Abstract
Rev Bras Ter Intensiva. 2012;24(4):357-361
DOI 10.1590/S0103-507X2012000400011
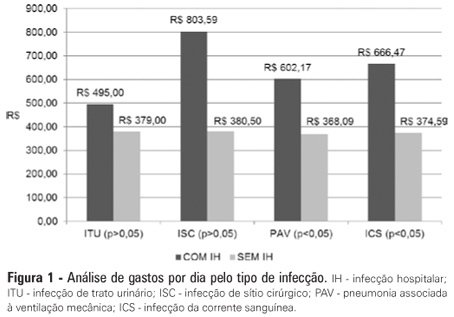
OBJECTIVE: Infections in intensive care units are often associated with a high morbidity and mortality in addition to high costs. An analysis of these aspects can assist in optimizing the allocation of relevant financial resources. METHODS: This retrospective study analyzed the hospital administration and quality in intensive care medical databases [Sistema de Gestão Hospitalar (SGH)] and RM Janus®. A cost analysis was performed by evaluating the medical products and materials used in direct medical care. The costs are reported in the Brazilian national currency (Real). The cost and length of stay analyses were performed for all the costs studied. The median was used to determine the costs involved. Costs were also adjusted by the patients' length of stay in the intensive care unit. RESULTS: In total, 974 individuals were analyzed, of which 51% were male, and the mean age was 57±18.24 years. There were 87 patients (8.9%) identified who had nosocomial infections associated with the intensive care unit. The median cost per admission and the length of stay for all the patients sampled were R$1.257,53 and 3 days, respectively. Compared to the patients without an infection, the patients with an infection had longer hospital stays (15 [11-25] versus 3 [2-6] days, p<0.01), increased costs per patient in the intensive care unit (median R$9.763,78 [5445.64 - 18,007.90] versus R$1.093,94 [416.14 - 2755.90], p<0.01) and increased costs per day of hospitalization in the intensive care unit (R$618,00 [407.81 - 838.69] versus R$359,00 [174.59 - 719.12], p<0.01). CONCLUSION: Nosocomial infections associated with the intensive care unit were determinants of increased costs and longer hospital stays. However, the study design did not allow us to evaluate specific aspects of cause and effect.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):239-244
DOI 10.5935/0103-507X.20130041
This study sought to evaluate infections related to health care caused by coagulase-negative Staphylococci in a neonatal intensive care unit by assessing antimicrobial susceptibility profiles and potentially effective antibiotic regimens.
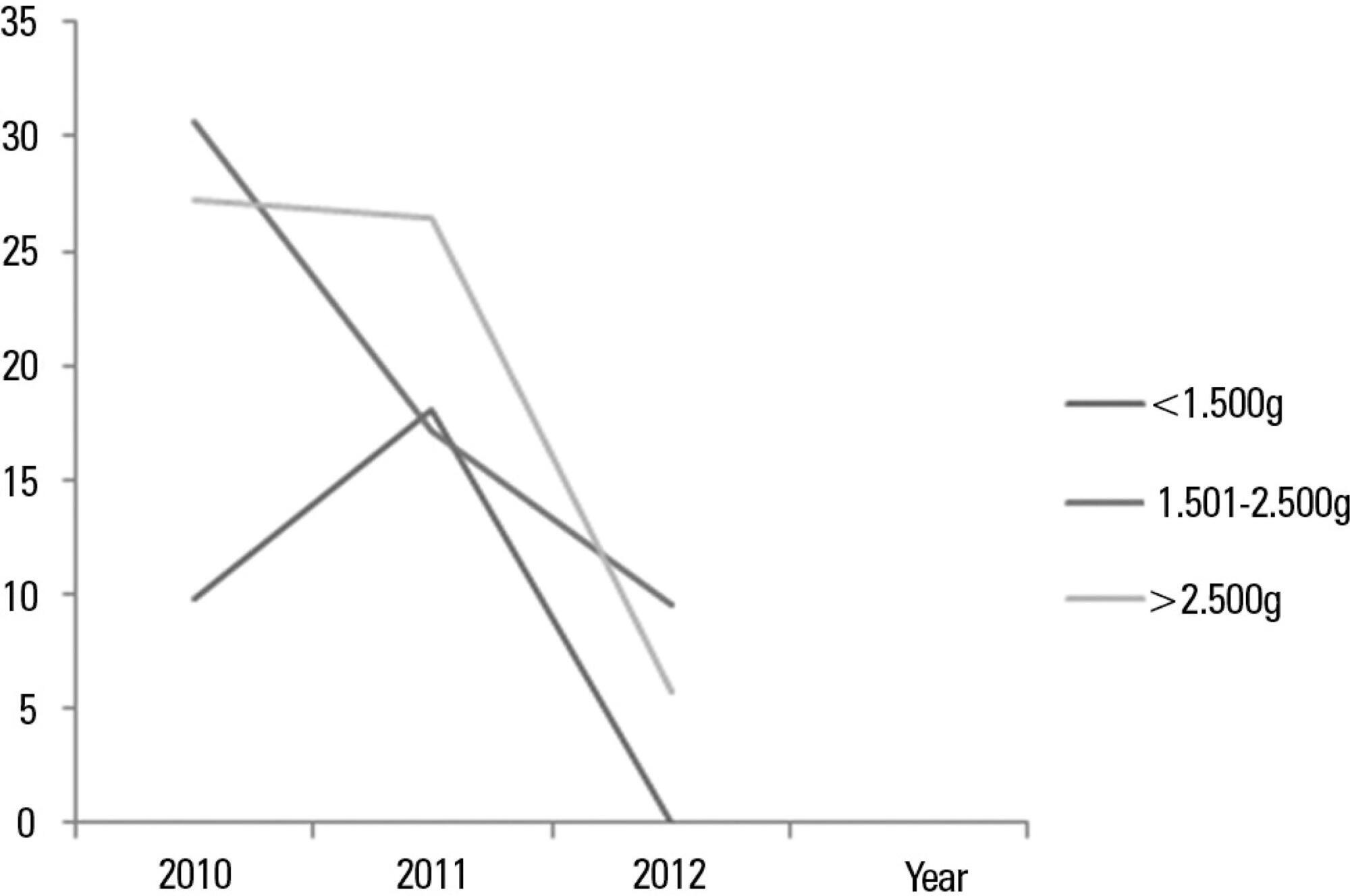
This was a retrospective descriptive study performed on a case series of healthcare-associated infections, and the antimicrobial susceptibility profiles were evaluated. Newborns from other hospitals who were admitted to a neonatal intensive care unit in Rio de Janeiro between January 1, 2010, and June 30, 2012, were studied.
In total, 765 patients were admitted, totaling 3,051 patient-days, and the incidence density of general infection was 18.9 per 1,000 patient-days. The rate of central venous catheter use was 71.6%, and the positive culture rate for all sites and all infections related to health care were 68.4%. Coagulase-negative Staphylococci were identified in 11 (19.2%) of 57 health care-related infections, and infections with extended-spectrum beta-lactamase producing Klebsiella pneumoniae and Candida sp. constituted 5 cases each. Of the 11 cases of coagulase-negative Staphylococci, 10 (90.9%) were primary bloodstream infections. The sensitivity of the coagulase-negative Staphylococci isolates to vancomycin, clindamycin, ciprofloxacin, oxacillin and gentamycin was 100%, 81.8%, 72.7%, 27.2% and 22.2%, respectively. There were no deaths directly attributed to coagulase-negative Staphylococci infection.
Coagulase-negative Staphylococci was the main agent identified in healthcare-associated infections, with low rates of infections related to central venous catheter. In hospitals with a high oxacillin resistance profile, similar to those included in this study, vancomycin may be used as an initial therapy, although clindamycin represents a viable alternative.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):96-98
DOI 10.1590/S0103-507X2010000100016
A case of Chryseobacterium indologenes infection is reported, identified in an invasive mechanic ventilation patient's tracheal aspiration material. Epidemiological, microbiological, and intensive care unit therapy aspects are discussed. The patient was a 30 years-old male, admitted with idiopathic medullary aplasia and febrile neutropenia, referred to the intensive care unit with severe bronchopneumonia and sepsis of pulmonary origin. Most of the previously reported Chryseobacterium indologenes infection cases were associated with severe diseases and polymicrobial infections which could make difficult interpreting antimicrobial therapy options against this agent.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):269-275
DOI 10.1590/S0103-507X2009000300006
OBJECTIVE: Infection is one of the main complications of dialysis procedures to correct renal injury, with a significant impact on morbidity mortality in chronic and critically acute dialysis patients. The objective of this work was to review literature on infection in patients submitted to hemodyalisis. METHODS: A survey of publications from 1990 to March 2008 was carried out in the database COCHRANE, PubMed/MEDLINE, Latin-American and Caribbean literature on Health Sciences and Nursing database. In Health Science (DECS) and Medical Subject Headings Section (MeSH) from |PubMed/MEDLINE the following descriptors were used: infection; cross infection; bacteremia; renal dialysis; renal failure;acute renal failure; hemofiltation; hemodiafiltration; renal replacement therapy. RESULTS: Thirty three articles were selected. Most publications were American, from 2001 to 2005 and mainly about vascular access-related infection. Studies diverged on the definition of infection and nomenclature, hindering comparisons. Fiver articles covered different infection topographies, 16 studied vascular access-related infections in the different types of vascular accesses, nine specifically focused on temporary central catheters for hemodialysis and only three studied infections in intensive care unit patients. Temporary central catheters for hemodialysis were identified as the principal risk factor. CONCLUSION: There is a need for studies about infection incidence in critically ill, submitted to dialysis with temporary catheters, due to acute renal injury to define a causal relationship and risk factors to orient adequate prevention and control measures.
Abstract
Rev Bras Ter Intensiva. 2006;18(1):27-33
DOI 10.1590/S0103-507X2006000100006
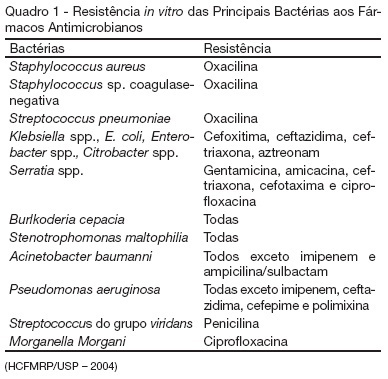
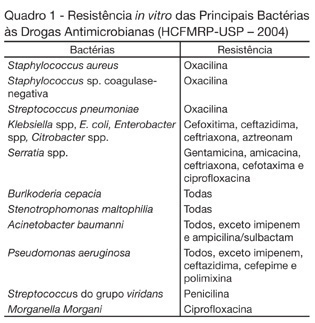
BACKGROUND AND OBJECTIVES: Nosocomial infection represents a challenge in clinical practice involving hospitalized patients, as they considerably extend the hospitalization period and morbidity and mortality rates and, at the same time, increase hospital costs. Given their clinical conditions, which require invasive procedures and antimicrobial treatment, hospitalized patients, especially at the Intensive Care Unit, are particularly susceptible to hospital infection. This study aimed to evaluate the occurrence of multiresistant bacteria in patients hospitalized at the Intensive Care Unit of a Brazilian emergency hospital. METHODS: Our retrospective study was approved by the Ethics Committee and considered the period between October 2003 and September 2004. A database was developed through variable coding and double entry, and Statistical Package for Social Sciences (SPSS) software, version 10.0, was used for statistical analysis. RESULTS: Multiresistant bacteria were identified in 68 patients, 47 (69.1%) of whom were men, with 55 years as the mean age. All patients were submitted to endotracheal intubation and central venipuncture. The most frequent bacteria were coagulase-negative Staphylococcus sp. (36.4%), followed by Staphylococcus aureus (19%). Cephalosporin was the most frequently used (21.4%) antimicrobial agent. CONCLUSIONS: Knowledge on infection occurrence provokes reflections on multiresistance, directs educative actions and favors interventions to prevent and control problem situations.
Abstract
Rev Bras Ter Intensiva. 2006;18(4):344-350
DOI 10.1590/S0103-507X2006000400005
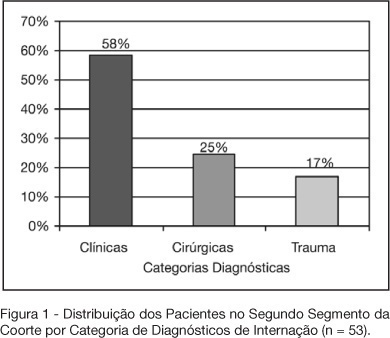
BACKGROUND AND OBJECTIVES: Variable magnitude of impact on the outcomes of the critically ill patients has been credited to ventilation-associated pneumonia, in terms of mortality, length of hospital stay and mechanic ventilation days. Three objectives have been defined in this study: mortality and incidence of ventilation-associated pneumonia before and after the implantation of a prophylaxis protocol (primary objectives); microbiologic mapping (secondary objective) as an instrument to optimize therapy. METHODS: A historical cohort was followed during the period of August 2001 to January 2004, fragmented in two segments, pre (until January 2003, n = 52) and post-implantation of the mentioned protocol, the analysis of mortality and microbiologic mapping been performed in the second segment (control group n = 39 and case group n = 14). RESULTS: The incidence rates from 2001 to 2003 were respectively 28.05‰ ± 12.92‰, 22.45‰ ± 10.18‰ and 10.75‰ ± 7.61‰. The decrease in this rate after the intervention did not reach statistical significance (p > 0.4). Mortality rates were 49% in the control group (CI 95 = 33% to 65%) and 43% in the case group (CI 95 = 14% to 72%), OR = 0.88 (CI 95 = 0.26 to 2.94), without statistical significance either (p = 0.65). Eight bronco-alveolar lavage were obtained (57%), 50% with multiple flora. Pseudomonas aeruginosa was isolated in six patients (75%), Acinetobacter sp in one case (12.5 %) and methicilin-resistent Staphylococcus aureus (MRSA) in one (12.5%). Other Gram negative bacilli producers of extended spectrum betalactamase (ESBL) were isolated in two cases (25%) and Stenotrophomonas maltophilia in another (12.5%). CONCLUSIONS: The incidence rate of ventilation-associated pneumonia revealed a tendency to considerable reduction after the utilization of the prophylaxis protocol, while the results suggest no impact on mortality rates. Further prospective evaluation of a greater sample is required, in order to get to definite conclusions regarding prognosis. The isolated germs were, in its majority, high risk pathogens to multiresistance to antibiotics, pointing the necessity of knowledge of local susceptibility profile, so that an adequate initial therapeutic strategy can be undertaken.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):342-347
DOI 10.1590/S0103-507X2007000300013
BACKGROUND AND OBJECTIVES: Care in the intensive care unit (ICU) is constantly challenged by infections related to invasive procedures, which result in increased morbidity and mortality, hospitalization term and costs. This study aimed to prospectively evaluate critical patients according to age, clinical conditions, hospitalization term, occurrence of hospital infection, topography of hospital infection, occurrence of microbial multi-resistance or not, use of invasive procedures and antimicrobial agents. METHODS: This is a prospective, observational, clinical research, carried out at an ICU between February and July 2006. The research subjects were critical patients hospitalized for more than 24 hours at the ICU, followed from admission until discharge, transference or death. RESULTS: The study group consisted of 71 patients with a mean age of 53.5 ± 18.75 years. Forty-seven of these patients (66.2%) acquired hospital infection. Twenty-nine infections (37.6%) occurred in the blood stream, 20 (26%) respiratory and 13 (16.9%) urinary. The most frequent multi-resistant strains were: 14 (10.85%) Pseudomonas aeruginosa, 4 (3.1%) coagulase-negative Staphylococcus sp and 4 (3.1%) Staphylococcus aureus. The most used antimicrobial agents were carbapenem (22.4%), glycopeptides (21.6%) and cephalosporin (21.6%). Twenty-nine (40.8%) of these patients died. CONCLUSIONS: Hospital infection is aggravated if associated to the increased resistance of the microorganisms to the antibiotics.