Abstract
Crit Care Sci. 2023;35(4):402-410
DOI 10.5935/2965-2774.20230174-pt
To describe, with a larger number of patients in a real-world scenario following routine implementation, intensivist-led ultrasound-guided percutaneous dilational tracheostomy and the possible risks and complications of the procedure not identified in clinical trials.
This was a phase IV cohort study of patients admitted to three intensive care units of a quaternary academic hospital who underwent intensivist-led ultrasound-guided percutaneous tracheostomy in Brazil from September 2017 to December 2021.
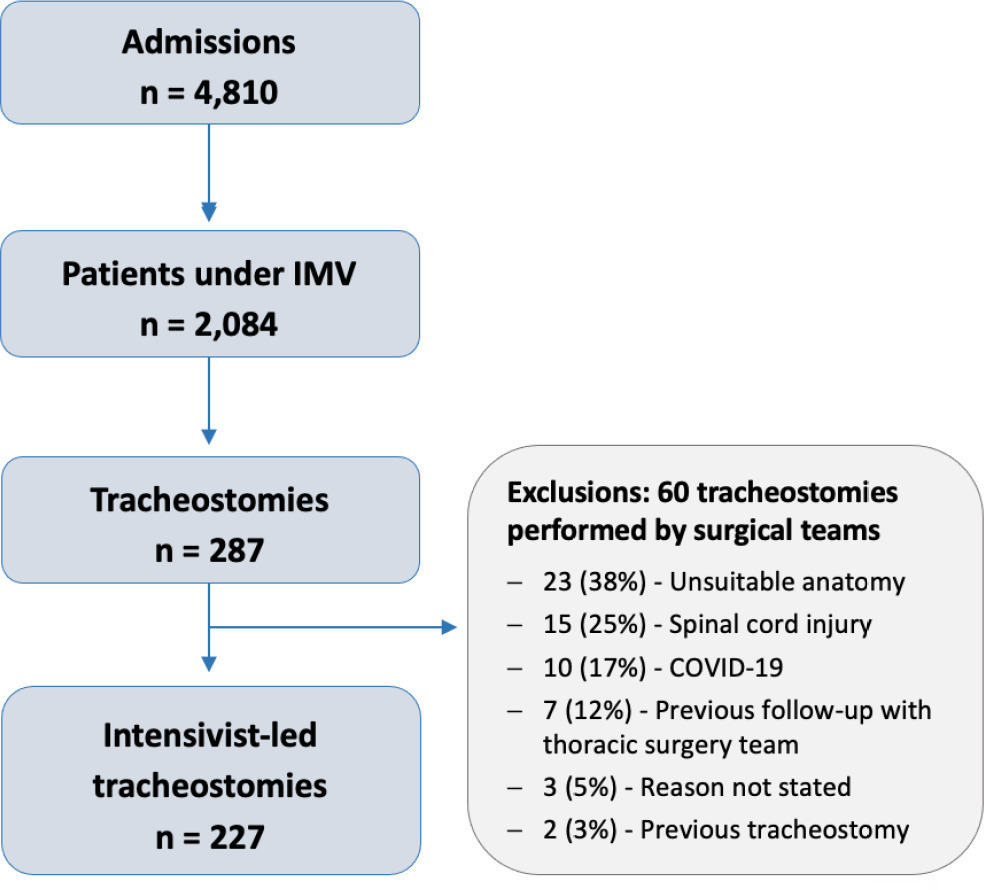
There were 4,810 intensive care unit admissions during the study period; 2,084 patients received mechanical ventilation, and 287 underwent tracheostomy, 227 of which were performed at bedside by the intensive care team. The main reason for intensive care unit admission was trauma, and for perform a tracheostomy it was a neurological impairment or an inability to protect the airways. The median time from intubation to tracheostomy was 14 days. Intensive care residents performed 76% of the procedures. At least one complication occurred in 29.5% of the procedures, the most common being hemodynamic instability and extubation during the procedure, with only 3 serious complications. The intensive care unit mortality was 29.1%, and the hospital mortality was 43.6%.
Intensivist-led ultrasound-guided percutaneous tracheostomy is feasible out of a clinical trial context with outcomes and complications comparable to those in the literature. Intensivists can acquire this competence during their training but should be aware of potential complications to enhance procedural safety.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):113-121
DOI 10.5935/0103-507X.20190018
To describe (1) the energy transfer from the ventilator to the lungs, (2) the match between venous-venous extracorporeal membrane oxygenation (ECMO) oxygen transfer and patient oxygen consumption (VO2), (3) carbon dioxide removal with ECMO, and (4) the potential effect of systemic venous oxygenation on pulmonary artery pressure.
Mathematical modeling approach with hypothetical scenarios using computer simulation.
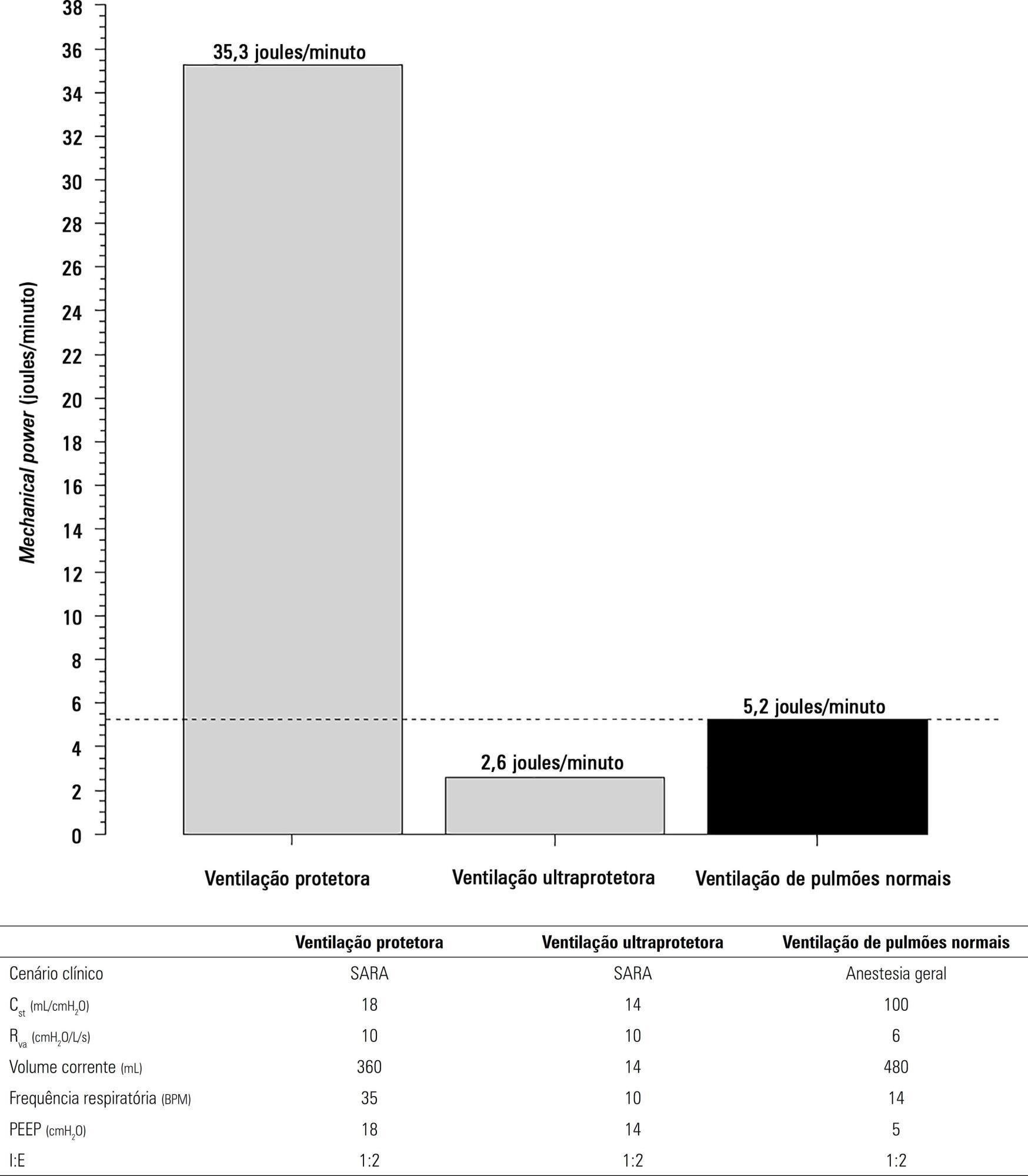
The transition from protective ventilation to ultraprotective ventilation in a patient with severe acute respiratory distress syndrome and a static respiratory compliance of 20mL/cm H2O reduced the energy transfer from the ventilator to the lungs from 35.3 to 2.6 joules/minute. A hypothetical patient, hyperdynamic and slightly anemic with VO2 = 200mL/minute, can reach an arterial oxygen saturation of 80%, while maintaining the match between the oxygen transfer by ECMO and the VO2 of the patient. Carbon dioxide is easily removed, and normal PaCO2 is easily reached. Venous blood oxygenation through the ECMO circuit may drive the PO2 stimulus of pulmonary hypoxic vasoconstriction to normal values.
Ultraprotective ventilation largely reduces the energy transfer from the ventilator to the lungs. Severe hypoxemia on venous-venous-ECMO support may occur despite the matching between the oxygen transfer by ECMO and the VO2 of the patient. The normal range of PaCO2 is easy to reach. Venous-venous-ECMO support potentially relieves hypoxic pulmonary vasoconstriction.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):86-97
DOI 10.5935/0103-507X.20180015
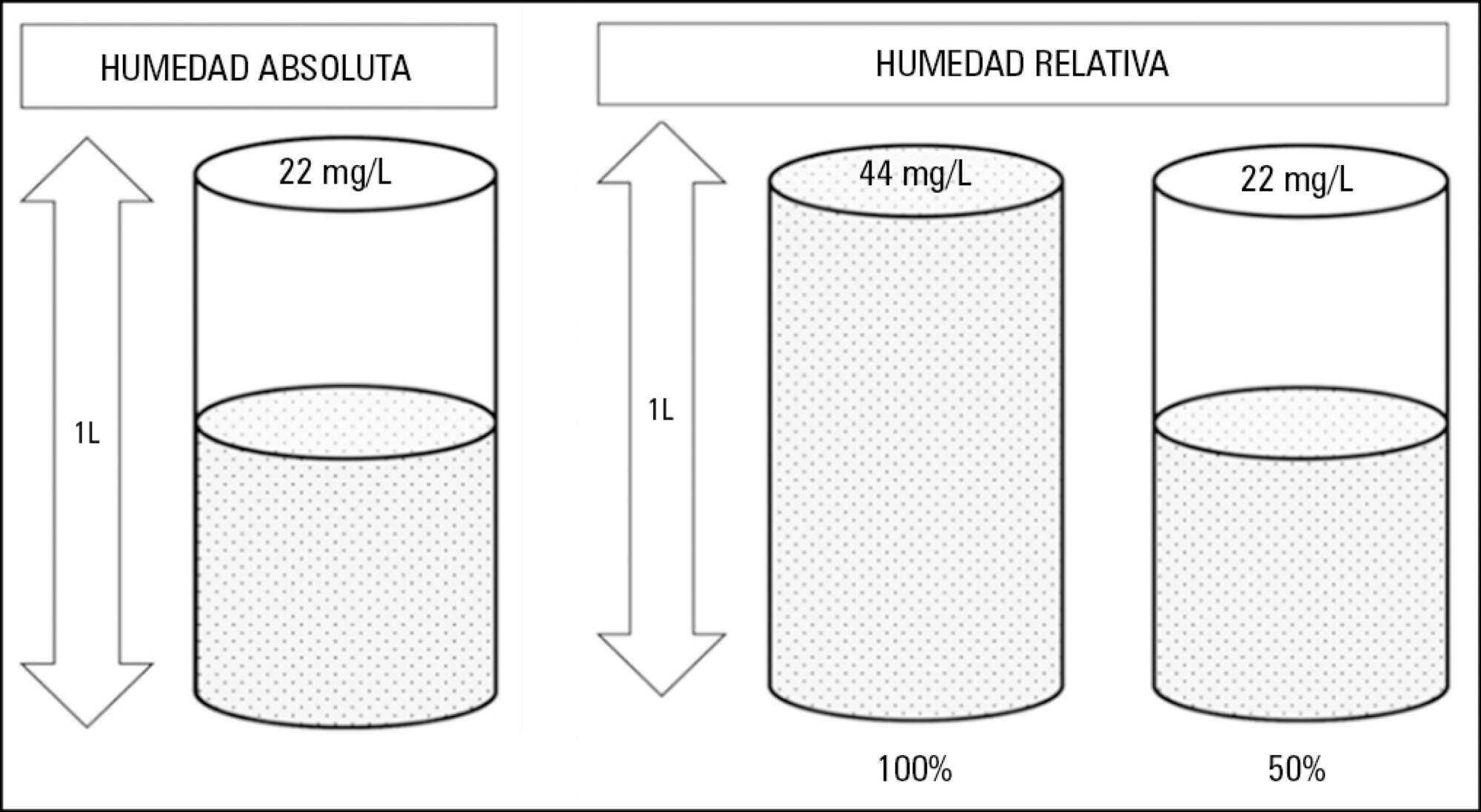
Instrumentation of the airways in critical patients (endotracheal tube or tracheostomy cannula) prevents them from performing their function of humidify and heating the inhaled gas. In addition, the administration of cold and dry medical gases and the high flows that patients experience during invasive and non-invasive mechanical ventilation generate an even worse condition. For this reason, a device for gas conditioning is needed, even in short-term treatments, to avoid potential damage to the structure and function of the respiratory epithelium. In the field of intensive therapy, the use of heat and moisture exchangers is common for this purpose, as is the use of active humidification systems. Acquiring knowledge about technical specifications and the advantages and disadvantages of each device is needed for proper use since the conditioning of inspired gases is a key intervention in patients with artificial airway and has become routine care. Incorrect selection or inappropriate configuration of a device can have a negative impact on clinical outcomes. The members of the Capítulo de Kinesiología Intensivista of the Sociedad Argentina de Terapia Intensiva conducted a narrative review aiming to show the available evidence regarding conditioning of inhaled gas in patients with artificial airways, going into detail on concepts related to the working principles of each one.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):452-462
DOI 10.5935/0103-507X.20160066
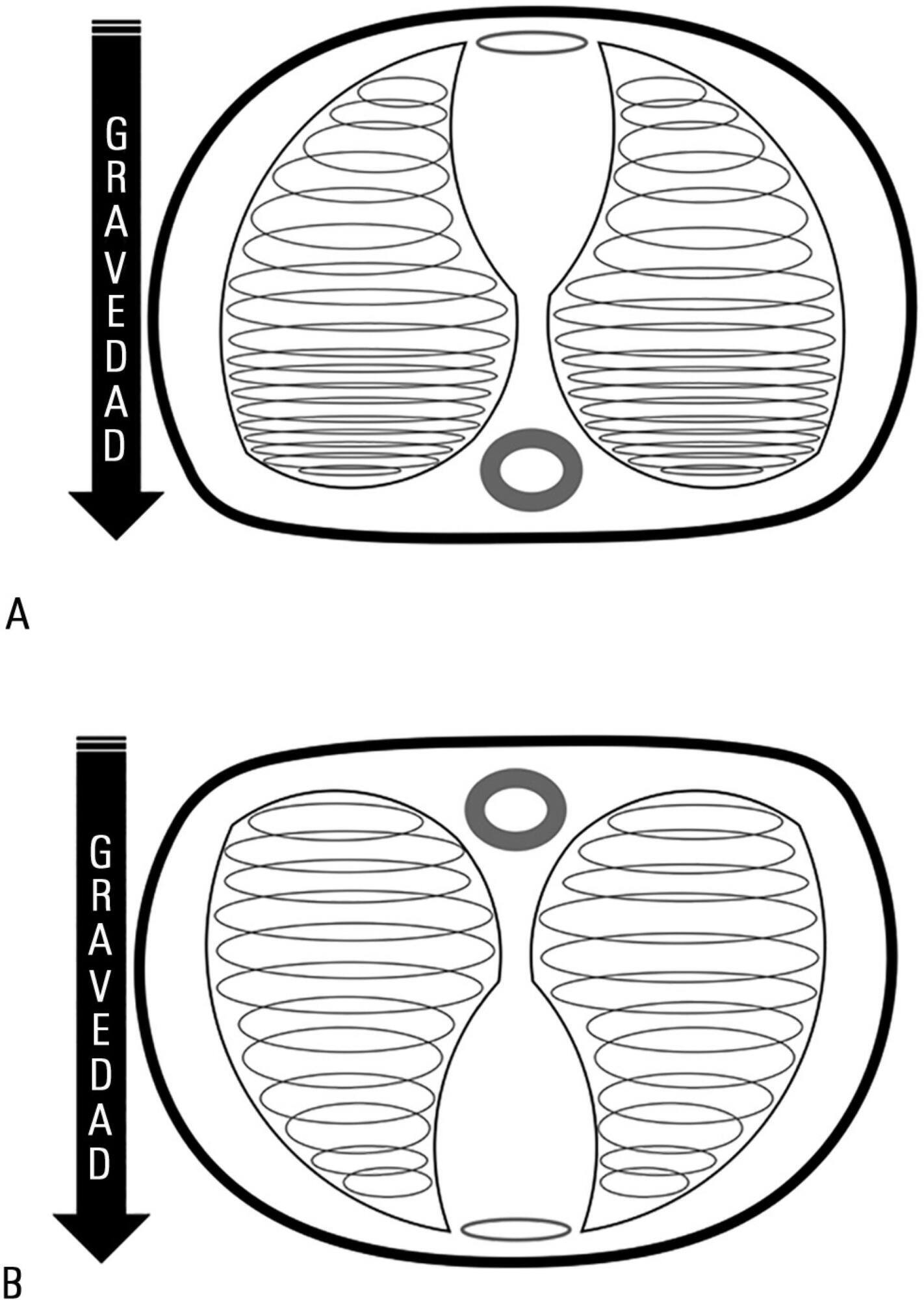
Acute respiratory distress syndrome occupies a great deal of attention in intensive care units. Despite ample knowledge of the physiopathology of this syndrome, the focus in intensive care units consists mostly of life-supporting treatment and avoidance of the side effects of invasive treatments. Although great advances in mechanical ventilation have occurred in the past 20 years, with a significant impact on mortality, the incidence continues to be high. Patients with acute respiratory distress syndrome, especially the most severe cases, often present with refractory hypoxemia due to shunt, which can require additional treatments beyond mechanical ventilation, among which is mechanical ventilation in the prone position. This method, first recommended to improve oxygenation in 1974, can be easily implemented in any intensive care unit with trained personnel.
Prone position has extremely robust bibliographic support. Various randomized clinical studies have demonstrated the effect of prone decubitus on the oxygenation of patients with acute respiratory distress syndrome measured in terms of the PaO2/FiO2 ratio, including its effects on increasing patient survival.
The members of the Respiratory Therapists Committee of the Sociedad Argentina de Terapia Intensiva performed a narrative review with the objective of discovering the available evidence related to the implementation of prone position, changes produced in the respiratory system due to the application of this maneuver, and its impact on mortality. Finally, guidelines are suggested for decision-making.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):56-61
DOI 10.1590/S0103-507X2011000100010
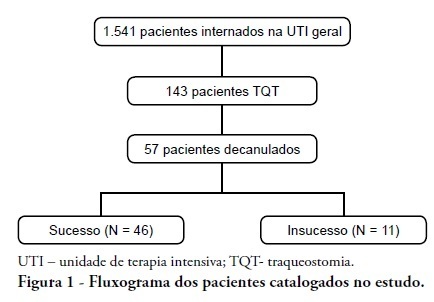
INTRODUCTION: Tracheostomy is probably the most common surgical procedure in critically ill patients and is generally performed to facilitate mechanical ventilation weaning. Evidence-based guidelines have confirmed the benefits of tracheostomy weaning protocols and of the physiotherapists engagement in this process; however, no consensus decannulation criteria are currently available. Therefore, this study aimed to evaluate the influence of peripheral muscle strength and other indicators on decannulation success. METHODS: This was an observational retrospective study that analyzed the medical records of patients admitted to the medical and surgical intensive care unit of Hospital Agamenon Magalhães between March 2007 and August 2009. Respiratory and peripheral muscle strengths were evaluated in decannulated patients. RESULTS: Overall, 1,541 patients were evaluated, 143 of which had been tracheostomized, and only 57 of which had been decannulated. Forty-six patients had a satisfactory decannulation outcome, while 11 had decannulation failure, requiring the return to an artificial airway within 2 weeks. The calculated Medical Research Council peripheral muscle strength score was significantly lower for the failure group than for the successful decannulation group (28.33 ± 15.31 vs. 41.11 ± 11.52; P = 0.04). Scores above or equal 26 had 94.4% sensitivity and 50.0% specificity for the decannulation outcome, with an area under the ROC curve of 0.7593. In addition, white blood cell counts were higher in decannulation failure group patients (14,070 ± 3,073 vs. 10,520 ± 3,402 cells/μL; P = 0.00). CONCLUSION: This study has shown that peripheral muscle strength and blood leucocyte counts evaluated on the day of decannulation may influence the tracheostomy decannulation success rate.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):264-269
DOI 10.1590/S0103-507X2010000300008
OBJECTIVES: In mechanically ventilated patients, humidifier devices are used to heat and moisturize the inspired gas. Heating and humidifying inspired gas may prevent complications associated with the respiratory mucosa dryness such as mucus plugging and endotracheal tube occlusion. Two devices have been commonly used to this, either heated humidifier or the heat moisture exchange filter. This study aimed to compare the effects of the heated humidifier and a model of heat moisture exchange filter on respiratory mechanics in mechanically ventilated neurological patients. METHODS: This was a randomized crossover trial, involving 31 neurological patients under mechanical ventilation randomly assigned to the humidification devices. Expired tidal volume, peak inspiratory flow, peak expiratory flow, static compliance, dynamic compliance and respiratory system resistance were evaluated. Statistical analysis used the Kolmogorov-Smirnov test and Student's t test for paired samples, in which P values < 0.05 were considered significant. RESULTS: The heat moisture exchanger filter decreased expired tidal volume, peak inspiratory flow, peak expiratory flow (p < 0.001) and dynamic compliance (p = 0.002), and increased respiratory system resistance (p < 0.001). CONCLUSION: In the studied population, the use of a heat moisture exchange filter model leaded to several changes on respiratory mechanics parameters.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):292-298
DOI 10.1590/S0103-507X2009000300009
BACKGROUND AND OBJECTIVES: An inspired oxygen fraction (FiO2) of 40% is often used for weaning patients, but lower FiO2 values are also recommended, if arterial oxygen pressure (PaO2)/ FiO2 >150-200 mmHg. This study aimed to compare respiratory variables and vital data values recorded during use of sufficient FiO2 (ideal) to maintain peripheral oxygen saturation at 92% with values recorded during use of FiO2 established at 40% (baseline) in weaning patients. METHODS: Prospective cross-over study. Respiratory variables (respiratory frequency, tidal volume, occlusion pressure, inspiratory time/total time ratio) and vital data (blood pressure and heart rate) were collected sequentially at 30 and 60 minutes with baseline FiO2, followed by ideal FiO2. These were compared to a generalized linear model for repeated measurements. Comparisons between baseline and ideal FiO2 values, and arterial blood gases were evaluated by the Student's t or Wilcoxon tests. RESULTS: In 30 adult patients the median of ideal FiO2 was 25% (IQ25%-75% 23-28). This was significantly lower than baseline FiO2 (40%) (p< 0.001). No significant difference was found in the PaO2/ FiO2 ratio between baseline FiO2 (269±53) and ideal FiO2 (268±47). Tidal volume was significantly lower during use of ideal FiO2 (p=0.003) and blood pressure was significantly higher during use of baseline FiO2 (p=0.041), but there was no clinical significance. The remaining variables were not affected by reduction in FiO2. The ideal FiO2 did not influence remaining variables. CONCLUSIONS: These results suggest that FiO2 levels sufficient to ensure a SpO2>92% did not alter breathing patterns or trigger clinical changes in weaning patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) ICU (25) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)