Abstract
Rev Bras Ter Intensiva. 2022;34(3):380-385
DOI 10.5935/0103-507X.20220224-en
To determine the incidence of postintensive care syndrome in a cohort of critically ill patients admitted to the intensive care unit and to identify risk factors related to its development in the physical, cognitive and mental health areas.
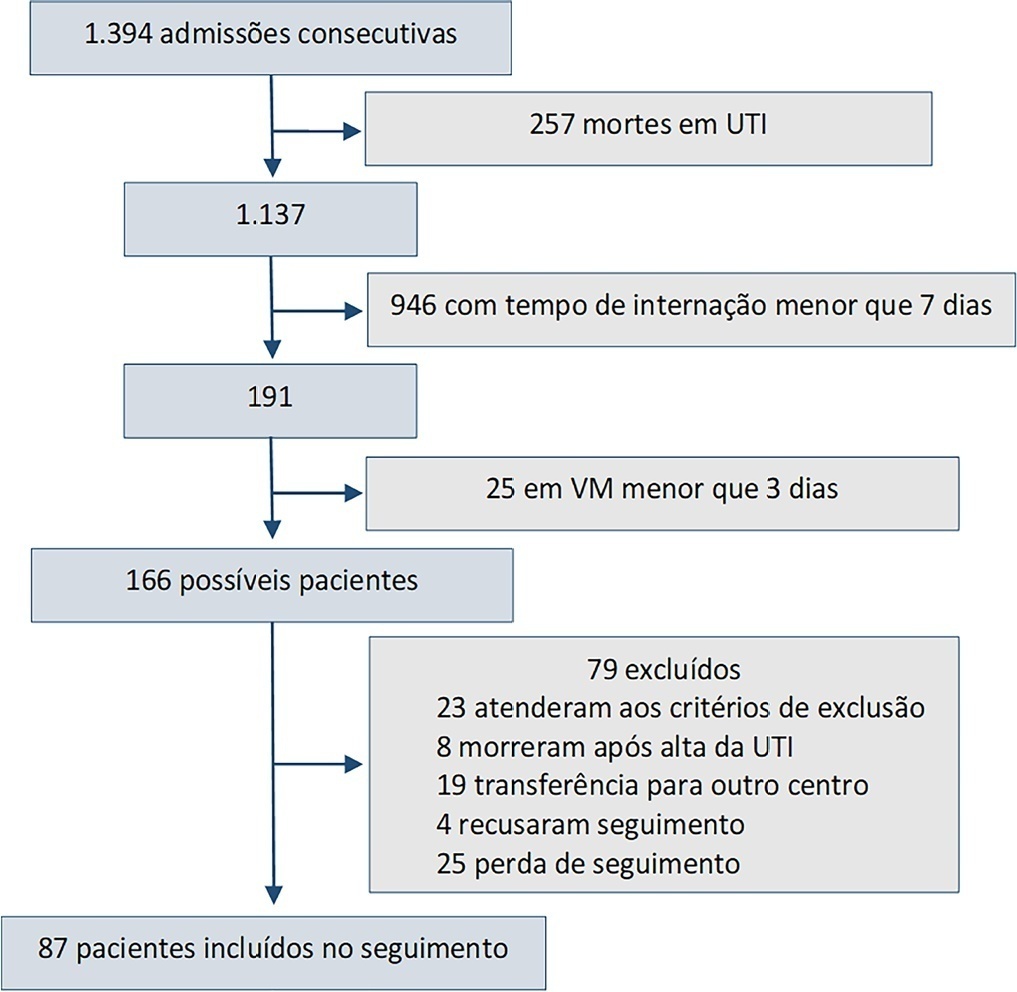
This was a prospective observational cohort study developed in the intensive care unit of a university hospital. Patients with intensive care unit stays equal to or longer than one week and the need for mechanical ventilation for more than 3 days, shock or delirium were included in the study. Demographic variables, reasons for admission, diagnoses, sedation, type of mechanical ventilation used, complications and length of stay were recorded. A univariate analysis was performed to identify risk factors related to postintensive care syndrome. The scales used for the assessment of the different spheres were Barthel, Pfeiffer, Hospital Anxiety and Depression Scale and Impact of Event Scale-6. The main variables of interest were postintensive care syndrome incidence overall and by domains. Risk factors were examined in each of the health domains (physical, cognitive and mental health).
Eighty-seven patients were included. The mean Acute Physiology and Chronic Health Evaluation II score was 16.5. The mean number of intensive care unit days was 17. The incidence of global postintensive care syndrome was 56.3% (n = 49, 95%CI 45.8 - 66.2%). The incidence of postintensive care syndrome in each of the spheres was 32.1% (physical), 11.5% (cognitive), and 36.6% (mental health).
The incidence of postintensive care syndrome is 56.3%. The mental health sphere is the most frequently involved. The risk factors are different depending on the area considered.
Abstract
Rev Bras Ter Intensiva. 2022;34(1):131-140
DOI 10.5935/0103-507X.20220007-en
To evaluate the incidence of risk factors for postintubation hypotension in critically ill patients with COVID-19.
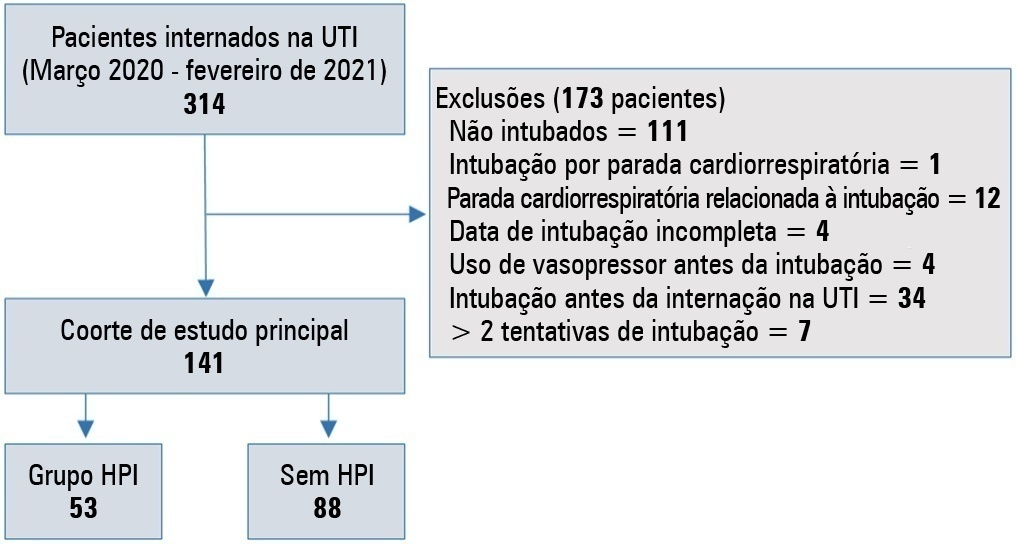
We conducted a retrospective study of 141 patients with COVID-19 who were intubated in the intensive care unit. Postintubation hypotension was defined as the need for any vasopressor dose at any time within the 60 minutes following intubation. Patients with intubation-related cardiac arrest and hypotension before intubation were excluded from the study.
Of the 141 included patients, 53 patients (37.5%) had postintubation hypotension, and 43.6% of the patients (n = 17) were female. The median age of the postintubation hypotension group was 75.0 (interquartile range: 67.0 - 84.0). In the multivariate analysis, shock index ≥ 0.90 (OR = 7.76; 95%CI 3.14 - 19.21; p < 0.001), albumin levels < 2.92g/dL (OR = 3.65; 95%CI 1.49 - 8.96; p = 0.005), and procalcitonin levels (OR = 1.07, 95%CI 1.01 - 1.15; p = 0.045) were independent risk factors for postintubation hypotension. Hospital mortality was similar in patients with postintubation hypotension and patients without postintubation hypotension (92.5% versus 85.2%; p = 0.29).
The incidence of postintubation hypotension was 37.5% in critically ill COVID-19 patients. A shock index ≥ 0.90 and albumin levels < 2.92g/dL were independently associated with postintubation hypotension. Furthermore, a shock index ≥ 0.90 may be a practical tool to predict the increased risk of postintubation hypotension in bedside scenarios before endotracheal intubation. In this study, postintubation hypotension was not associated with increased hospital mortality in COVID-19 patients.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):125-137
DOI 10.5935/0103-507X.20210014
To study the impact of delayed admission by more than 4 hours on the outcomes of critically ill patients.
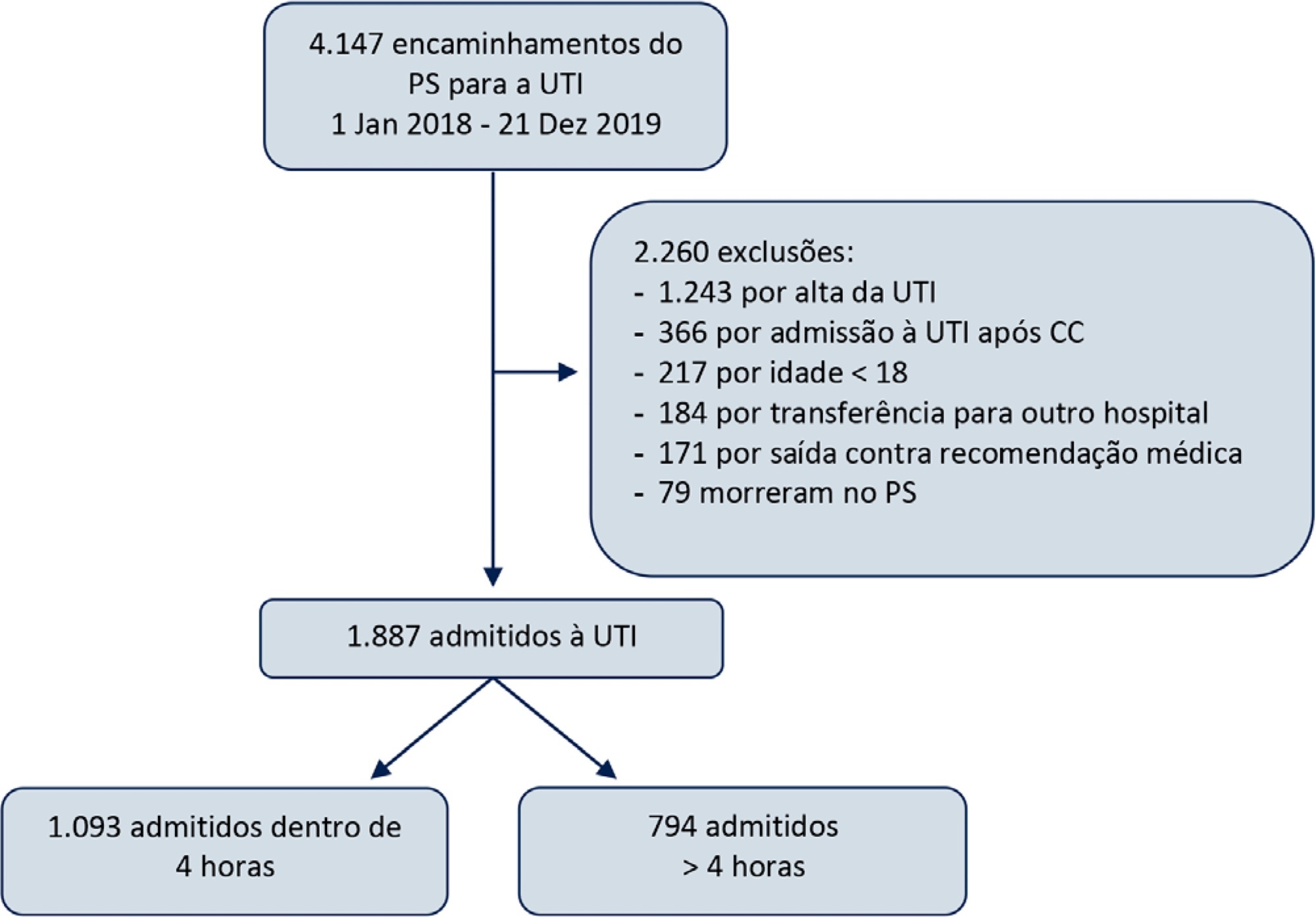
This was a retrospective observational study in which adult patients admitted directly from the emergency department to the intensive care unit were divided into two groups: Timely Admission if they were admitted within 4 hours and Delayed Admission if admission was delayed for more than 4 hours. Intensive care unit length of stay and hospital/intensive care unit mortality were compared between the groups. Propensity score matching was performed to correct for imbalances. Logistic regression analysis was used to explore delayed admission as an independent risk factor for intensive care unit mortality.
During the study period, 1,887 patients were admitted directly from the emergency department to the intensive care unit, with 42% being delayed admissions. Delayed patients had significantly longer intensive care unit lengths of stay and higher intensive care unit and hospital mortality. These results were persistent after propensity score matching of the groups. Delayed admission was an independent risk factor for intensive care unit mortality (OR = 2.6; 95%CI 1.9 - 3.5; p < 0.001). The association of delay and intensive care unit mortality emerged after a delay of 2 hours and was highest after a delay of 4 hours.
Delayed admission to the intensive care unit from the emergency department is an independent risk factor for intensive care unit mortality, with the strongest association being after a delay of 4 hours.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):111-118
DOI 10.5935/0103-507X.20210012
To evaluate the incidence of hypothermia in patients undergoing continuous renal replacement therapy in the intensive care unit. As secondary objectives, we determined associated factors and compared the occurrence of hypothermia between two modalities of continuous renal replacement therapy.
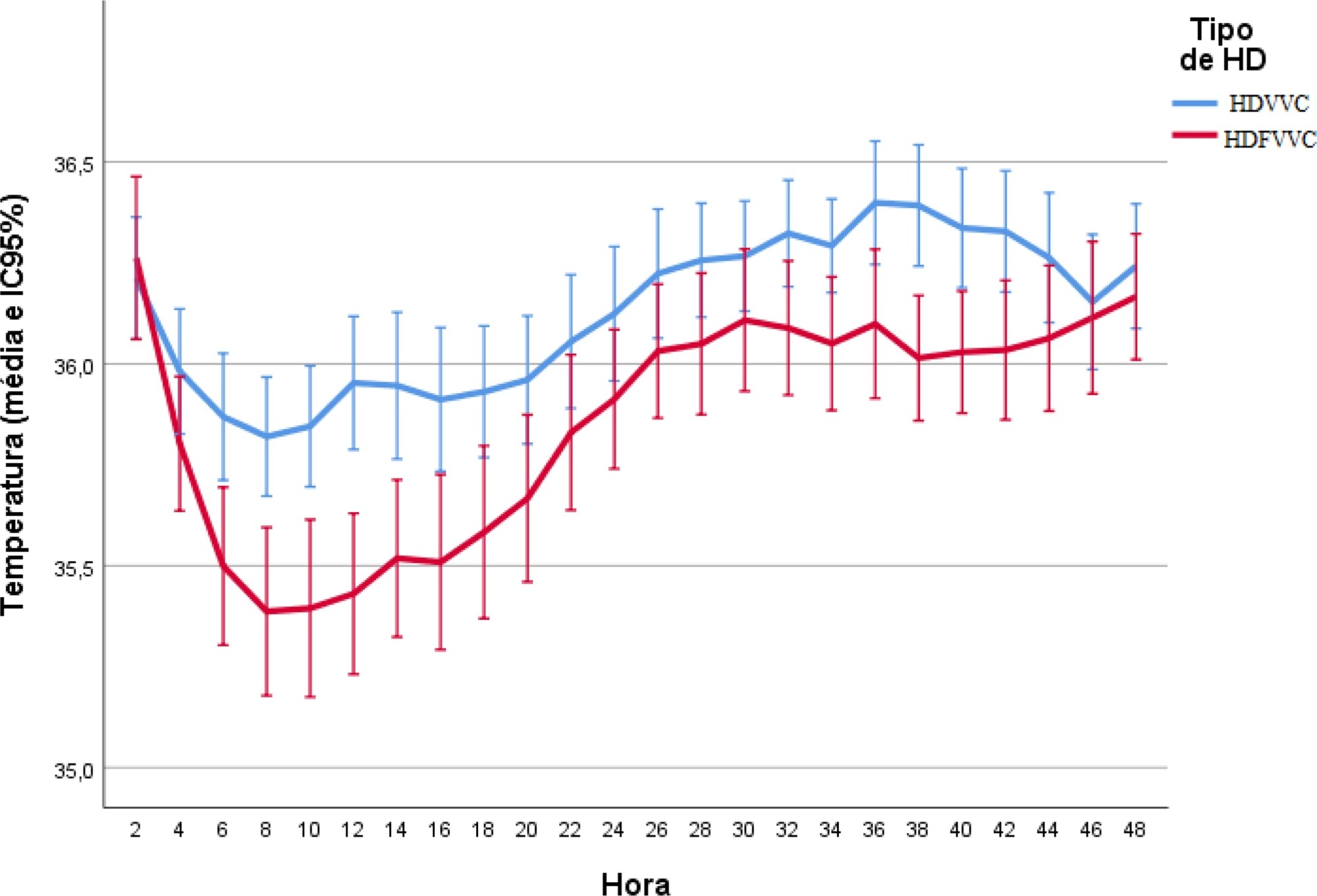
A prospective cohort study was conducted with adult patients who were admitted to a clinical-surgical intensive care unit and underwent continuous renal replacement therapy in a high-complexity public university hospital in southern Brazil from April 2017 to July 2018. Hypothermia was defined as a body temperature ≤ 35ºC. The patients included in the study were followed for the first 48 hours of continuous renal replacement therapy. The researchers collected data from medical records and continuous renal replacement therapy records.
A total of 186 patients were equally distributed between two types of continuous renal replacement therapy: hemodialysis and hemodiafiltration. The incidence of hypothermia was 52.7% and was higher in patients admitted for shock (relative risk of 2.11; 95%CI 1.21 - 3.69; p = 0.009) and in those who underwent hemodiafiltration with heating in the return line (relative risk of 1.50; 95%CI 1.13 - 1.99; p = 0.005).
Hypothermia in critically ill patients with continuous renal replacement therapy is frequent, and the intensive care team should be attentive, especially when there are associated risk factors.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):487-492
DOI 10.5935/0103-507X.20200082
This study aims to describe the clinical characteristics and predictors of mechanical ventilation of adult inpatients with COVID-19 in a single center.
A retrospective cohort study was performed and included adult inpatients hospitalized from March 17th to May 3rd, 2020, who were diagnosed with SARS-CoV-2 infection. Clinical and demographic characteristics were extracted from electronic medical records.
Overall, 88 consecutive patients were included in this study. The median age of the patients was 63 years (IQR 49 - 71); 59 (67%) were male, 65 (86%) had a college degree and 67 (76%) had at least one comorbidity. Twenty-nine (33%) patients were admitted to the intensive care unit, 18 (20%) patients needed mechanical ventilation, and 9 (10.2%) died during hospitalization. The median length of stay in the intensive care unit and the median duration of mechanical ventilation was 23 and 29.5 days, respectively. An age ≥ 65 years was an independent risk factor for mechanical ventilation (OR 8.4 95%CI 1.3 - 55.6 p = 0.02).
Our findings describe the first wave of Brazilian patients hospitalized for COVID-19. Age was the strongest predictor of respiratory insufficiency and the need for mechanical ventilation in our population.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):261-267
DOI 10.5935/0103-507X.20200042
To evaluate the functional status of pediatric patients undergoing congenital heart surgery after discharge from the intensive care unit, and to evaluate the correlations among clinical variables, functional status and surgical risk.
Cross-sectional study including patients aged 1 month to less than 18 years undergoing congenital heart surgery between October 2017 and May 2018. Functional outcome was assessed by the Functional Status Scale, surgical risk classification was determined using the Risk Adjustment for Congenital Heart Surgery-1 (RACHS-1), and clinical variables were collected from electronic medical records.
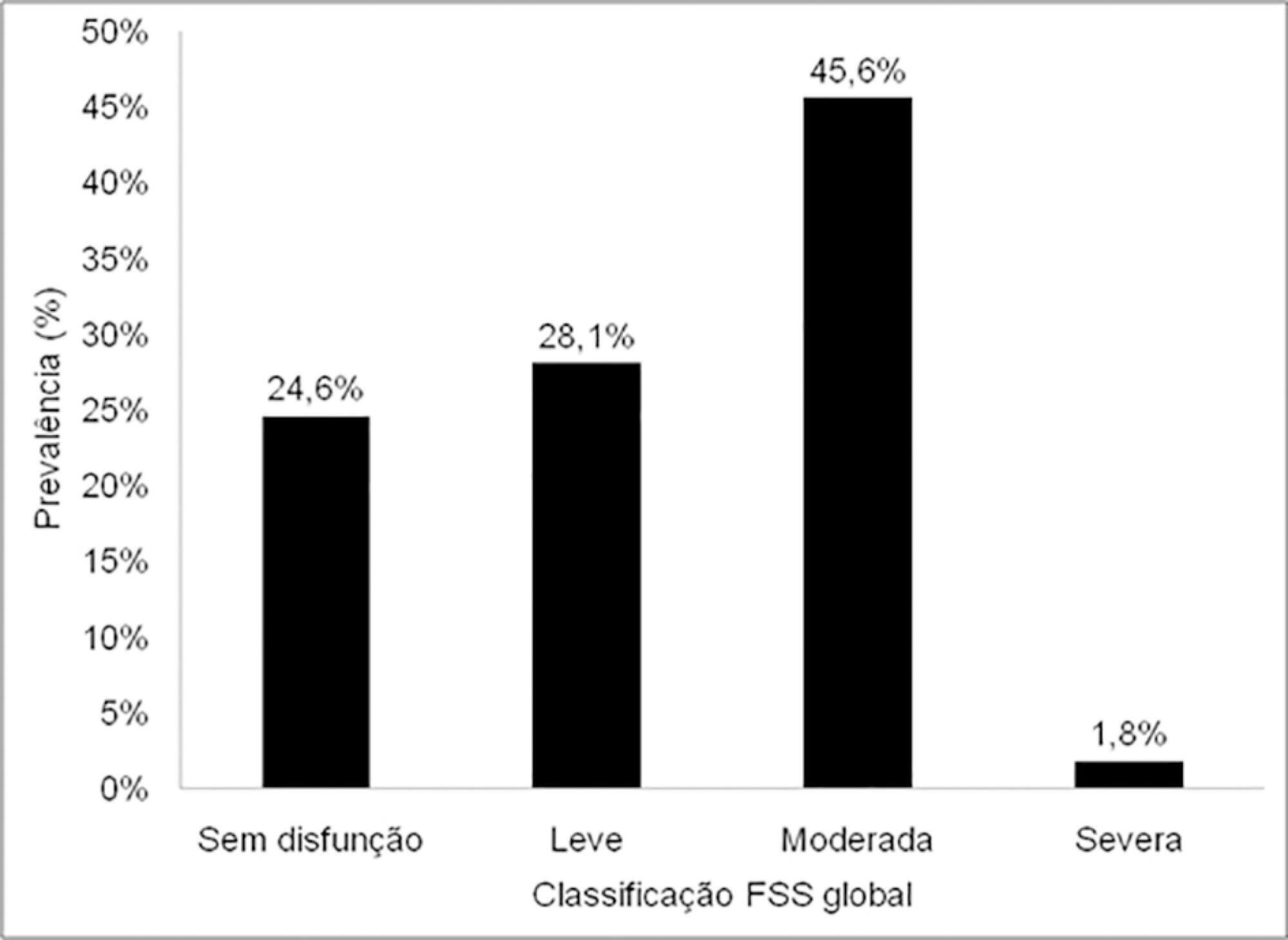
The sample comprised 57 patients with a median age of 7 months (2 - 17); 54.4% were male, and 75.5% showed dysfunction, which was moderate in 45.6% of the cases. RACHS-1 category > 3 was observed in 47% of the sample, indicating higher surgical risk. There was a correlation between functional deficit and younger age, longer duration of invasive mechanical ventilation and longer intensive care unit stay. Moreover, greater functional deficit was observed among patients classified as RACHS-1 category > 3.
The prevalence of functional deficit was high among children and adolescents with congenital heart disease after cardiac surgery. Higher surgical risk, longer duration of invasive mechanical ventilation, longer intensive care unit stay and younger age were correlated with worse functional status.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):43-48
DOI 10.5935/0103-507X.20200008
To determine the independent risk factors associated with mortality in adult burn patients.
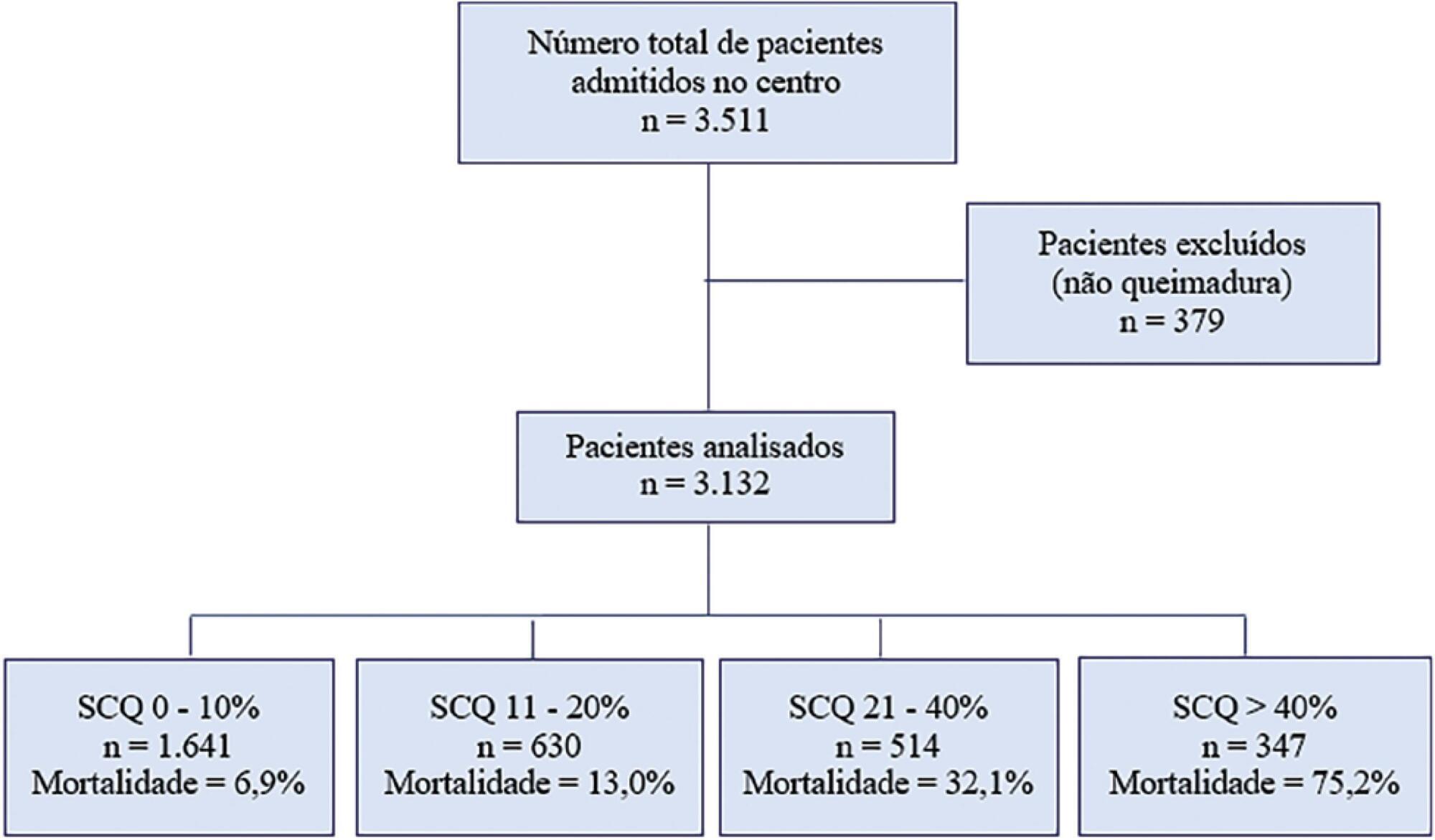
This was a retrospective, observational study performed at the Centro Nacional de Queimados do Uruguai. All patients with skin burns admitted to the unit since its opening on July 1, 1995 through December 31, 2018 were included. The demographic data, burn profiles, length of stay, mechanical ventilation duration and hospital mortality were studied. A multivariate logistic regression was used to identify the risk factors for mortality. The standardized mortality ratio was calculated by dividing the number of observed deaths by the number of expected deaths (according to the Abbreviated Burn Severity Index).
During the study period, 3,132 patients were included. The median total body surface area burned was 10% (3%-22%). The Abbreviated Burn Severity Index was 6 (4 - 7). Invasive mechanical ventilation was required in 60% of the patients for a median duration of 6 (3 - 16) days. The median length of stay in the unit was 17 (7 - 32) days. The global mortality was 19.9%. Crude mortality and standardized mortality ratio decreased from 1995 through 2018. The global standardized mortality ratio was 0.99. A need for mechanical ventilation (OR 8.80; 95%CI 5.68 - 13.62), older age (OR 1.07 per year; 95%CI 1.06 - 1.09), total body surface area burned (OR 1.05 per 1%; 95%CI 1.03 - 1.08) and extension of third-degree burns (OR 1.05 per 1%; 95%CI 1.03 - 1.07) were independent risk factors for mortality.
The need for mechanical ventilation, older age and burn extension were independent risk factors for mortality in the burned adult Uruguayan population.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98) Septic shock (25)