Abstract
Rev Bras Ter Intensiva. 2013;25(2):130-136
DOI 10.5935/0103-507X.20130024
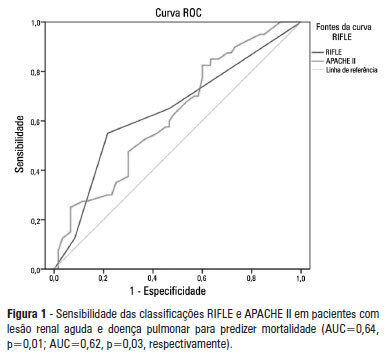
OBJECTIVE: To examine the factors associated with acute kidney injury and outcome in patients with lung disease. METHODS: A prospective study was conducted with 100 consecutive patients admitted to a respiratory intensive care unit in Fortaleza (CE), Brazil. The risk factors for acute kidney injury and mortality were investigated in a group of patients with lung diseases. RESULTS: The mean age of the study population was 57 years, and 50% were male. The incidence of acute kidney injury was higher in patients with PaO2/FiO2<200 mmHg (54% versus 23.7%; p=0.02). Death was observed in 40 cases and the rate of mortality of the acute kidney injury group was higher (62.8% versus 27.6%; p=0.01). The independent factor that was found to be associated with acute kidney injury was PaO2/FiO2<200 mmHg (p=0.01), and the independent risk factors for death were PEEP at admission (OR: 3.6; 95%CI: 1.3-9.6; p=0.009) and need for hemodialysis (OR: 7.9; 95%CI: 2.2-28.3; p=0.001). CONCLUSION: There was a higher mortality rate in the acute kidney injury group. Increased mortality was associated with mechanical ventilation, high PEEP, urea and need for dialysis. Further studies must be performed to better establish the relationship between kidney and lung injury and its impact on patient outcome.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):87-92
DOI 10.5935/0103-507X.20130018
OBJECTIVES: To evaluate the incidence of constipation in critical patients on enteral nutrition in a hospital intensive care unit and to correlate this incidence with the variables found for critical patients. METHODS: The present investigation was a retrospective analytical study conducted in the intensive care unit of Hospital Regional da Asa Norte (DF) via the analysis of medical records of patients admitted during the period from January to December 2011. Data on the incidence of constipation and enteral nutritional support, gastrointestinal changes, stool frequency, ventilatory support, and outcomes were collected and analyzed. RESULTS: The initial sample consisted of 127 patients admitted to the unit during the period from January to December 2011. Eighty-four patients were excluded, and the final sample consisted of 43 patients. The incidence of constipation, defined as no bowel movement during the first 4 days of hospitalization, was 72% (n=31). The patients were divided into a control group and a constipated group. The group of constipated patients reached the caloric target, on average, at 6.5 days, and the control group reached the caloric target in 5.6 days (p=0.51). Constipation was not associated with the length of hospital stay, suspension of nutritional support, or outcome of hospitalization. There was an association between evacuation during hospitalization and a longer duration of hospitalization for a subgroup of patients who did not evacuate during the entire period (p=0.009). CONCLUSION: The incidence of constipation in the unit studied was 72%. Only the absence of evacuation during hospitalization was associated with longer hospital stays. Constipation was not associated with the length of hospital stay, suspension of nutritional support, or outcome of hospitalization.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):93-98
DOI 10.5935/0103-507X.20130019
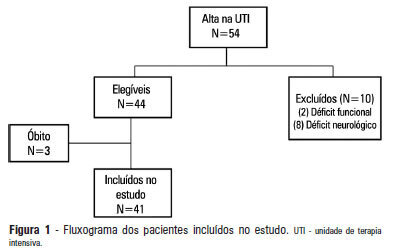
OBJECTIVE: 1) To evaluate the functional independence measures immediately after discharge from an intensive care unit and to compare these values with the FIMs 30 days after that period. 2) To evaluate the possible associated risk factors. METHODS: The present investigation was a prospective cohort study that included individuals who were discharged from the intensive care unit and underwent physiotherapy in the unit. Functional independence was evaluated using the functional independence measure immediately upon discharge from the intensive care unit and 30 days thereafter via a phone call. The patients were admitted to the Hospital Santa Clara intensive care unit during the period from May 2011 to August 2011. RESULTS: During the predetermined period of data collection, 44 patients met the criteria for inclusion in the study. The mean age of the patients was 55.4±10.5 years. Twenty-seven of the subjects were female, and 15 patients were admitted due to pulmonary disease. The patients exhibited an functional independence measure of 84.1±24.2. When this measure was compared to the measure at 30 days after discharge, there was improvement across the functional independence variables except for that concerned with sphincter control. There were no significant differences when comparing the gender, age, clinical diagnosis, length of stay in the intensive care unit, duration of mechanical ventilation, and the presence of sepsis during this period. CONCLUSION: Functional independence, as evaluated by the functional independence measure scale, was improved at 30 days after discharge from the intensive care unit, but it was not possible to define the potentially related factors.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):99-105
DOI 10.5935/0103-507X.20130020
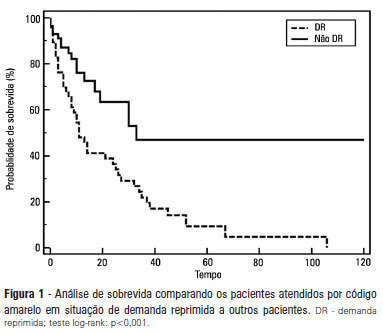
OBJECTIVE: To describe the epidemiological data of the clinical instability events in patients attended to by the rapid response team and to identify prognostic factors. METHODS: This was a longitudinal study, performed from January to July 2010, with an adult inpatient population in a hospital environment. The data collected regarding the code yellow service included the criteria of the clinical instability, the drug and non-drug therapies administered and the activities and procedures performed. The outcomes evaluated were the need for intensive care unit admission and the hospital mortality rates. A level of p=0.05 was considered to be significant. RESULTS: A total of 150 code yellow events that occurred in 104 patients were evaluated. The most common causes were related to acute respiratory insufficiency with hypoxia or a change in the respiratory rate and a concern of the team about the patient's clinical condition. It was necessary to request a transfer to the intensive care unit in 80 of the 150 cases (53.3%). It was necessary to perform 42 procedures. The most frequent procedures were orotracheal intubation and the insertion of a central venous catheter. The patients who were in critical condition and had to wait for an intensive care unit bed had a higher risk of death compared to the other patients (hazard ratio: 3.12; 95% CI: 1.80-5.40; p<0.001). CONCLUSIONS: There are patients in critical condition that require expert intensive care in the regular ward unit hospital beds. The events that most frequently led to the code yellow activation were related to hemodynamic and respiratory support. The interventions performed indicate the need for a physician on the team. The situation of pent-up demand is associated with a higher mortality rate.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):106-114
DOI 10.5935/0103-507X.20130021
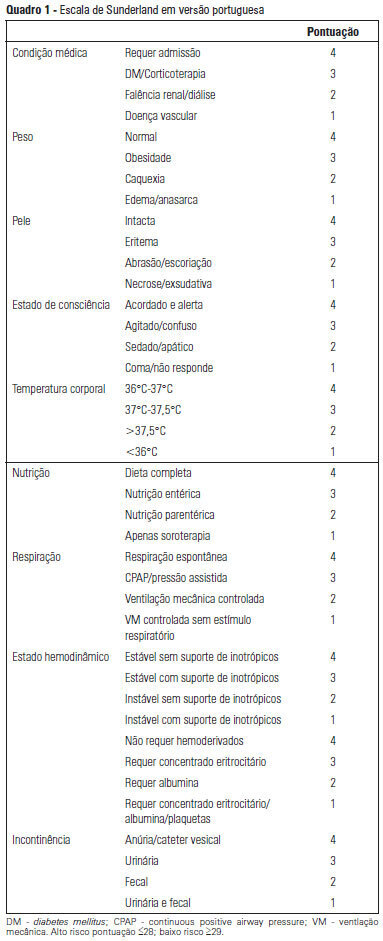
OBJECTIVE: To Translate into Portuguese and evaluate the measuring properties of the Sunderland Scale and the Cubbin & Jackson Revised Scale, which are instruments for evaluating the risk of developing pressure ulcers during intensive care. METHODS: This study included the process of translation and adaptation of the scales to the Portuguese language, as well as the validation of these tools. To assess the reliability, Cronbach alpha values of 0.702 to 0.708 were identified for the Sunderland Scale and the Cubbin & Jackson Revised Scale, respectively. The validation criteria (predictive) were performed comparatively with the Braden Scale (gold standard), and the main measurements evaluated were sensitivity, specificity, positive predictive value, negative predictive value, and area under the curve, which were calculated based on cutoff points. RESULTS: The Sunderland Scale exhibited 60% sensitivity, 86.7% specificity, 47.4% positive predictive value, 91.5% negative predictive value, and 0.86 for the area under the curve. The Cubbin & Jackson Revised Scale exhibited 73.3% sensitivity, 86.7% specificity, 52.4% positive predictive value, 94.2% negative predictive value, and 0.91 for the area under the curve. The Braden scale exhibited 100% sensitivity, 5.3% specificity, 17.4% positive predictive value, 100% negative predictive value, and 0.72 for the area under the curve. CONCLUSIONS: Both tools demonstrated reliability and validity for this sample. The Cubbin & Jackson Revised Scale yielded better predictive values for the development of pressure ulcers during intensive care.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):115-122
DOI 10.5935/0103-507X.20130022
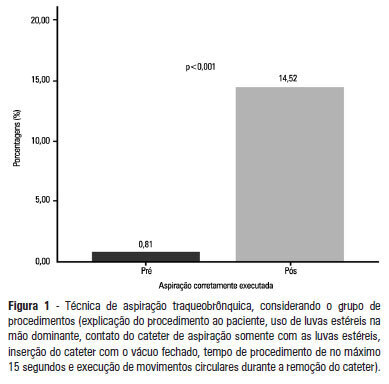
OBJECTIVE: To evaluate the effectiveness of an educational intervention on healthcare professionals' adherence to the technical recommendations for tracheobronchial aspiration in intensive care unit patients. METHODS: A quasi-experimental study was performed to evaluate intensive care unit professionals' adherence to the tracheobronchial aspiration technical recommendations in intensive care unit patients both before and after a theoretical and practical educational intervention. Comparisons were performed using the chi-square test, and the significance level was set to p<0.05. RESULTS: A total of 124 procedures, pre- and post-intervention, were observed. Increased adherence was observed in the following actions: the use of personal protective equipment (p=0.01); precaution when opening the catheter package (p<0.001); the use of a sterile glove on the dominant hand to remove the catheter (p=0.003); the contact of the sterile glove with the catheter only (p<0.001); the execution of circular movements during the catheter removal (p<0.001); wrapping the catheter in the sterile glove at the end of the procedure (p=0.003); the use of distilled water, opened at the start of the procedure, to wash the connection latex (p=0.002); the disposal of the leftover distilled water at the end of the procedure (p<0.001); and the performance of the aspiration technique procedures (p<0.001). CONCLUSION: There was a low adherence by health professionals to the preventive measures against hospital infection, indicating the need to implement educational strategies. The educational intervention used was shown to be effective in increasing adherence to the technical recommendations for tracheobronchial aspiration.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):39-43
DOI 10.1590/S0103-507X2013000100008
OBJECTIVE: The objective of this study was to use a cycle ergometer to assess cardiorespiratory changes during active exercise and to verify patients' satisfaction with this type of activity. METHODS: A single intervention involving active lower limb exercise was performed with a cycle ergometer (without load) for 5 minutes. The following variables were measured before, during and immediately after exercise: heart rate, blood pressure, respiratory rate, peripheral oxygen saturation and the Borg dyspnea scale score. Following the exercise, the patients answered a questionnaire to evaluate their satisfaction with this type of activity. RESULTS: A total of 38 patients (65% male) with a mean age of 48 ± 16 years old participated in the study. Enrolled patients presented a sequential organ failure assessment (SOFA) score of 2 (0 - 5 scale). During the exercise, 16% of the patients used ventilation support and 55% of them were breathing at room air. A comparison of the initial and final values of the variables indicated increases in the heart rate (92±17 beats/min vs. 95±18 beats/min; p<0.05), the respiratory rate (19 ± 8 breaths/min vs. 23±8 breaths/min; p<0.05) and the Borg dyspnea scale score (1.3±1.8 vs. 2.8±2.2; p<0.05). In addition, 85% of the patients reported enjoying the activity. Only 25% of the patients reported some discomfort, and 100% of the patients wanted to repeat this type of activity in future treatments. CONCLUSION: During the cycle ergometer exercises, minor cardiorespiratory changes were observed in the patients. The evaluated patients reported high satisfaction with this type of activity.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98) Septic shock (25)