You searched for:"Ruy Camargo Pires-Neto"
We found (3) results for your search.-
Editorial
Awaking, exercising, sitting, walking and extubating: moving on the paradigms for mechanically ventilated patients
Rev Bras Ter Intensiva. 2014;26(3):203-204
Abstract
EditorialAwaking, exercising, sitting, walking and extubating: moving on the paradigms for mechanically ventilated patients
Rev Bras Ter Intensiva. 2014;26(3):203-204
DOI 10.5935/0103-507X.20140030
Views0In the intensive care unit (ICU) patients are exposed to catheters, tubes, alarms and noise, and they experience thirst, hunger, immobility and several other sources of discomfort. How hostile is the ICU environment to patients and to caregivers? It is intuitive to put patients to sleep while they stay in this inhospitable place for life […]See more -
Original Articles
Ineffectiveness of using the pressure relief valve technique during cuff inflation
Rev Bras Ter Intensiva. 2014;26(4):367-372
Abstract
Original ArticlesIneffectiveness of using the pressure relief valve technique during cuff inflation
Rev Bras Ter Intensiva. 2014;26(4):367-372
DOI 10.5935/0103-507X.20140056
Views0Objective:
To test the effectiveness of using a cuff pressure relief valve technique to maintain cuff pressure levels within the normal in vitro range (Phase 1) in patients admitted to the intensive care unit (Phase 2) and to test the reproducibility of the technique using different syringes.
Methods:
In Phase 1, a tracheal tube was inserted into a trachea model. Ten- and 20mL syringes were used to inflate the cuff through the tracheal tube. The cuff was slowly and steadily inflated until the syringe plunger would move in the opposite direction of the application. After the plunger stopped, the cuff pressures were recorded. In Phase 2, the same maneuvers for inflating the cuff were performed on 20 patients using 5, 10, and 20mL syringes and were compared with manometer measurements. The intraclass correlation coefficient and Bland-Altman analysis were employed to determine the reproducibility and agreement between syringes. Data were expressed as medians (interquartile range).
Results:
There was no reproducibility between syringes with an intraclass correlation coefficient ranging between -0.33 and 0.8 (p>0.05). The pressures generated with the syringes were higher than the pressures generated using a standard manometer: the 5mL syringe pressure was 105cmH2O (82.5-120cmH2O), the 10mL syringe pressure was 69cmH2O (47.5-111.3cmH2O), and the 20mL syringe pressure was 45cmH2O (35-59.5cmH2O). The Bland-Altman analysis confirmed the large bias and variability between the syringes used, compared with the manometer.
Conclusion:
The use of syringes is not an effective technique for determining the cuff pressure in patients admitted to the intensive care unit.
Keywords:Airway managementIntensive care unitsIntubation, intratrachealRespiration, artificialRespiratory therapyTransducers, pressureSee more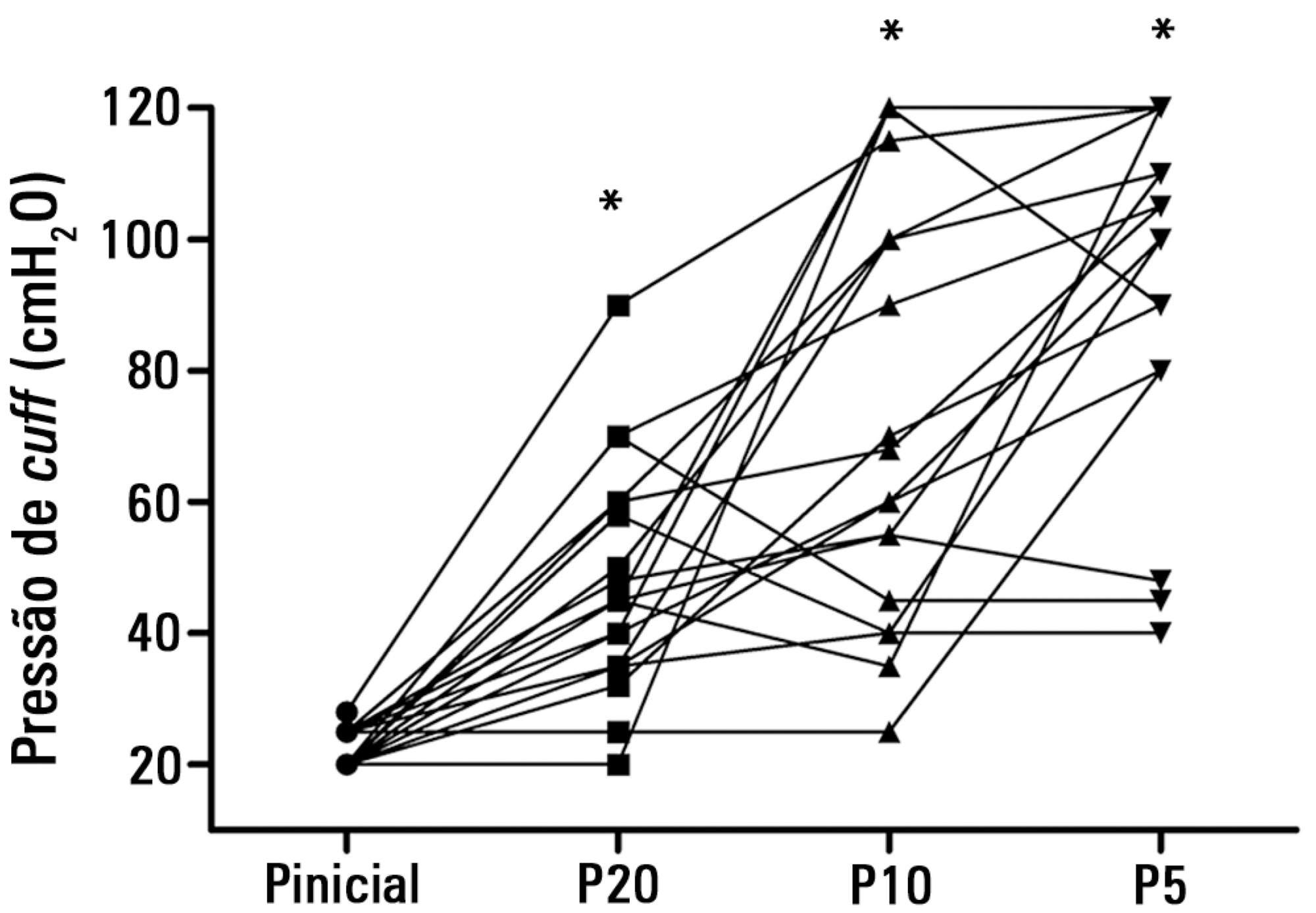
-
Original Articles – Clinical Research
Characterization of the use of a cycle ergometer to assist in the physical therapy treatment of critically ill patients
Rev Bras Ter Intensiva. 2013;25(1):39-43
Abstract
Original Articles – Clinical ResearchCharacterization of the use of a cycle ergometer to assist in the physical therapy treatment of critically ill patients
Rev Bras Ter Intensiva. 2013;25(1):39-43
DOI 10.1590/S0103-507X2013000100008
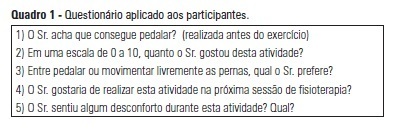
Views0See moreOBJECTIVE: The objective of this study was to use a cycle ergometer to assess cardiorespiratory changes during active exercise and to verify patients’ satisfaction with this type of activity. METHODS: A single intervention involving active lower limb exercise was performed with a cycle ergometer (without load) for 5 minutes. The following variables were measured before, during and immediately after exercise: heart rate, blood pressure, respiratory rate, peripheral oxygen saturation and the Borg dyspnea scale score. Following the exercise, the patients answered a questionnaire to evaluate their satisfaction with this type of activity. RESULTS: A total of 38 patients (65% male) with a mean age of 48 ± 16 years old participated in the study. Enrolled patients presented a sequential organ failure assessment (SOFA) score of 2 (0 – 5 scale). During the exercise, 16% of the patients used ventilation support and 55% of them were breathing at room air. A comparison of the initial and final values of the variables indicated increases in the heart rate (92±17 beats/min vs. 95±18 beats/min; p<0.05), the respiratory rate (19 ± 8 breaths/min vs. 23±8 breaths/min; p<0.05) and the Borg dyspnea scale score (1.3±1.8 vs. 2.8±2.2; p<0.05). In addition, 85% of the patients reported enjoying the activity. Only 25% of the patients reported some discomfort, and 100% of the patients wanted to repeat this type of activity in future treatments. CONCLUSION: During the cycle ergometer exercises, minor cardiorespiratory changes were observed in the patients. The evaluated patients reported high satisfaction with this type of activity.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




