Abstract
Rev Bras Ter Intensiva. 2020;32(3):433-438
DOI 10.5935/0103-507X.20200073
To describe the use of neuromuscular blockade as well as other practices among Brazilian physicians in adult intensive care units.
An online national survey was designed and administered to Brazilian intensivists. Questions were selected using the Delphi method and assessed physicians’ demographic data, intensive care unit characteristics, practices regarding airway management, use of neuromuscular blockade and sedation during endotracheal intubation in the intensive care unit. As a secondary outcome, we applied a multivariate analysis to evaluate factors associated with the use of neuromuscular blockade.
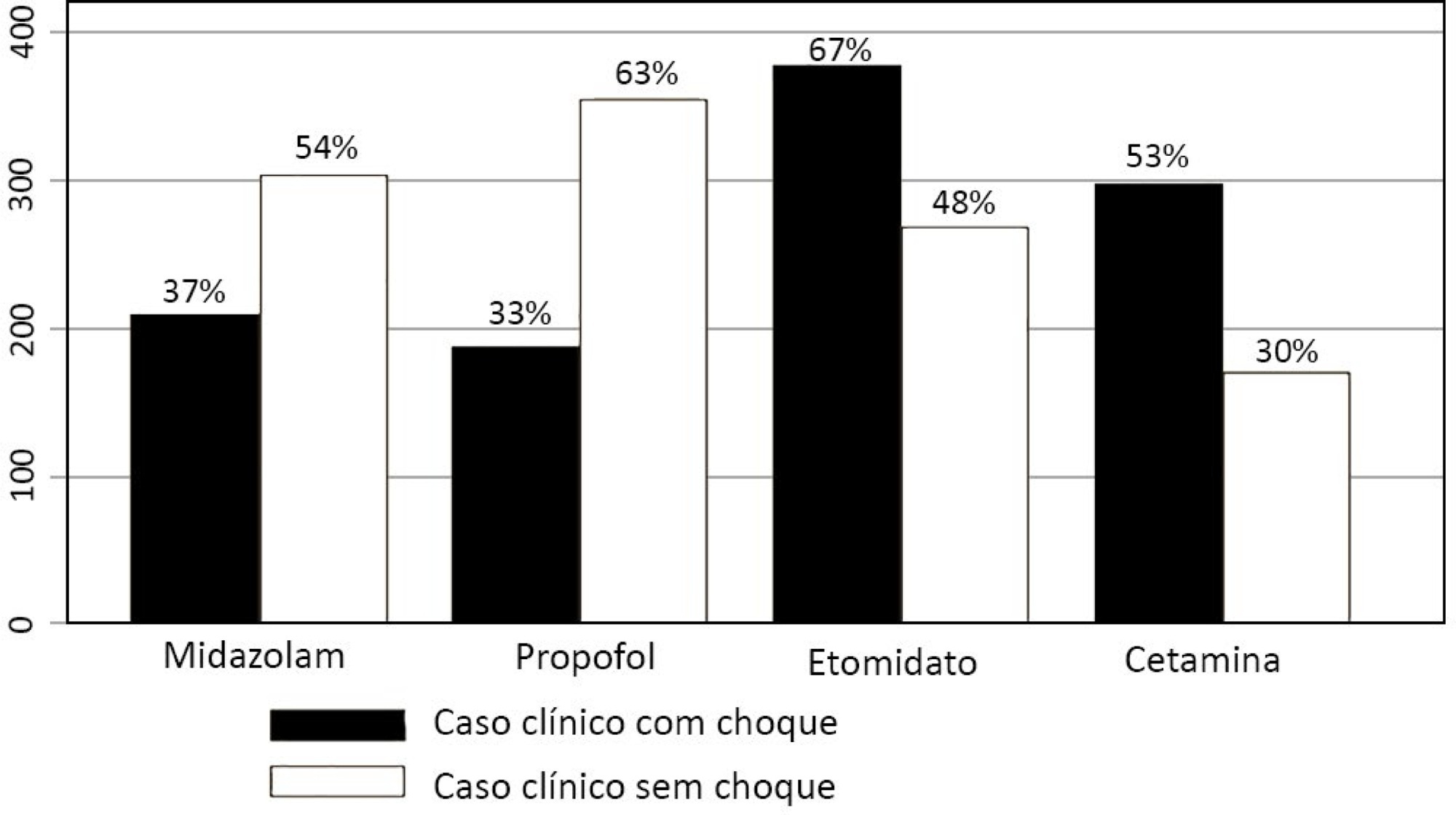
Five hundred sixty-five intensivists from all Brazilian regions responded to the questionnaire. The majority of respondents were male (65%), with a mean age of 38 ( 8.4 years, and 58.5% had a board certification in critical care. Only 40.7% of the intensivists reported the use of neuromuscular blockade during all or in more than 75% of endotracheal intubations. In the multivariate analysis, the number of intubations performed monthly and physician specialization in anesthesiology were directly associated with frequent use of neuromuscular blockade. Etomidate and ketamine were more commonly used in the clinical situation of hypotension and shock, while propofol and midazolam were more commonly prescribed in the situation of clinical stability.
The reported use of neuromuscular blockade was low among intensivists, and sedative drugs were chosen in accordance with patient hemodynamic stability. These results may help the design of future studies regarding airway management in Brazil.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):86-97
DOI 10.5935/0103-507X.20180015
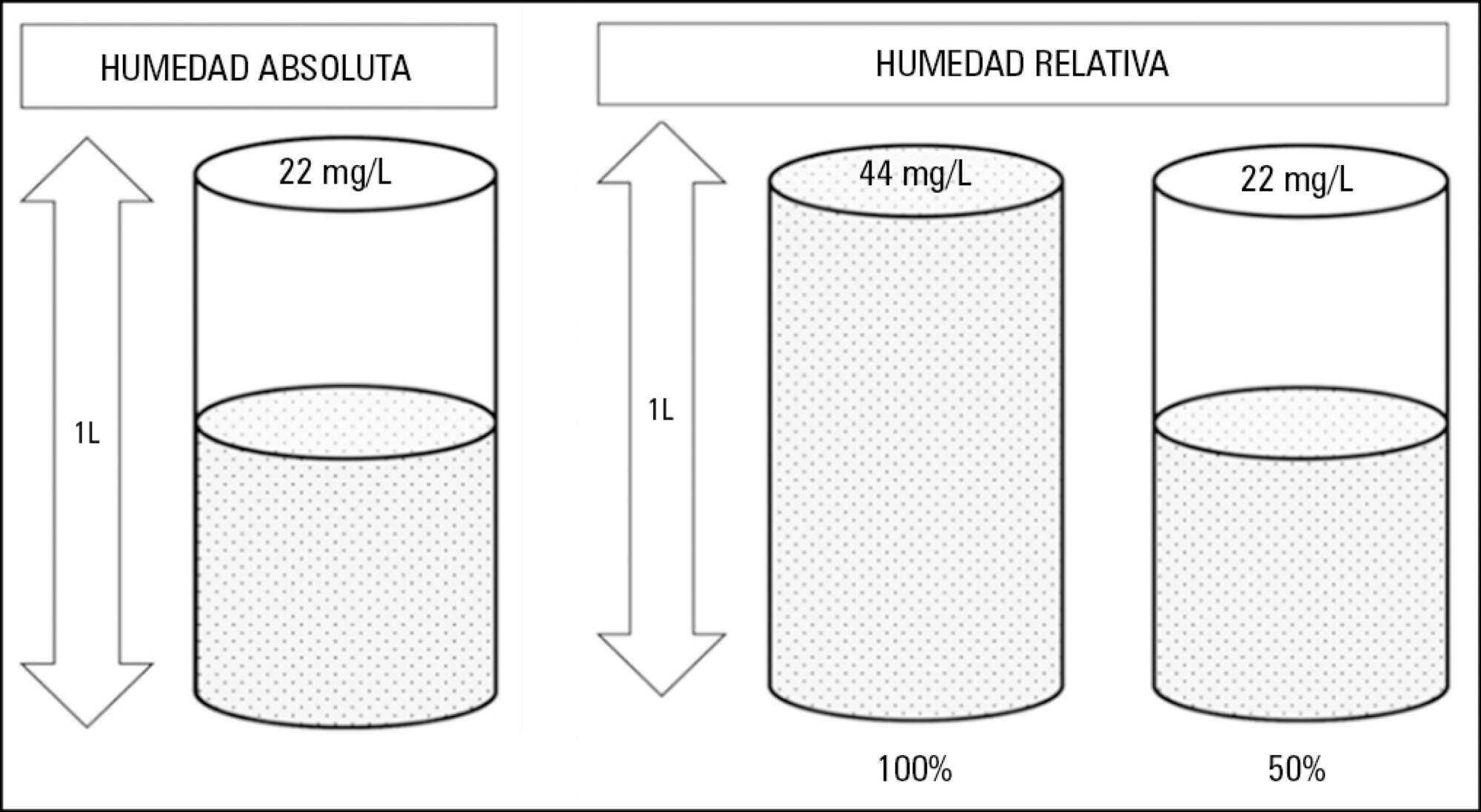
Instrumentation of the airways in critical patients (endotracheal tube or tracheostomy cannula) prevents them from performing their function of humidify and heating the inhaled gas. In addition, the administration of cold and dry medical gases and the high flows that patients experience during invasive and non-invasive mechanical ventilation generate an even worse condition. For this reason, a device for gas conditioning is needed, even in short-term treatments, to avoid potential damage to the structure and function of the respiratory epithelium. In the field of intensive therapy, the use of heat and moisture exchangers is common for this purpose, as is the use of active humidification systems. Acquiring knowledge about technical specifications and the advantages and disadvantages of each device is needed for proper use since the conditioning of inspired gases is a key intervention in patients with artificial airway and has become routine care. Incorrect selection or inappropriate configuration of a device can have a negative impact on clinical outcomes. The members of the Capítulo de Kinesiología Intensivista of the Sociedad Argentina de Terapia Intensiva conducted a narrative review aiming to show the available evidence regarding conditioning of inhaled gas in patients with artificial airways, going into detail on concepts related to the working principles of each one.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):14-22
DOI 10.5935/0103-507X.20170004
To evaluate the effects of bag-valve breathing maneuvers combined with standard manual chest compression techniques on safety, hemodynamics and oxygenation in stable septic shock patients.
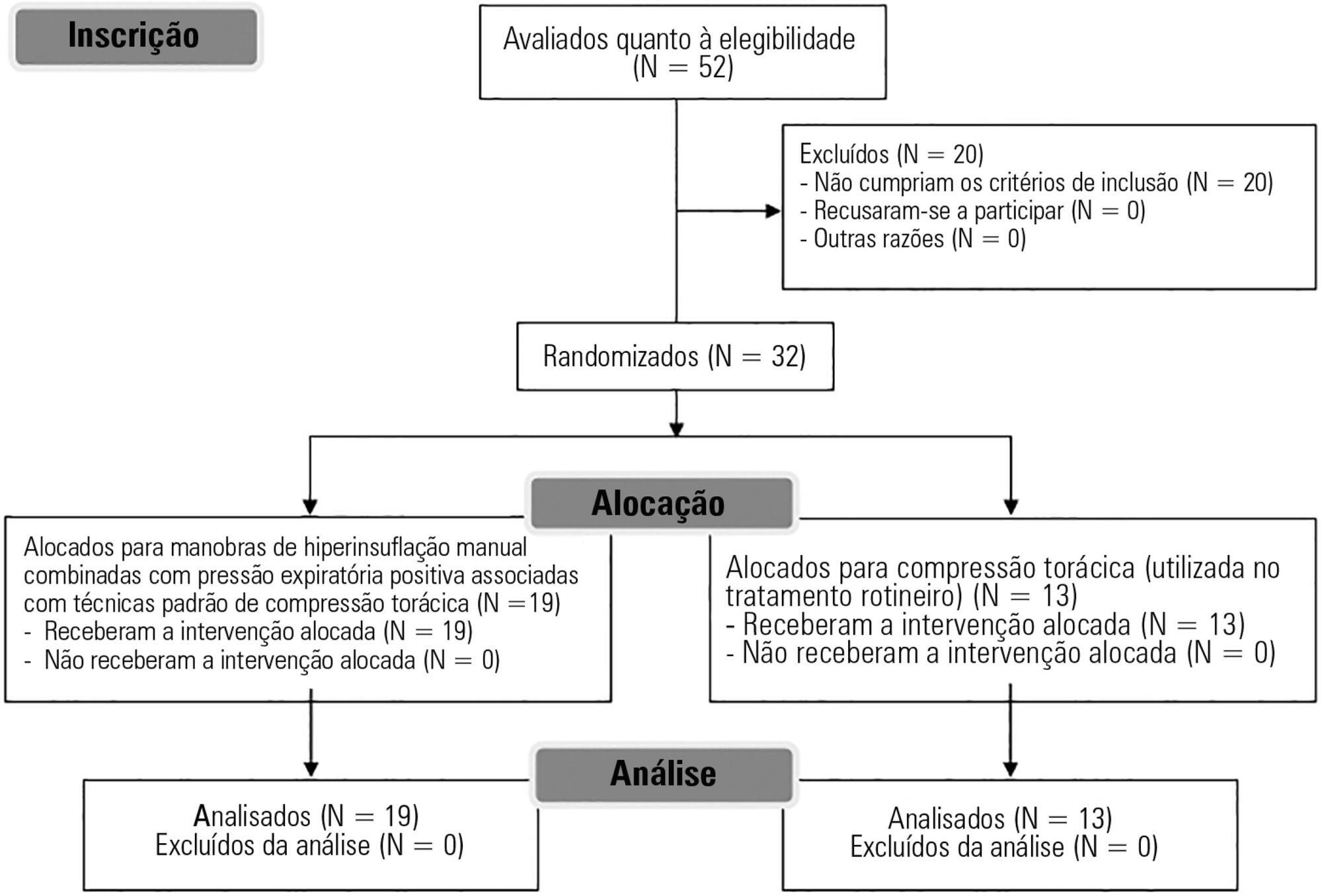
A parallel, assessor-blinded, randomized trial of two groups. A computer-generated list of random numbers was prepared by an independent researcher to allocate treatments.
The Intensive Care Unit at Hospital São Lucas, Pontifícia Universidade Católica do Rio Grande do Sul.
Fifty-two subjects were assessed for eligibility, and 32 were included. All included subjects (n = 32) received the allocated intervention (n = 19 for the Experimental Group and n = 13 for the Control Group).
Twenty minutes of bag-valve breathing maneuvers combined with manual chest compression techniques (Experimental Group) or chest compression, as routinely used at our intensive care unit (Control Group). Follow-up was performed immediately after and at 30 minutes after the intervention.
Mean artery pressure.
All included subjects completed the trial (N = 32). We found no relevant effects on mean artery pressure (p = 0.17), heart rate (p = 0.50) or mean pulmonary artery pressure (p = 0.89) after adjusting for subject age and weight. Both groups were identical regarding oxygen consumption after the data adjustment (p = 0.84). Peripheral oxygen saturation tended to increase over time in both groups (p = 0.05), and there was no significant association between cardiac output and venous oxygen saturation (p = 0.813). No clinical deterioration was observed.
A single session of bag-valve breathing maneuvers combined with manual chest compression is hemodynamically safe for stable septic-shocked subjects over the short-term.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):367-372
DOI 10.5935/0103-507X.20140056
To test the effectiveness of using a cuff pressure relief valve technique to maintain cuff pressure levels within the normal in vitro range (Phase 1) in patients admitted to the intensive care unit (Phase 2) and to test the reproducibility of the technique using different syringes.
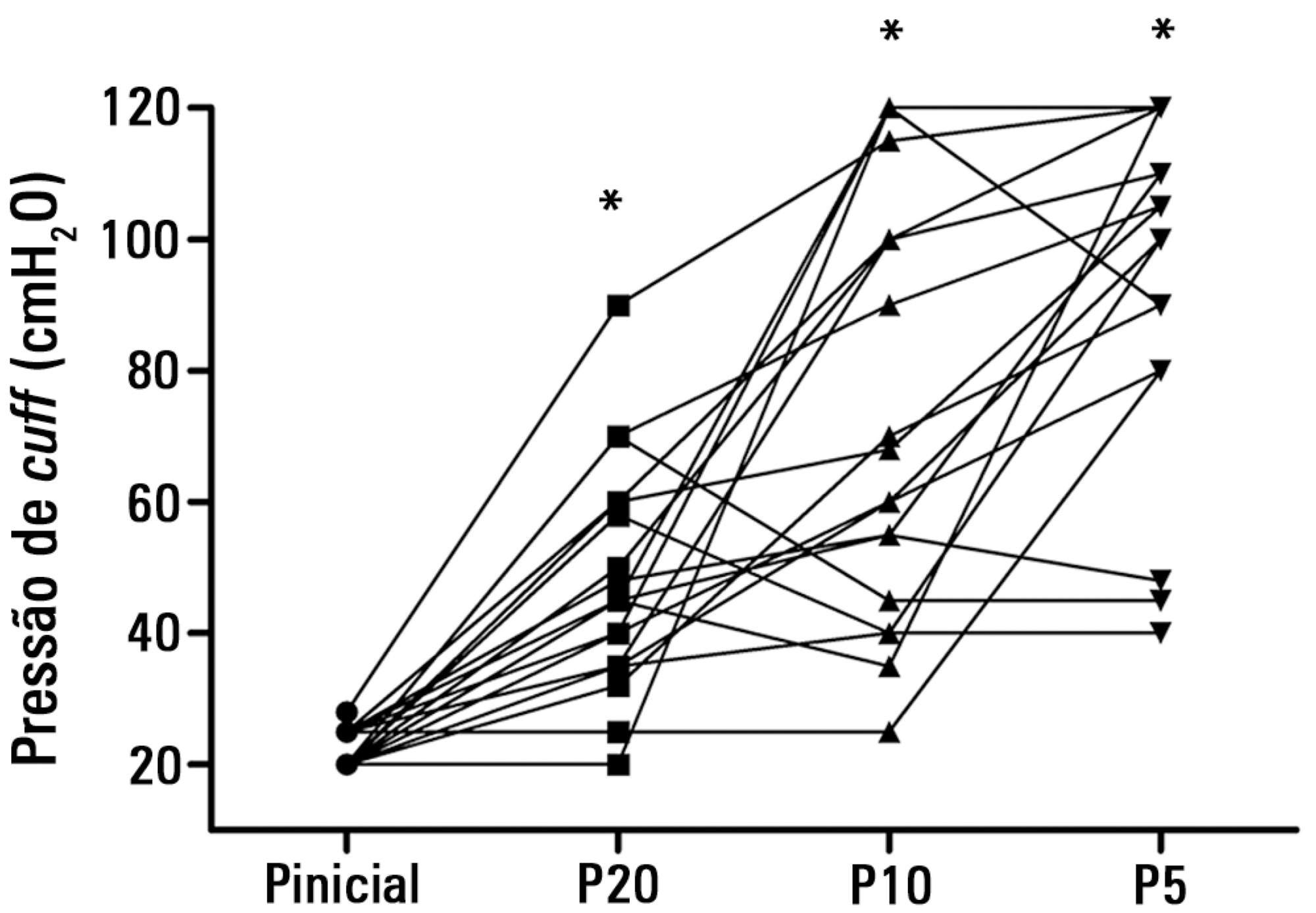
In Phase 1, a tracheal tube was inserted into a trachea model. Ten- and 20mL syringes were used to inflate the cuff through the tracheal tube. The cuff was slowly and steadily inflated until the syringe plunger would move in the opposite direction of the application. After the plunger stopped, the cuff pressures were recorded. In Phase 2, the same maneuvers for inflating the cuff were performed on 20 patients using 5, 10, and 20mL syringes and were compared with manometer measurements. The intraclass correlation coefficient and Bland-Altman analysis were employed to determine the reproducibility and agreement between syringes. Data were expressed as medians (interquartile range).
There was no reproducibility between syringes with an intraclass correlation coefficient ranging between -0.33 and 0.8 (p>0.05). The pressures generated with the syringes were higher than the pressures generated using a standard manometer: the 5mL syringe pressure was 105cmH2O (82.5-120cmH2O), the 10mL syringe pressure was 69cmH2O (47.5-111.3cmH2O), and the 20mL syringe pressure was 45cmH2O (35-59.5cmH2O). The Bland-Altman analysis confirmed the large bias and variability between the syringes used, compared with the manometer.
The use of syringes is not an effective technique for determining the cuff pressure in patients admitted to the intensive care unit.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)