Abstract
Crit Care Sci. 2023;35(4):355-366
DOI 10.5935/2965-2774.20230015-pt
To compare, within a cohort of patients with acute respiratory failure, the phenotypes of patients with and without COVID-19 in the context of the pandemic and evaluate whether COVID-19 is an independent predictor of intensive care unit mortality.
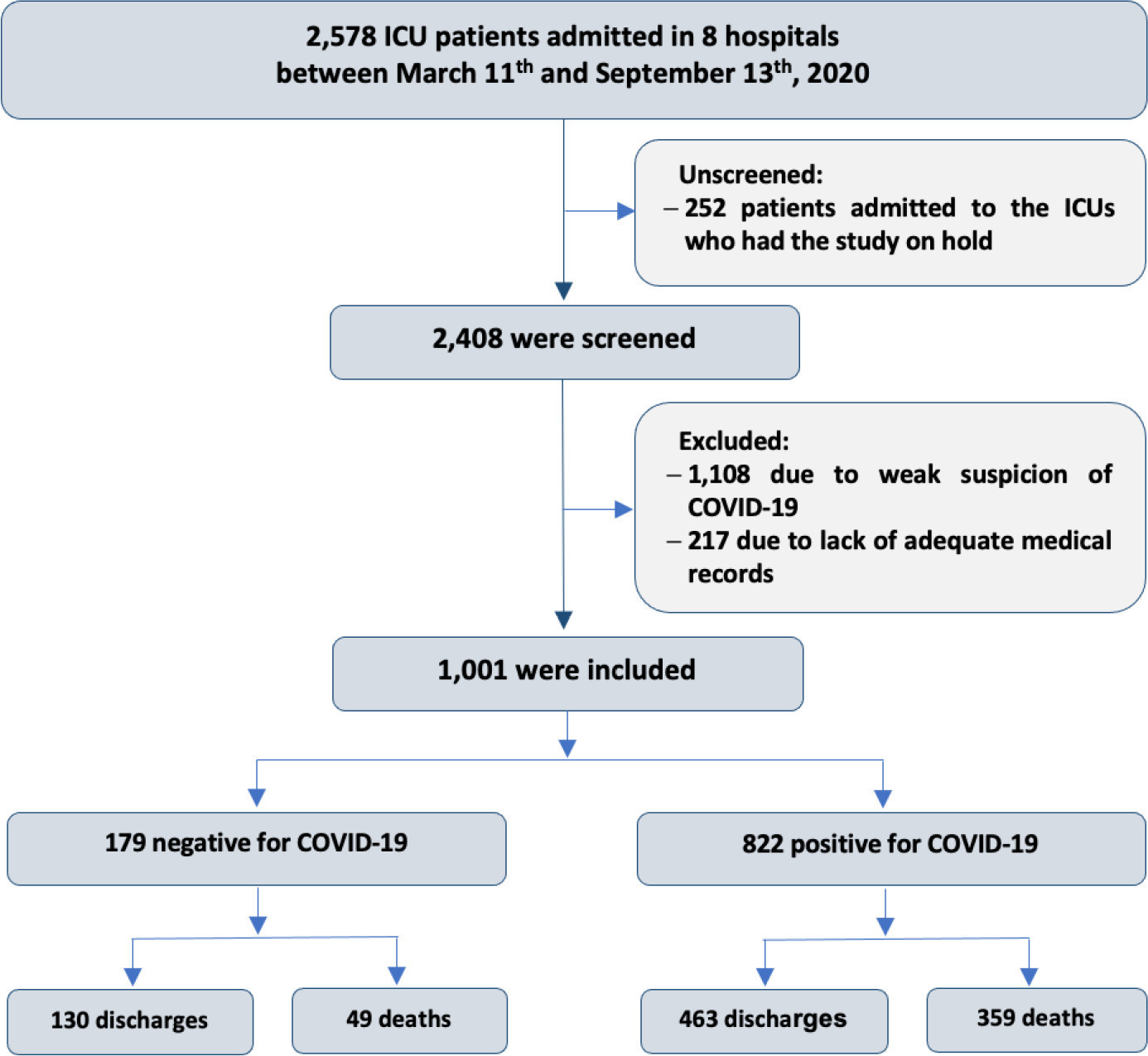
This historical cohort study evaluated 1001 acute respiratory failure patients with suspected COVID-19 admitted to the intensive care unit of 8 hospitals. Patients were classified as COVID-19 cases and non-COVID-19 cases according to real-time polymerase chain reaction results. Data on clinical and demographic characteristics were collected on intensive care unit admission, as well as daily clinical and laboratory data and intensive care unit outcomes.
Although the groups did not differ in terms of APACHE II or SOFA scores at admission, the COVID-19 group had more initial symptoms of fever, myalgia and diarrhea, had a longer duration of symptoms, and had a higher prevalence of obesity. They also had a lower PaO2/FiO2 ratio, lower platelet levels than non-COVID-19 patients, and more metabolic changes, such as higher levels of blood glucose, C-reactive protein, and lactic dehydrogenase. Patients with non-COVID-19 acute respiratory failure had a higher prevalence of chronic obstructive pulmonary disease/asthma and cardiopathy. Patients with COVID-19 stayed in the hospital longer and had more complications, such as acute kidney failure, severe acute respiratory distress syndrome and severe infection. The all-cause mortality rate was also higher in this group (43.7% in the COVID-19 group versus 27.4% in the non-COVID-19 group). The diagnosis of COVID-19 was a predictor of intensive care unit mortality (odds ratio, 2.77; 95%CI, 1.89 - 4.07; p < 0.001), regardless of age or Charlson Comorbidity Index score.
In a prospective cohort of patients admitted with acute respiratory failure, patients with COVID-19 had a clearly different phenotype and a higher mortality than non-COVID-19 patients. This may help to outline more accurate screening and appropriate and timely treatment for these patients.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):624-634
DOI 10.5935/0103-507X.20210088
To identify the clinical and epidemiological profile of adult intensive care units in Brazil.
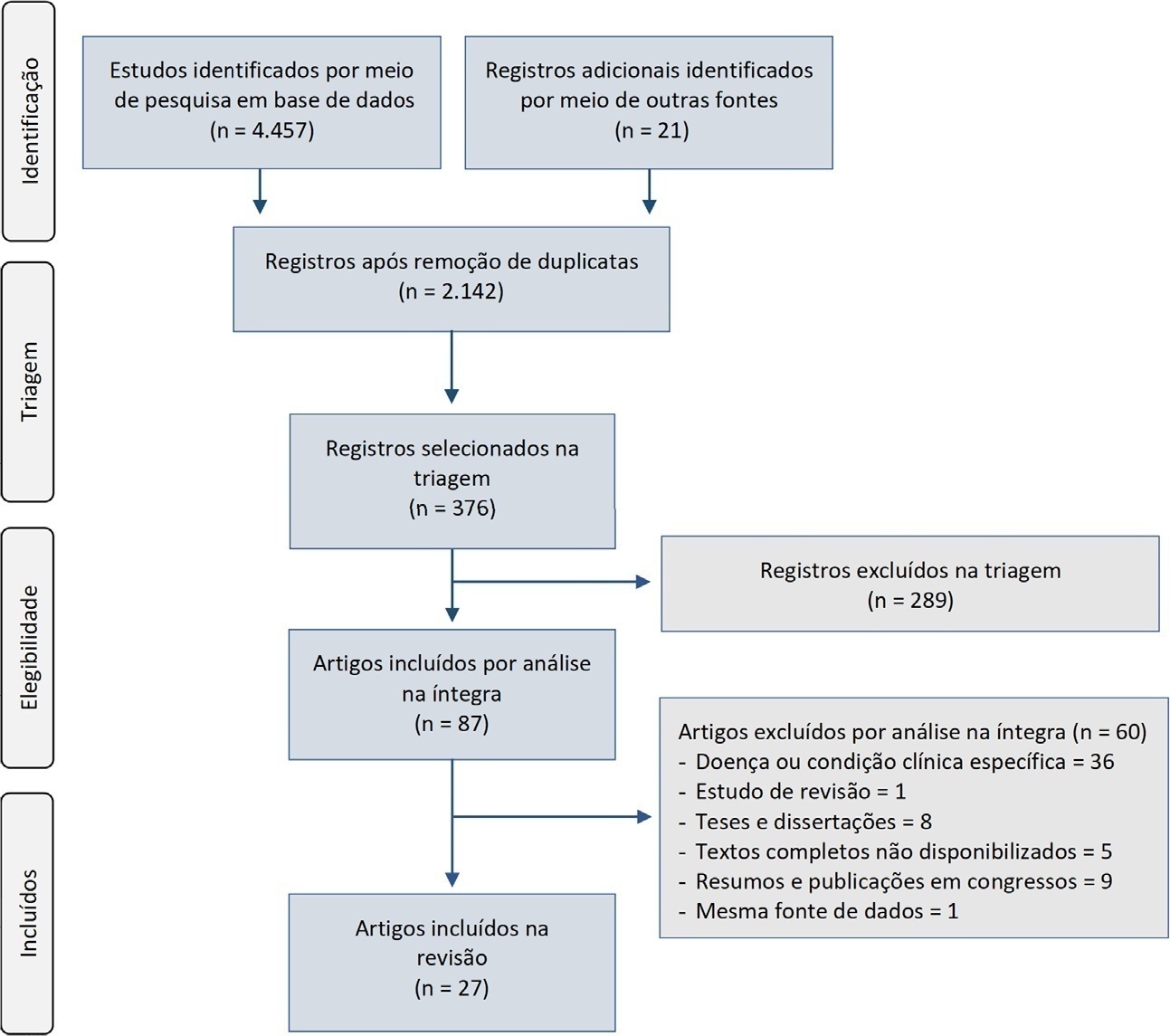
A systematic review was performed using a comprehensive strategy to search PubMed®, Embase, SciELO, and the Biblioteca Virtual em Saúde. The eligibility criteria for this review were observational studies that described the epidemiological and/or clinical profile of critically ill patients admitted to Brazilian intensive care units and were published between 2007 and 2020.
From the 4,457 identified studies, 27 were eligible for this review, constituting an analysis of 113 intensive care units and a final sample of 75,280 individuals. There was a predominance of male and elderly patients. Cardiovascular diseases were the main cause of admission to the intensive care unit. The Acute Physiology and Chronic Health Evaluation II score was the most widely used disease severity assessment system. The length of stay and mortality in the intensive care unit varied widely between institutions.
These results can help guide the planning and organization of intensive care units, providing support for decision-making and the implementation of interventions that ensure better quality patient care.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):229-234
DOI 10.5935/0103-507X.20200041
To depict the clinical presentation and outcomes of a cohort of critically ill patients with esophageal cancer.
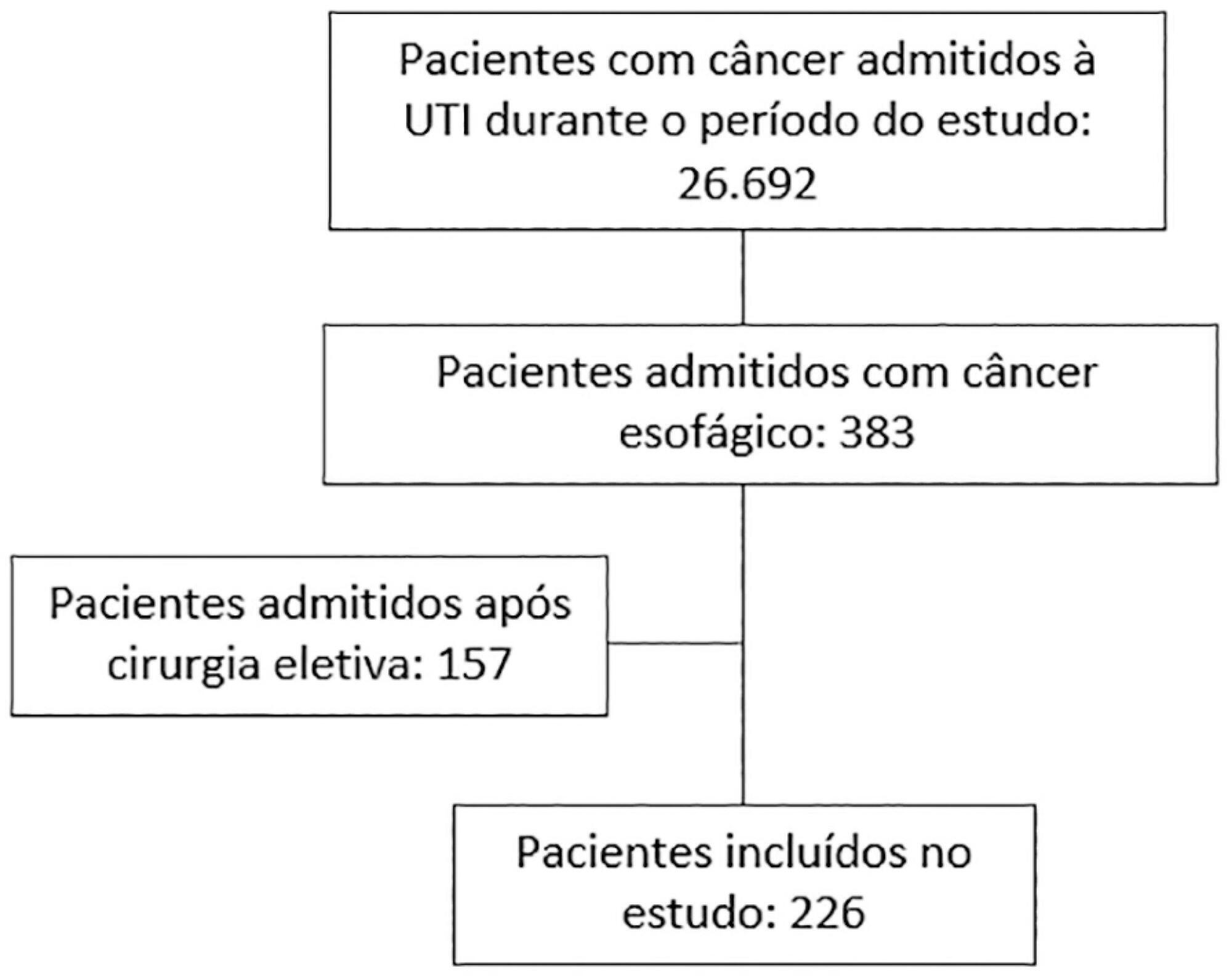
We carried out a multicenter retrospective study that included patients with esophageal cancer admitted to intensive care units with acute illness between September 2009 and December 2017. We collected the demographic and clinical characteristics of all included patients, as well as organ-support measures and hospital outcomes. We performed logistic regression analysis to identify independent factors associated with in-hospital mortality.
Of 226 patients included in the study, 131 (58.0%) patients died before hospital discharge. Squamous cell carcinoma was more frequent than adenocarcinoma, and 124 (54.9%) patients had metastatic cancer. The main reasons for admission were sepsis/septic shock and acute respiratory failure. Mechanical ventilation (OR = 6.18; 95%CI 2.86 - 13.35) and metastatic disease (OR = 7.10; 95%CI 3.35 - 15.05) were independently associated with in-hospital mortality.
In this cohort of patients with esophageal cancer admitted to intensive care units with acute illness, the in-hospital mortality rate was very high. The requirement for invasive mechanical ventilation and metastatic disease were independent prognostic factors and should be considered in discussions about the short-term outcomes of these patients.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):124-127
DOI 10.1590/S0103-507X2008000200002
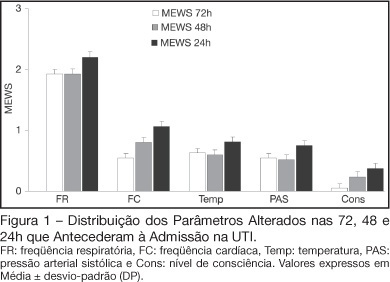
BACKGROUND AND OBJECTIVES: Prognosis of patients in the intensive care unit (ICU) has a relation with their severity just before admission. The Modified Early Warning Score (MEWS) was used to evaluate the severe condition of patients 12, 24 and 72 hours before admission in the ICU, assess the most prevalent parameters and correlate the MEWS before ICU with the outcome (survival versus death). METHODS: Retrospective analyses of 65 patients consecutively admitted to the ICU from July to October, 2006 evaluating the physiological parameters 72 hours prior to admission. RESULTS: APACHE II mean was 22.2 ± 7.9 points, mortality was 54.6% and standardized mortality ratio means was 1.24. MEWS means were 3.7 ± 0.2; 4.0 ± 0.2 and 5.1 ± 0.2 points, calculated 72, 48 and 24 hours previous to ICU admission, respectively. An increasing percentage of patients with MEWS > 3 points within 72, 48 and 24 hours before admission - 43.8%, 59.4% and 73.4%, respectively was recorded. Among the included physiological parameters respiratory rate contributed the most to the MEWS. Highest mortality was found in patients with MEWS > 3 points already found 72 hours before admission. Patients who died presented with a significant increase in the MEWS 24 hours prior to admission to the ICU (in relation to the MEWS recorded 72 hours before) but the situation was not identified in survivors. CONCLUSIONS: MEWS closely identified the severity of patients admitted to the ICU, suggesting that it can be a reliable score, useful in the situations preceding the ICU.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):128-134
DOI 10.1590/S0103-507X2008000200003
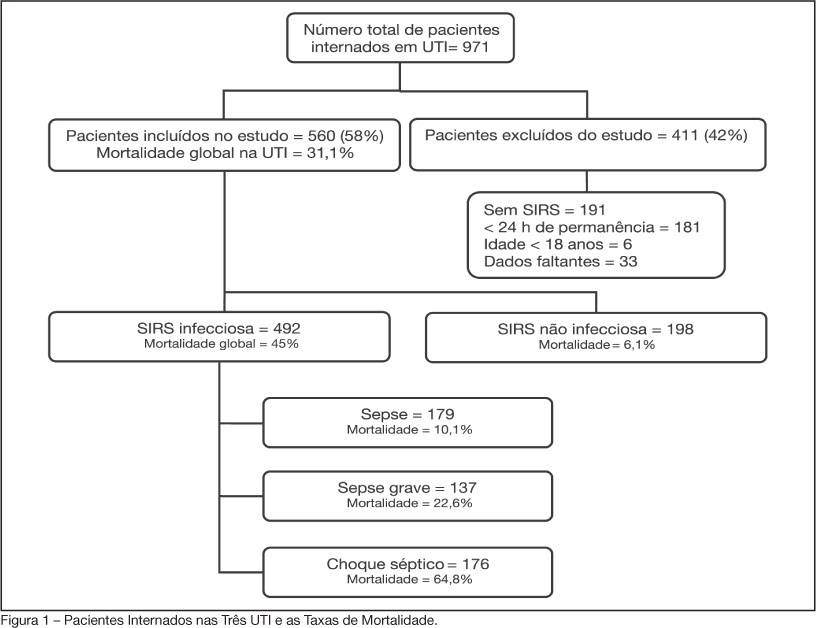
BACKGROUND AND OBJECTIVES: Sepsis is the main cause of death in patients treated in intensive care units (ICU). The aim of this study was to evaluate etiology, prognostic factors and mortality of septic patients treated in ICU of Passo Fundo, Brazil. METHODS: Out of 971 consecutive patients prospectively evaluated from August 2005 to February 2006, 560 were selected due to presence of systemic inflammatory response syndrome (SIRS) and followed for 28 days or until discharge or death. Patients were categorized according with the etiology of SIRS and further classified as having SIRS, sepsis, severe sepsis and septic shock. Prognosis was assessed by means of Apache II and SOFA. Mortality was compared in different etiologies of sepsis, APACHE II and SOFA scores, parameters. RESULTS: Of the 971 patients admitted to the ICU, 560 developed SIRS (58%). The most frequent cause of internation was neurological disease (28.9%), the most frequent site of infection was the respiratory tract (71.6%), and the most prevalent pathogens were gram-negative bacilli (53.2%). Mean APACHE II score was 18 ± 9, and mean SOFA score was 5 ± 4. Median ICU stay was 6 (3-11) days and overall mortality rate was 31.1%: 6.1% for non-infectious SIRS, 10.1% for sepsis, 22.6% for severe sepsis, and 64.8% for septic shock. CONCLUSIONS: Sepsis is an important health problem that leads to an extremely high mortality rate in the ICU of Passo Fundo, Brazil.
Abstract
Rev Bras Ter Intensiva. 2006;18(1):9-17
DOI 10.1590/S0103-507X2006000100003
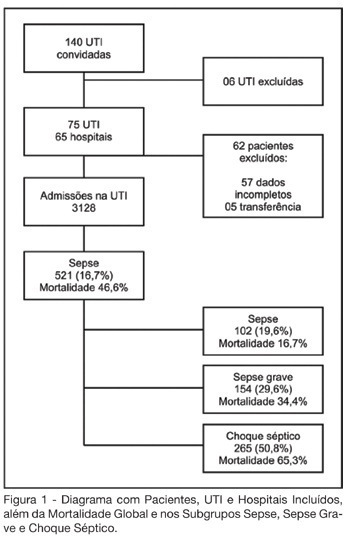
BACKGROUND AND OBJECTIVES: Sepsis represents the major cause of death in the ICUs all over the world. Many studies have shown an increasing incidence over time and only a slight reduce in mortality. Many new treatment strategies are arising and we should define the incidence and features of sepsis in Brazil. METHODS: Prospective cohort study in sixty-five hospitals all over Brazil. The patients who were admitted or who developed sepsis during the month of September, 2003 were enrolled. They were followed until the 28th day and/or until their discharge. The diagnoses were made in accordance to the criteria proposed by ACCP/SCCM. It were evaluated demographic features, APACHE II score, SOFA (Sepsis-related Organ Failure Assessment) score, mortality, sources of infections, microbiology, morbidities and length of stay (LOS). RESULTS: Seventy-five ICUs from all regions of Brazil took part in the study.3128 patients were identified and 521 (16.7%) filled the criteria of sepsis, severe sepsis or septic shock. Mean age was 61.7 (IQR 39-79), 293 (55.7%) were males, and the overall 28-day mortality rate was 46.6%. Average APACHE II score was 20 and SOFA score on the first day was 7 (IQR 4-10). SOFA score in the mortality group was higher on day 1 (8, IQR 5-11), and had increased on day 3 (9, IQR 6-12). The mortality rate for sepsis, severe sepsis and septic shock was 16.7%, 34.4% and 65.3%, respectively. The average LOS was 15 days (IQR 5-22). The two main sources of infection were the respiratory tract (69%) and the abdomen one (23.1%). Gram-negative bacilli were more prevalent (40.1%). Gram-positive cocci were identified in 32.8% and fungi infections in 5%. Mechanical ventilation was observed in 82.1% of the patients, Swan-Ganz catheter in 18.8%, vasopressors in 66.2% and hemotransfusion in 44.7%. CONCLUSIONS: It was observed a high mortality of sepsis in the ICUs in Brazil. The high frequency of septic shock demonstrated a group at high risk of death. In order to have a better use of the resources and reduce in mortality during the next 5 years, it is very important to identify our specific features related to this syndrome.
Abstract
Rev Bras Ter Intensiva. 2006;18(1):38-44
DOI 10.1590/S0103-507X2006000100008
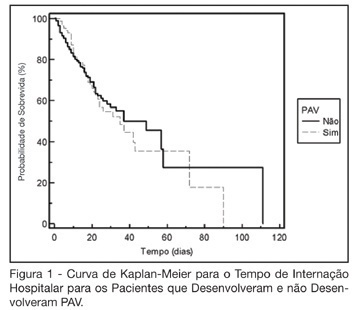
BACKGROUND AND OBJECTIVES: The ventilator-associated pneumonia (VAP) is a severe infection that presents multiple causes which can vary depending on the type of intensive care unit, type of patients, emphasizing the needs for vigilance measures with local data. The aim of this study is to describe the incidence, risk factors and mortality of VAP in patients in a surgical ICU. METHODS: Prospective cohort conducted from January 2004 to January 2005. It was included all the patients in mechanical ventilation, followed daily to collect data about demographics, diagnostic, APACHE II and TISS 28 scores, duration of mechanical ventilation, length of stay, incidence of VAP and mortality. RESULTS: 462 patients were studied; age 57.2 ± 16.6 years, 55% men. The mean APACHE II score was 18.3 and the incidence of VAP was 18.8%. The TISS score at admission OR = 1.050 (IC 95%: 1.003-1.050) and the enteral nutrition OR = 5.609 (IC 3.351-9.388) were factors associated with VAP and the prophylactic use of antibiotics was a factor of protection OR = 0.399 (IC95%: 0.177-0.902). The patients with VAP had longer length of stay in ICU (10.3 ± 10.7 vs 4.9 ± 3.3 days), higher median of duration of mechanical ventilation (4 vs 1 days), higher mean of TISS 28 (24.4 ± 4.6 vs 22.8 ± 4.5), and higher crude mortality (46 vs 28.8%) when compared with the patients without VAP. CONCLUSIONS: VAP was a frequent infection in surgical patients in mechanical ventilation. Enteral nutrition and admission TISS were risk factors and the previous use of antibiotics was protection factor to develop VAP. In our sample the results demonstrate that VAP is associated with higher duration in mechanical ventilation, longer length of stay and higher mortality.
Abstract
Rev Bras Ter Intensiva. 2006;18(4):344-350
DOI 10.1590/S0103-507X2006000400005
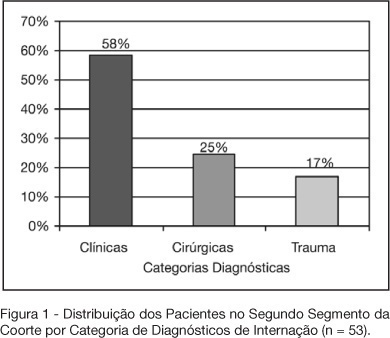
BACKGROUND AND OBJECTIVES: Variable magnitude of impact on the outcomes of the critically ill patients has been credited to ventilation-associated pneumonia, in terms of mortality, length of hospital stay and mechanic ventilation days. Three objectives have been defined in this study: mortality and incidence of ventilation-associated pneumonia before and after the implantation of a prophylaxis protocol (primary objectives); microbiologic mapping (secondary objective) as an instrument to optimize therapy. METHODS: A historical cohort was followed during the period of August 2001 to January 2004, fragmented in two segments, pre (until January 2003, n = 52) and post-implantation of the mentioned protocol, the analysis of mortality and microbiologic mapping been performed in the second segment (control group n = 39 and case group n = 14). RESULTS: The incidence rates from 2001 to 2003 were respectively 28.05‰ ± 12.92‰, 22.45‰ ± 10.18‰ and 10.75‰ ± 7.61‰. The decrease in this rate after the intervention did not reach statistical significance (p > 0.4). Mortality rates were 49% in the control group (CI 95 = 33% to 65%) and 43% in the case group (CI 95 = 14% to 72%), OR = 0.88 (CI 95 = 0.26 to 2.94), without statistical significance either (p = 0.65). Eight bronco-alveolar lavage were obtained (57%), 50% with multiple flora. Pseudomonas aeruginosa was isolated in six patients (75%), Acinetobacter sp in one case (12.5 %) and methicilin-resistent Staphylococcus aureus (MRSA) in one (12.5%). Other Gram negative bacilli producers of extended spectrum betalactamase (ESBL) were isolated in two cases (25%) and Stenotrophomonas maltophilia in another (12.5%). CONCLUSIONS: The incidence rate of ventilation-associated pneumonia revealed a tendency to considerable reduction after the utilization of the prophylaxis protocol, while the results suggest no impact on mortality rates. Further prospective evaluation of a greater sample is required, in order to get to definite conclusions regarding prognosis. The isolated germs were, in its majority, high risk pathogens to multiresistance to antibiotics, pointing the necessity of knowledge of local susceptibility profile, so that an adequate initial therapeutic strategy can be undertaken.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)