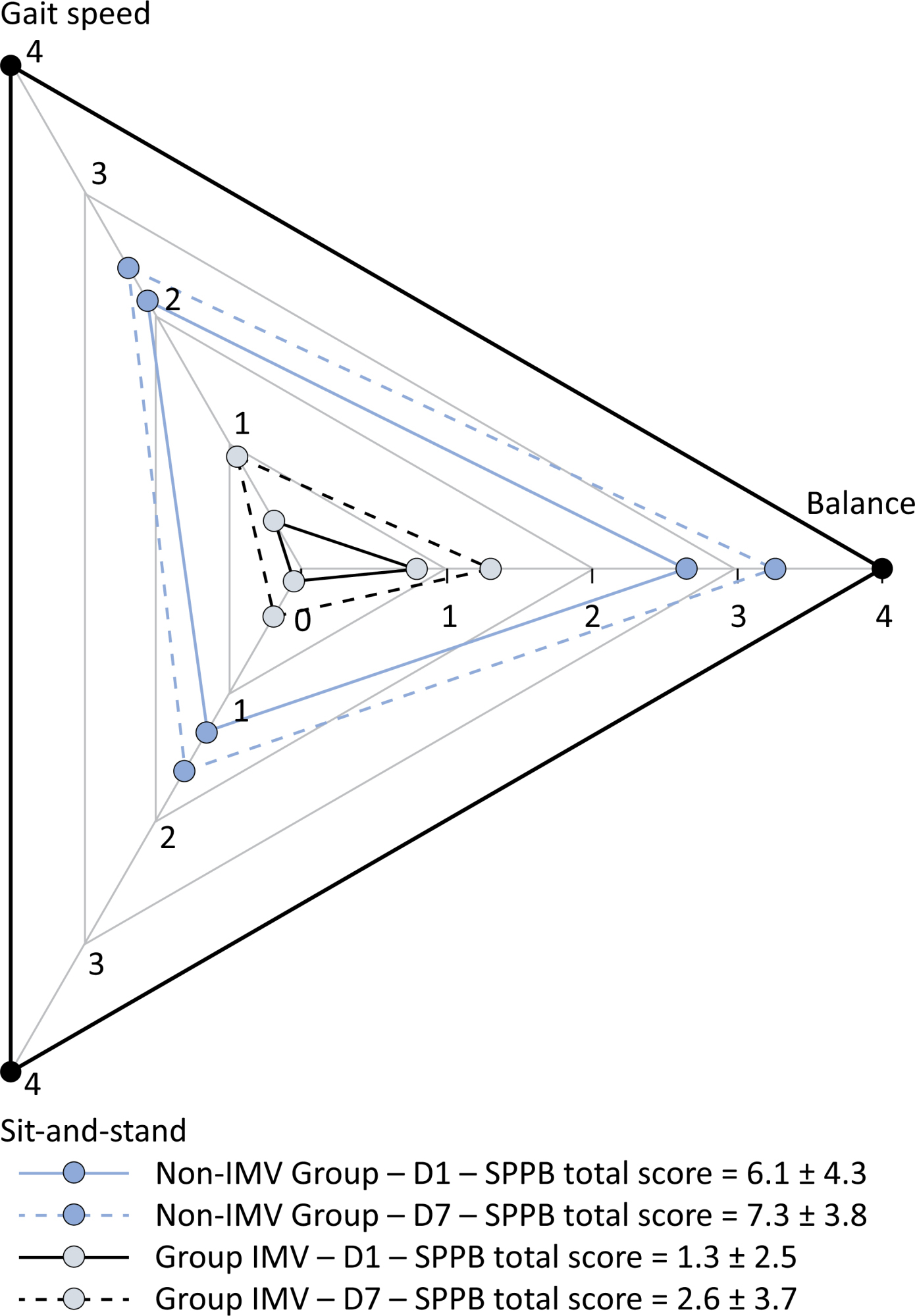
This was a prospective cohort study of adult patients with COVID-19 who needed invasive mechanical ventilation, non-invasive ventilation or high-flow nasal cannula and were discharged from the intensive care unit to the ward. Participants were submitted to Medical Research Council sum-score, handgrip strength, maximal inspiratory pressure, maximal expiratory pressure, and short physical performance battery tests. Participants were grouped into two groups according to their need for invasive ventilation: the Invasive Mechanical Ventilation Group (IMV Group) and the Non-Invasive Mechanical Ventilation Group (Non-IMV Group).
Patients in the IMV Group (n = 31) were younger and had higher Sequential Organ Failure Assessment scores than those in the Non-IMV Group (n = 33). The short physical performance battery scores (range 0 - 12) on D1 and D7 were 6.1 ± 4.3 and 7.3 ± 3.8, respectively for the Non-Invasive Mechanical Ventilation Group, and 1.3 ± 2.5 and 2.6 ± 3.7, respectively for the IMV Group. The prevalence of intensive care unit-acquired weakness on D7 was 13% for the Non-IMV Group and 72% for the IMV Group. The maximal inspiratory pressure, maximal expiratory pressure, and handgrip strength increased on D7 in both groups, but the maximal expiratory pressure and handgrip strength were still weak. Only maximal inspiratory pressure was recovered (i.e., > 80% of the predicted value) in the Non-IMV Group. Female sex, and the need and duration of invasive mechanical were independently and negatively associated with the short physical performance battery score and handgrip strength.
Patients who recovered from critical COVID-19 and who received invasive mechanical ventilation presented greater disability than those who were not invasively ventilated. However, they both showed marginal functional improvement during early recovery, regardless of the need for invasive mechanical ventilation. This might highlight the severity of disability caused by SARS-CoV-2.
Abstract
Crit Care Sci. 2024;36:e20240158en
DOI 10.62675/2965-2774.20240158-pt
To evaluate the association of biomarkers with successful ventilatory weaning in COVID-19 patients.
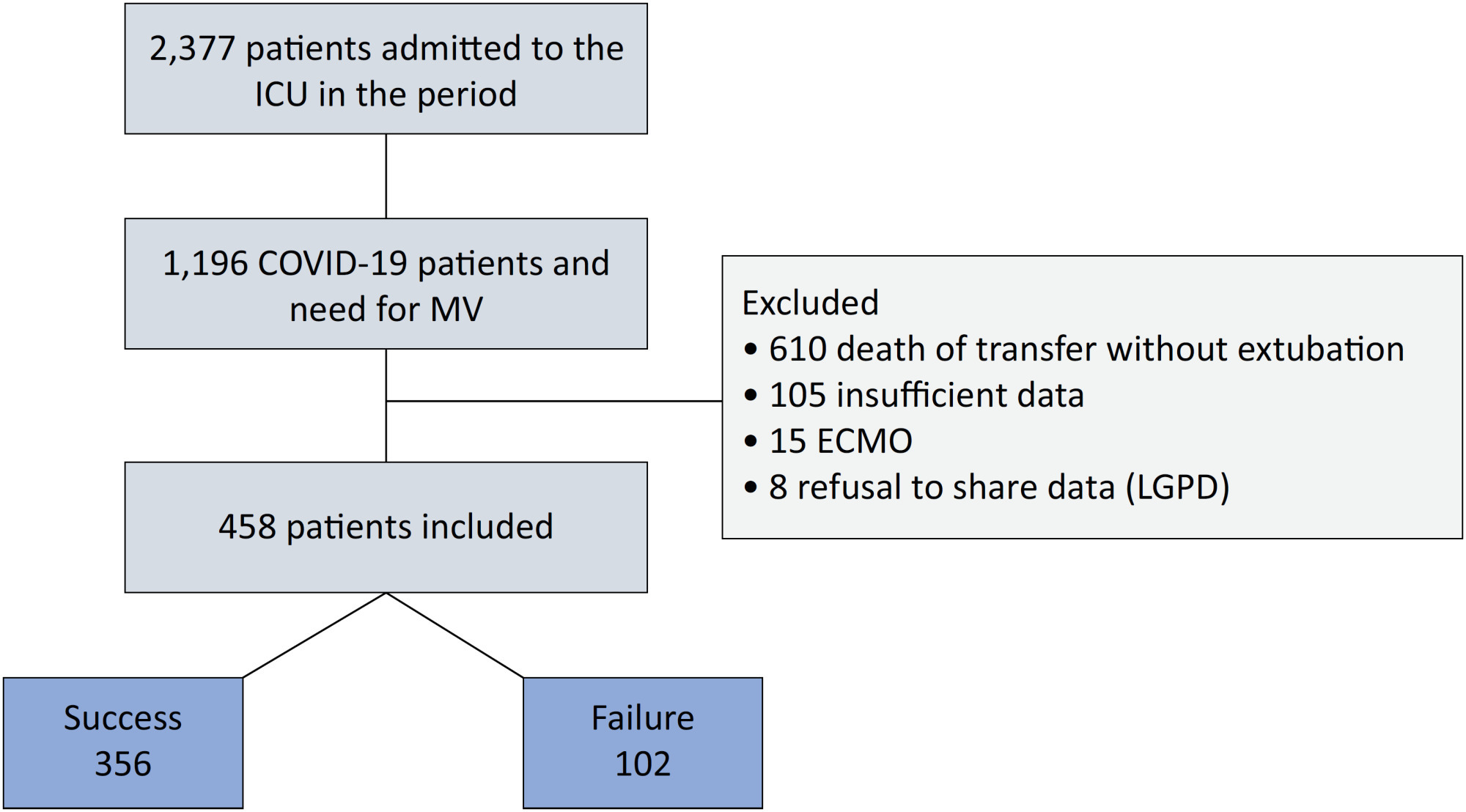
An observational, retrospective, and single-center study was conducted between March 2020 and April 2021. C-reactive protein, total lymphocytes, and the neutrophil/lymphocyte ratio were evaluated during attrition and extubation, and the variation in these biomarker values was measured. The primary outcome was successful extubation. ROC curves were drawn to find the best cutoff points for the biomarkers based on sensitivity and specificity. Statistical analysis was performed using logistic regression.
Of the 2,377 patients admitted to the intensive care unit, 458 were included in the analysis, 356 in the Successful Weaning Group and 102 in the Failure Group. The cutoff points found from the ROC curves were −62.4% for C-reactive protein, +45.7% for total lymphocytes, and −32.9% for neutrophil/lymphocyte ratio. These points were significantly associated with greater extubation success. In the multivariate analysis, only C-reactive protein variation remained statistically significant (OR 2.6; 95%CI 1.51 – 4.5; p < 0.001).
In this study, a decrease in C-reactive protein levels was associated with successful extubation in COVID-19 patients. Total lymphocytes and the neutrophil/lymphocyte ratio did not maintain the association after multivariate analysis. However, a decrease in C-reactive protein levels should not be used as a sole variable to identify COVID-19 patients suitable for weaning; as in our study, the area under the ROC curve demonstrated poor accuracy in discriminating extubation outcomes, with low sensitivity and specificity.
Abstract
Crit Care Sci. 2024;36:e20240176en
DOI 10.62675/2965-2774.20240176-en
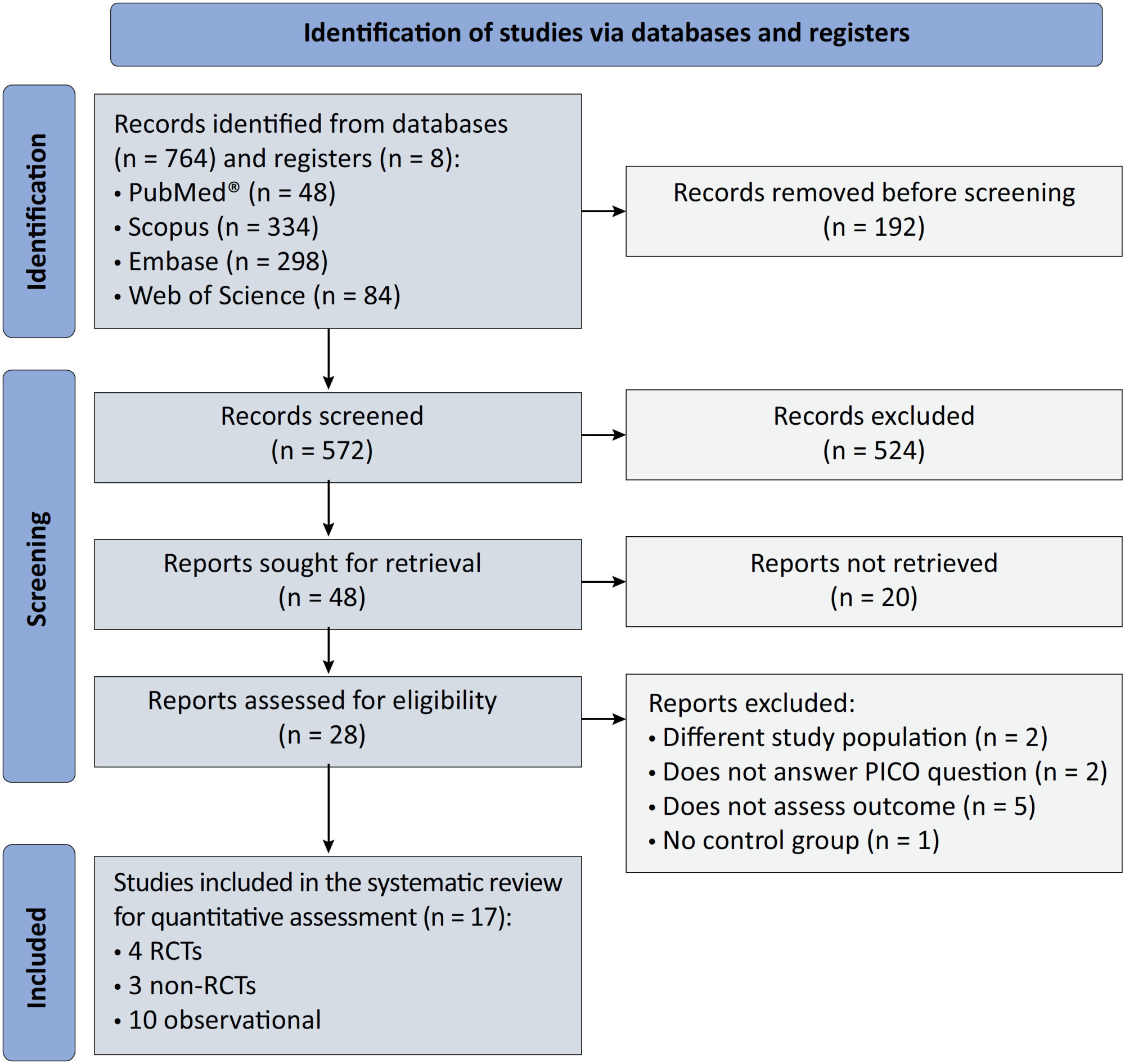
To systematically review the effect of the prone position on endotracheal intubation and mortality in nonintubated COVID-19 patients with acute respiratory distress syndrome.
We registered the protocol (CRD42021286711) and searched for four databases and gray literature from inception to December 31, 2022. We included observational studies and clinical trials. There was no limit by date or the language of publication. We excluded case reports, case series, studies not available in full text, and those studies that included children < 18-years-old.
We included ten observational studies, eight clinical trials, 3,969 patients, 1,120 endotracheal intubation events, and 843 deaths. All of the studies had a low risk of bias (Newcastle-Ottawa Scale and Risk of Bias 2 tools). We found that the conscious prone position decreased the odds of endotracheal intubation by 44% (OR 0.56; 95%CI 0.40 - 0.78) and mortality by 43% (OR 0.57; 95%CI 0.39 - 0.84) in nonintubated COVID-19 patients with acute respiratory distress syndrome. This protective effect on endotracheal intubation and mortality was more robust in those who spent > 8 hours/day in the conscious prone position (OR 0.43; 95%CI 0.26 - 0.72 and OR 0.38; 95%CI 0.24 - 0.60, respectively). The certainty of the evidence according to the GRADE criteria was moderate.
The conscious prone position decreased the odds of endotracheal intubation and mortality, especially when patients spent over 8 hours/day in the conscious prone position and treatment in the intensive care unit. However, our results should be cautiously interpreted due to limitations in evaluating randomized clinical trials, nonrandomized clinical trials and observational studies. However, despite systematic reviews with meta-analyses of randomized clinical trials, we must keep in mind that these studies remain heterogeneous from a clinical and methodological point of view.
Abstract
Crit Care Sci. 2023;35(4):355-366
DOI 10.5935/2965-2774.20230015-pt
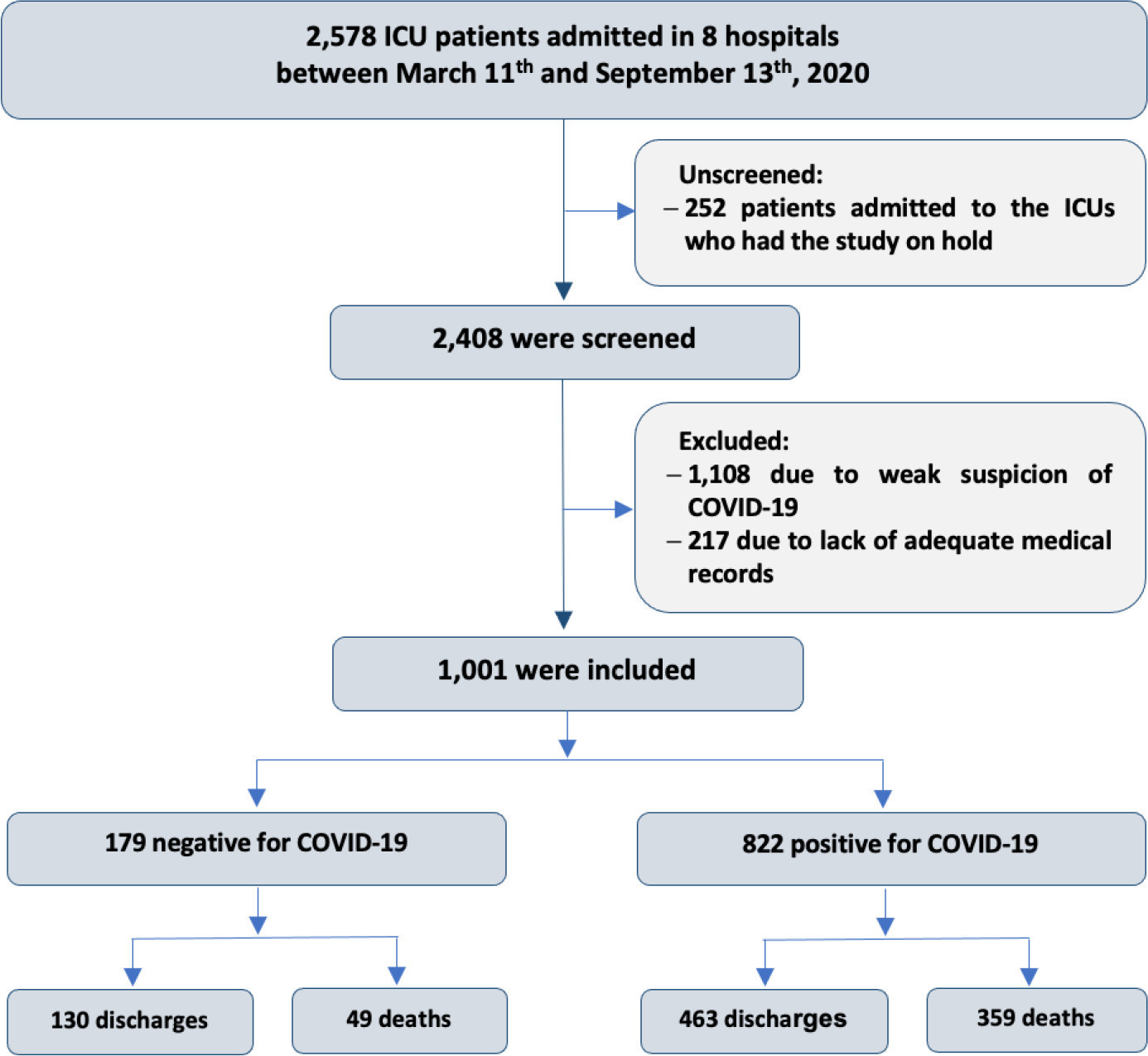
To compare, within a cohort of patients with acute respiratory failure, the phenotypes of patients with and without COVID-19 in the context of the pandemic and evaluate whether COVID-19 is an independent predictor of intensive care unit mortality.
This historical cohort study evaluated 1001 acute respiratory failure patients with suspected COVID-19 admitted to the intensive care unit of 8 hospitals. Patients were classified as COVID-19 cases and non-COVID-19 cases according to real-time polymerase chain reaction results. Data on clinical and demographic characteristics were collected on intensive care unit admission, as well as daily clinical and laboratory data and intensive care unit outcomes.
Although the groups did not differ in terms of APACHE II or SOFA scores at admission, the COVID-19 group had more initial symptoms of fever, myalgia and diarrhea, had a longer duration of symptoms, and had a higher prevalence of obesity. They also had a lower PaO2/FiO2 ratio, lower platelet levels than non-COVID-19 patients, and more metabolic changes, such as higher levels of blood glucose, C-reactive protein, and lactic dehydrogenase. Patients with non-COVID-19 acute respiratory failure had a higher prevalence of chronic obstructive pulmonary disease/asthma and cardiopathy. Patients with COVID-19 stayed in the hospital longer and had more complications, such as acute kidney failure, severe acute respiratory distress syndrome and severe infection. The all-cause mortality rate was also higher in this group (43.7% in the COVID-19 group versus 27.4% in the non-COVID-19 group). The diagnosis of COVID-19 was a predictor of intensive care unit mortality (odds ratio, 2.77; 95%CI, 1.89 - 4.07; p < 0.001), regardless of age or Charlson Comorbidity Index score.
In a prospective cohort of patients admitted with acute respiratory failure, patients with COVID-19 had a clearly different phenotype and a higher mortality than non-COVID-19 patients. This may help to outline more accurate screening and appropriate and timely treatment for these patients.
Abstract
Crit Care Sci. 2023;35(3):243-255
DOI 10.5935/2965-2774.20230136-pt
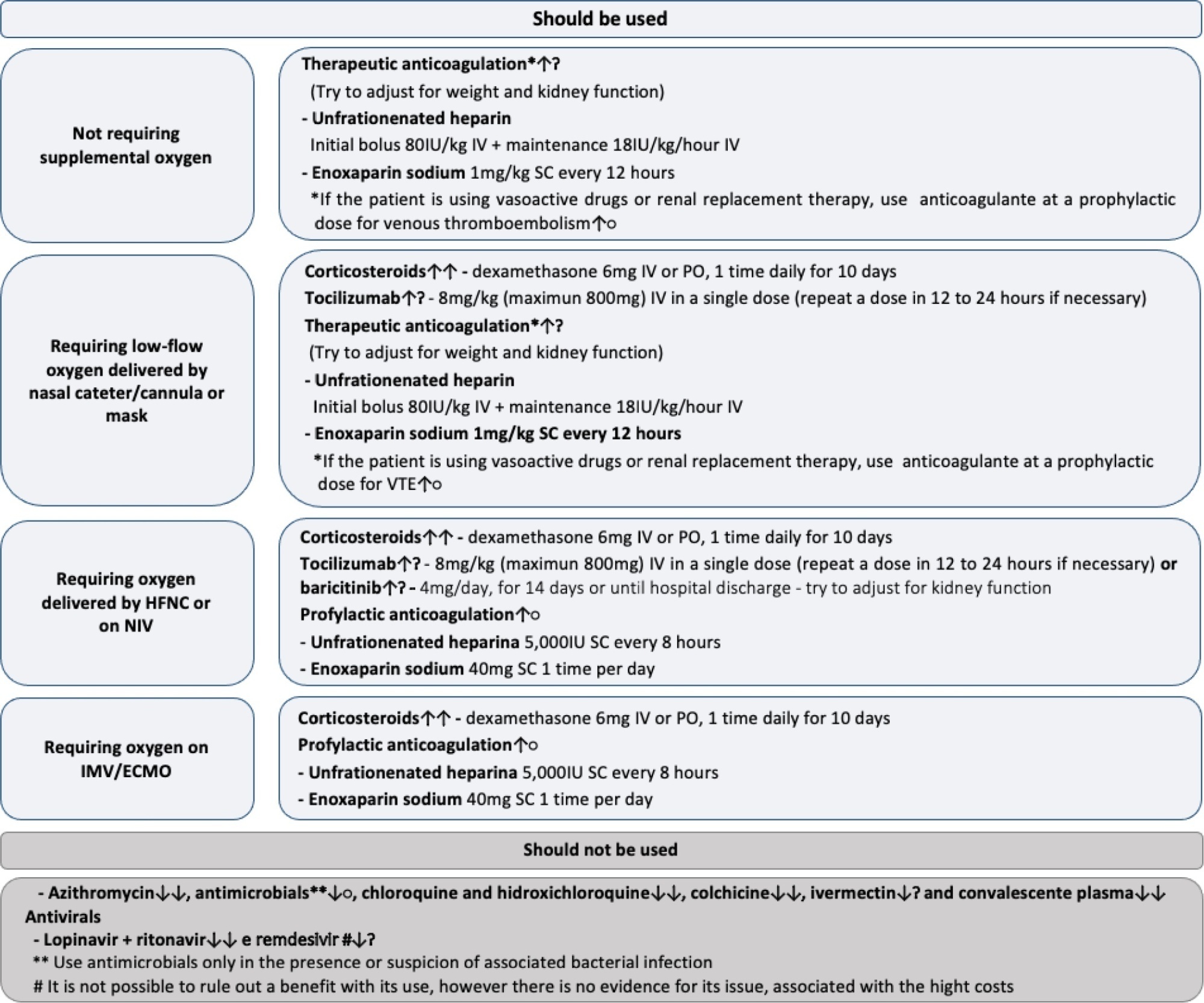
To update the recommendations to support decisions regarding the pharmacological treatment of patients hospitalized with COVID-19 in Brazil.
Experts, including representatives of the Ministry of Health and methodologists, created this guideline. The method used for the rapid development of guidelines was based on the adoption and/or adaptation of existing international guidelines (GRADE ADOLOPMENT) and supported by the e-COVID-19 RecMap platform. The quality of the evidence and the preparation of the recommendations followed the GRADE method.
Twenty-one recommendations were generated, including strong recommendations for the use of corticosteroids in patients using supplemental oxygen and conditional recommendations for the use of tocilizumab and baricitinib for patients on supplemental oxygen or on noninvasive ventilation and anticoagulants to prevent thromboembolism. Due to suspension of use authorization, it was not possible to make recommendations regarding the use of casirivimab + imdevimab. Strong recommendations against the use of azithromycin in patients without suspected bacterial infection, hydroxychloroquine, convalescent plasma, colchicine, and lopinavir + ritonavir and conditional recommendations against the use of ivermectin and remdesivir were made.
New recommendations for the treatment of hospitalized patients with COVID-19 were generated, such as those for tocilizumab and baricitinib. Corticosteroids and prophylaxis for thromboembolism are still recommended, the latter with conditional recommendation. Several drugs were considered ineffective and should not be used to provide the best treatment according to the principles of evidence-based medicine and to promote resource economy.
Abstract
Crit Care Sci. 2023;35(3):302-310
DOI 10.5935/2965-2774.20230141-pt
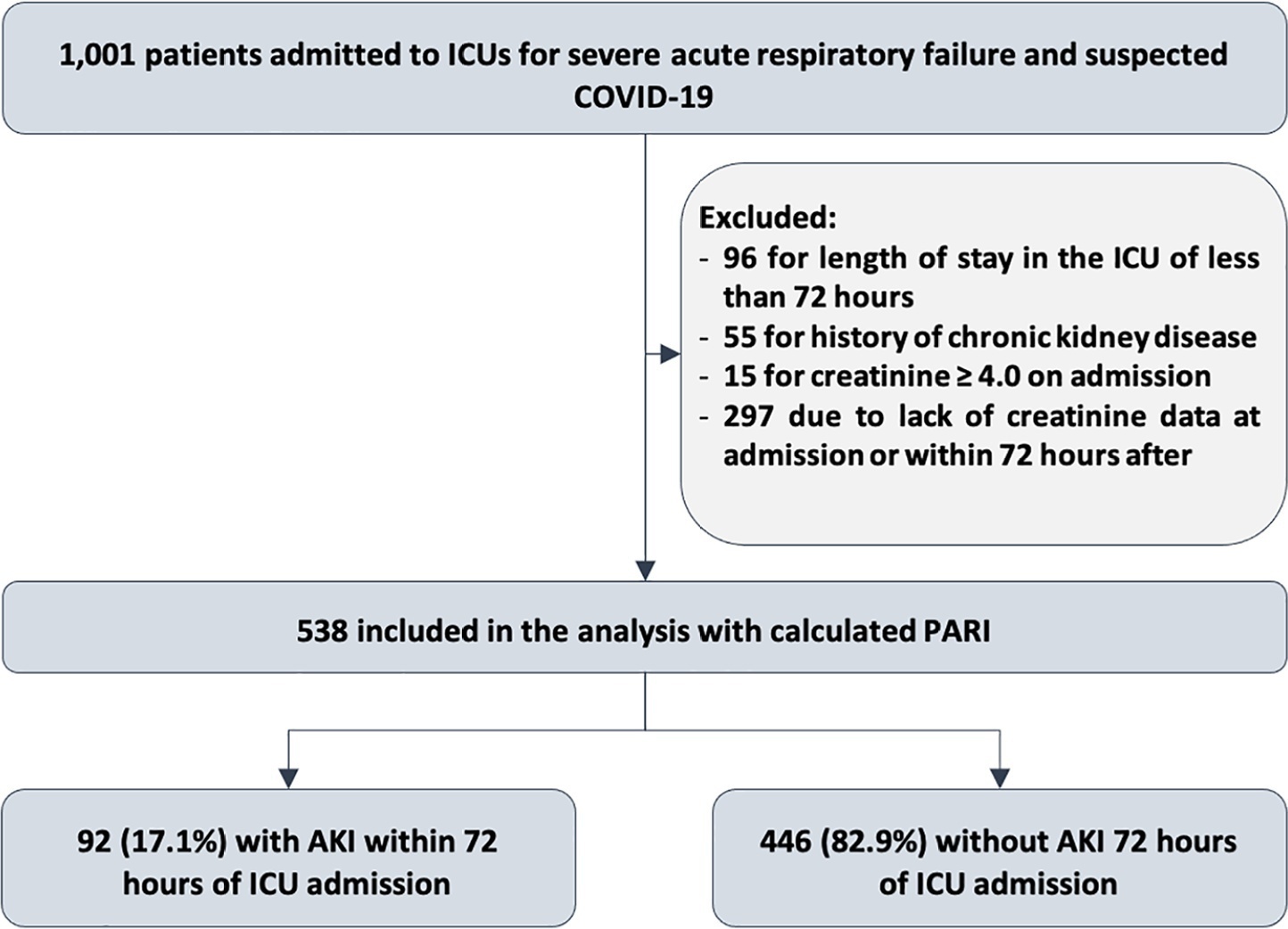
To evaluate the accuracy of the persistent AKI risk index (PARI) in predicting acute kidney injury within 72 hours after admission to the intensive care unit, persistent acute kidney injury, renal replacement therapy, and death within 7 days in patients hospitalized due to acute respiratory failure.
This study was done in a cohort of diagnoses of consecutive adult patients admitted to the intensive care unit of eight hospitals in Curitiba, Brazil, between March and September 2020 due to acute respiratory failure secondary to suspected COVID-19. The COVID-19 diagnosis was confirmed or refuted by RT-PCR for the detection of SARS-CoV-2. The ability of PARI to predict acute kidney injury at 72 hours, persistent acute kidney injury, renal replacement therapy, and death within 7 days was analyzed by ROC curves in comparison to delta creatinine, SOFA, and APACHE II.
Of the 1,001 patients in the cohort, 538 were included in the analysis. The mean age was 62 ± 17 years, 54.8% were men, and the median APACHE II score was 12. At admission, the median SOFA score was 3, and 83.3% had no renal dysfunction. After admission to the intensive care unit, 17.1% had acute kidney injury within 72 hours, and through 7 days, 19.5% had persistent acute kidney injury, 5% underwent renal replacement therapy, and 17.1% died. The PARI had an area under the ROC curve of 0.75 (0.696 - 0.807) for the prediction of acute kidney injury at 72 hours, 0.71 (0.613 - 0.807) for renal replacement therapy, and 0.64 (0.565 - 0.710) for death.
The PARI has acceptable accuracy in predicting acute kidney injury within 72 hours and renal replacement therapy within 7 days of admission to the intensive care unit, but it is not significantly better than the other scores.
Abstract
Crit Care Sci. 2023;35(2):156-162
DOI 10.5935/2965-2774.20230343-pt
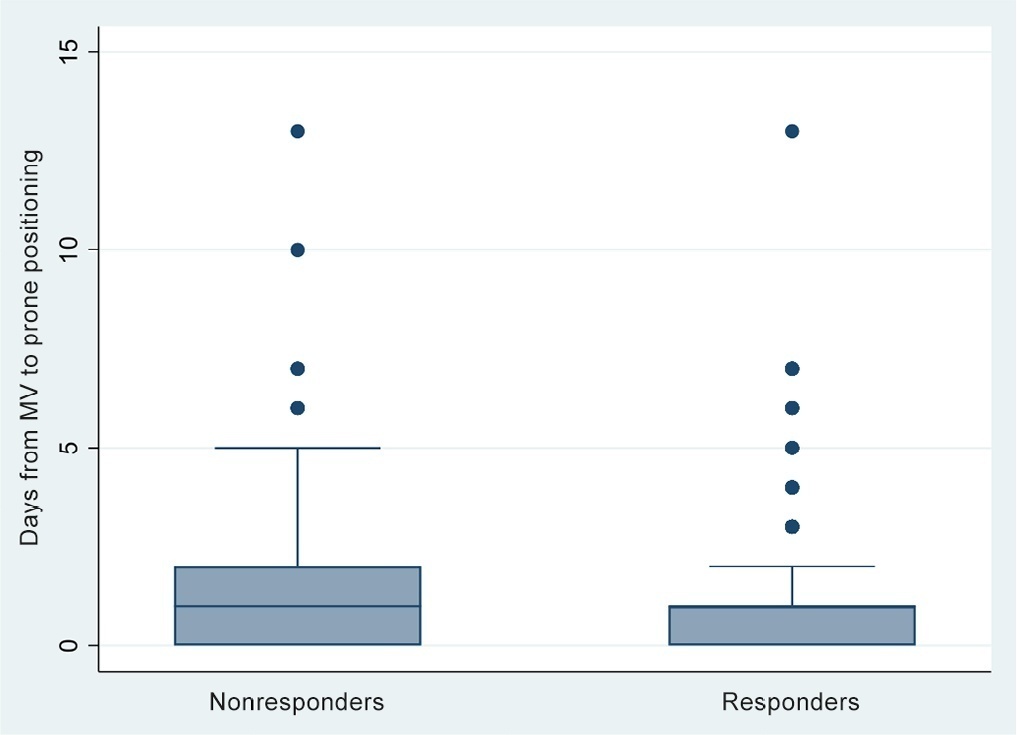
To identify risk factors for nonresponse to prone positioning in mechanically ventilated patients with COVID-19-associated severe acute respiratory distress syndrome and refractory hypoxemia in a tertiary care hospital in Colombia.
Observational study based on a retrospective cohort of mechanically ventilated patients with severe acute respiratory distress syndrome due to SARS-CoV-2 who underwent prone positioning due to refractory hypoxemia. The study considered an improvement ≥ 20% in the PaO2/FiO2 ratio after the first cycle of 16 hours in the prone position to be a ‘response’. Nonresponding patients were considered cases, and responding patients were controls. We controlled for clinical, laboratory, and radiological variables.
A total of 724 patients were included (58.67 ± 12.37 years, 67.7% males). Of those, 21.9% were nonresponders. Mortality was 54.1% for nonresponders and 31.3% for responders (p < 0.001). Variables associated with nonresponse were time from the start of mechanical ventilation to pronation (OR 1.23; 95%CI 1.10 - 1.41); preintubation PaO2/FiO2 ratio (OR 0.62; 95%CI 0.40 - 0.96); preprone PaO2/FiO2 ratio (OR 1.88. 95%CI 1.22 - 2.94); and radiologic multilobe consolidation (OR 2.12; 95%CI 1.33 - 3.33) or mixed pattern (OR 1.72; 95%CI 1.07 - 2.85) compared with a ground-glass pattern.
This study identified factors associated with nonresponse to prone positioning in patients with refractory hypoxemia and acute respiratory distress syndrome due to SARS-CoV-2 receiving mechanical ventilation. Recognizing such factors helps identify candidates for other rescue strategies, including more extensive prone positioning or extracorporeal membrane oxygenation. Further studies are needed to assess the consistency of these findings in populations with acute respiratory distress syndrome of other etiologies.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) ICU (25) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)