Abstract
Rev Bras Ter Intensiva. 2021;33(1):111-118
DOI 10.5935/0103-507X.20210012
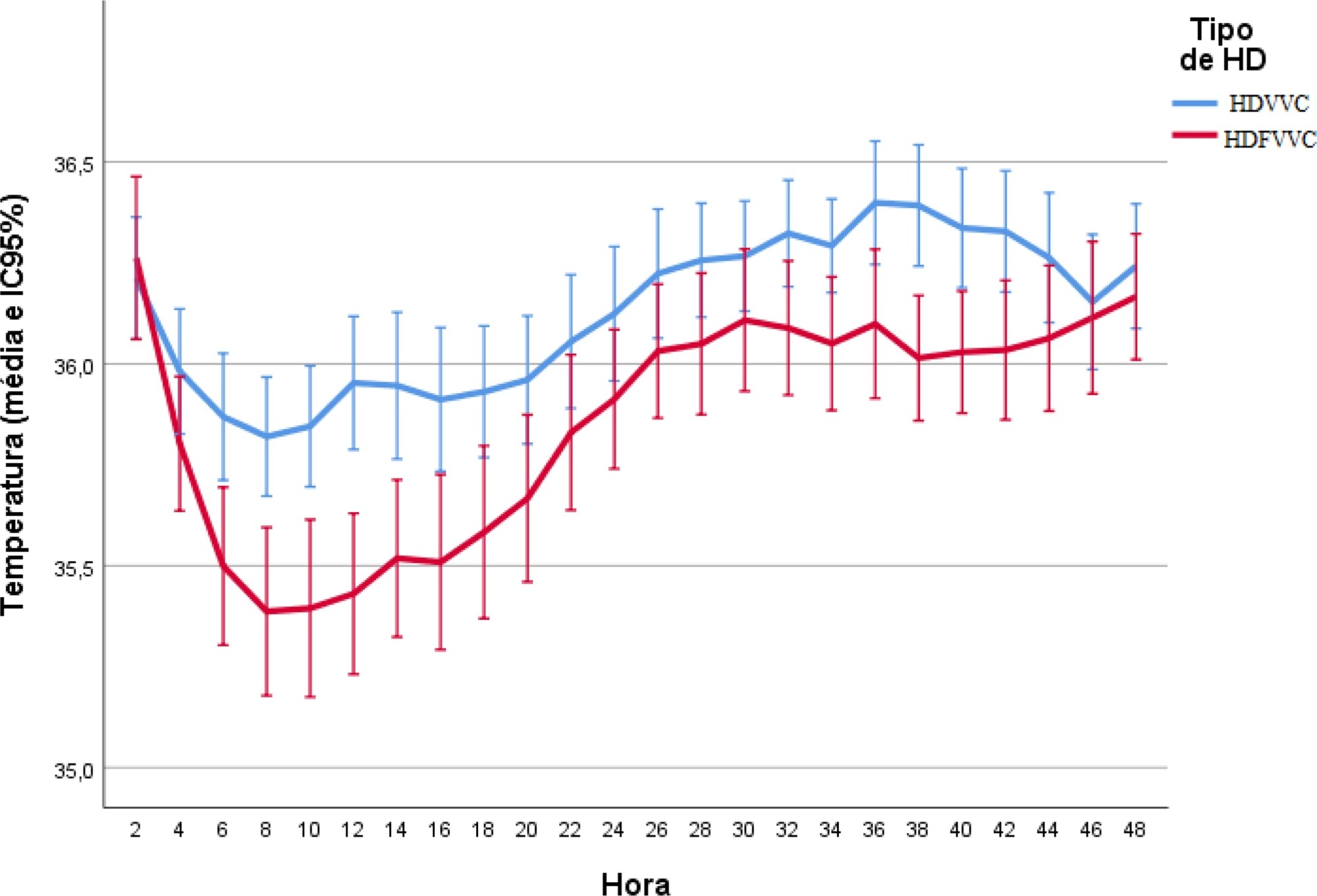
To evaluate the incidence of hypothermia in patients undergoing continuous renal replacement therapy in the intensive care unit. As secondary objectives, we determined associated factors and compared the occurrence of hypothermia between two modalities of continuous renal replacement therapy.
A prospective cohort study was conducted with adult patients who were admitted to a clinical-surgical intensive care unit and underwent continuous renal replacement therapy in a high-complexity public university hospital in southern Brazil from April 2017 to July 2018. Hypothermia was defined as a body temperature ≤ 35ºC. The patients included in the study were followed for the first 48 hours of continuous renal replacement therapy. The researchers collected data from medical records and continuous renal replacement therapy records.
A total of 186 patients were equally distributed between two types of continuous renal replacement therapy: hemodialysis and hemodiafiltration. The incidence of hypothermia was 52.7% and was higher in patients admitted for shock (relative risk of 2.11; 95%CI 1.21 - 3.69; p = 0.009) and in those who underwent hemodiafiltration with heating in the return line (relative risk of 1.50; 95%CI 1.13 - 1.99; p = 0.005).
Hypothermia in critically ill patients with continuous renal replacement therapy is frequent, and the intensive care team should be attentive, especially when there are associated risk factors.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):120-131
DOI 10.5935/0103-507X.20160026
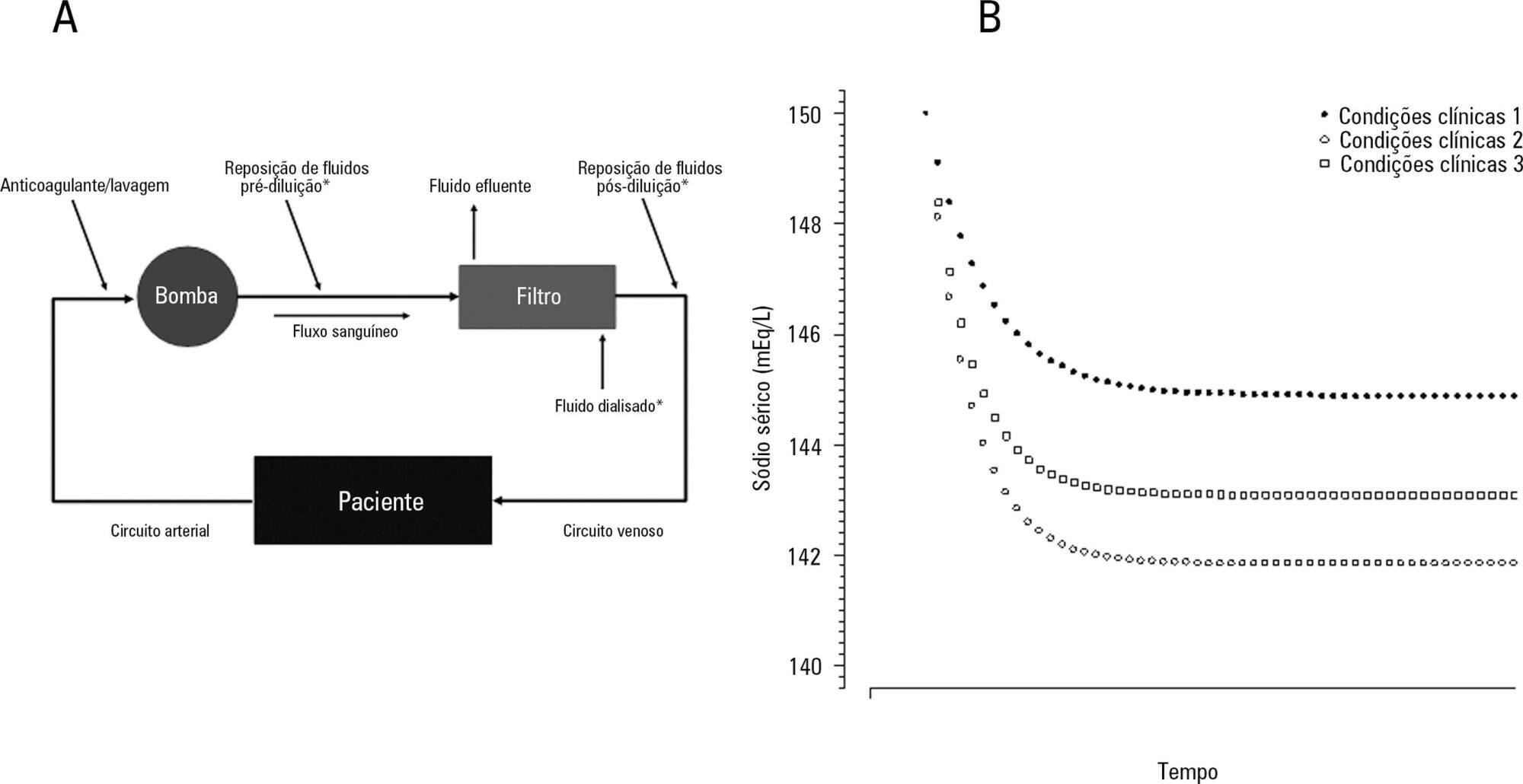
The aim of this study was to investigate the clinical and laboratorial factors associated with serum sodium variation during continuous renal replacement therapy and to assess whether the perfect admixture formula could predict 24-hour sodium variation.
Thirty-six continuous renal replacement therapy sessions of 33 patients, in which the affluent prescription was unchanged during the first 24 hours, were retrieved from a prospective collected database and then analyzed. A mixed linear model was performed to investigate the factors associated with large serum sodium variations (≥ 8mEq/L), and a Bland-Altman plot was generated to assess the agreement between the predicted and observed variations.
In continuous renal replacement therapy 24-hour sessions, SAPS 3 (p = 0.022) and baseline hypernatremia (p = 0.023) were statistically significant predictors of serum sodium variations ≥ 8mEq/L in univariate analysis, but only hypernatremia demonstrated an independent association (β = 0.429, p < 0.001). The perfect admixture formula for sodium prediction at 24 hours demonstrated poor agreement with the observed values.
Hypernatremia at the time of continuous renal replacement therapy initiation is an important factor associated with clinically significant serum sodium variation. The use of 4% citrate or acid citrate dextrose - formula A 2.2% as anticoagulants was not associated with higher serum sodium variations. A mathematical prediction for the serum sodium concentration after 24 hours was not feasible.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):402-405
DOI 10.5935/0103-507X.20150067
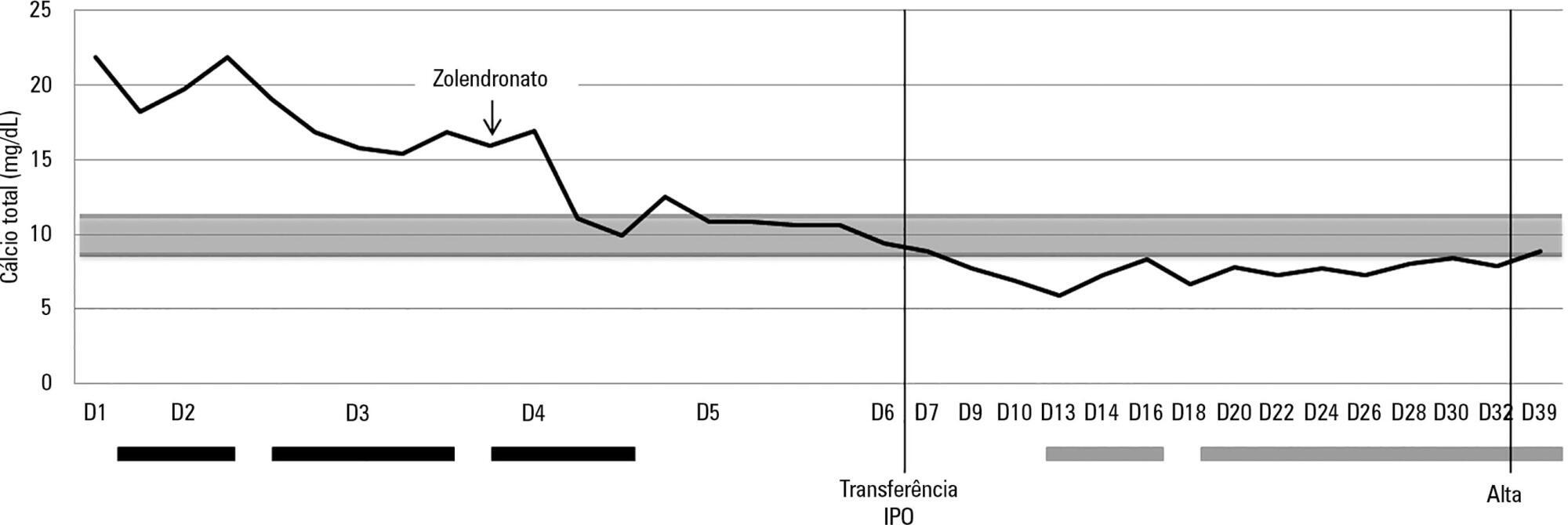
Hypercalcemia is a rare metabolic disorder in children and is potentially fatal. It has a wide differential diagnosis, including cancer. Here, we report the case of a previously healthy 3-year-old who was admitted to the emergency room with fatigue, hyporeactivity, fever and limping gait that had evolved over 5 days and that was progressively worsening. On examination the patient was unconscious (Glasgow coma score: 8). Laboratory tests indicated severe hypercalcemia (total calcium 21.39mg/dL, ionized calcium 2.93mmol/L) and microcytic anemia. Hyperhydration was initiated, and the child was transferred to the pediatric intensive care unit. Continuous venovenous hemodiafiltration with calcium-free solution was instituted, which brought progressive normalization of serum calcium and an improved state of consciousness. Zoledronate was administered, and metabolic and infectious causes and poisoning were excluded. The bone marrow smear revealed a diagnosis of acute lymphoblastic leukemia. Hypercalcemia associated with malignancy in children is rare and occurs as a form of cancer presentation or recurrence. Continuous venovenous hemodiafiltration should be considered in situations where there is imminent risk to life.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)