Abstract
Rev Bras Ter Intensiva. 2019;31(4):447-455
DOI 10.5935/0103-507X.20190085
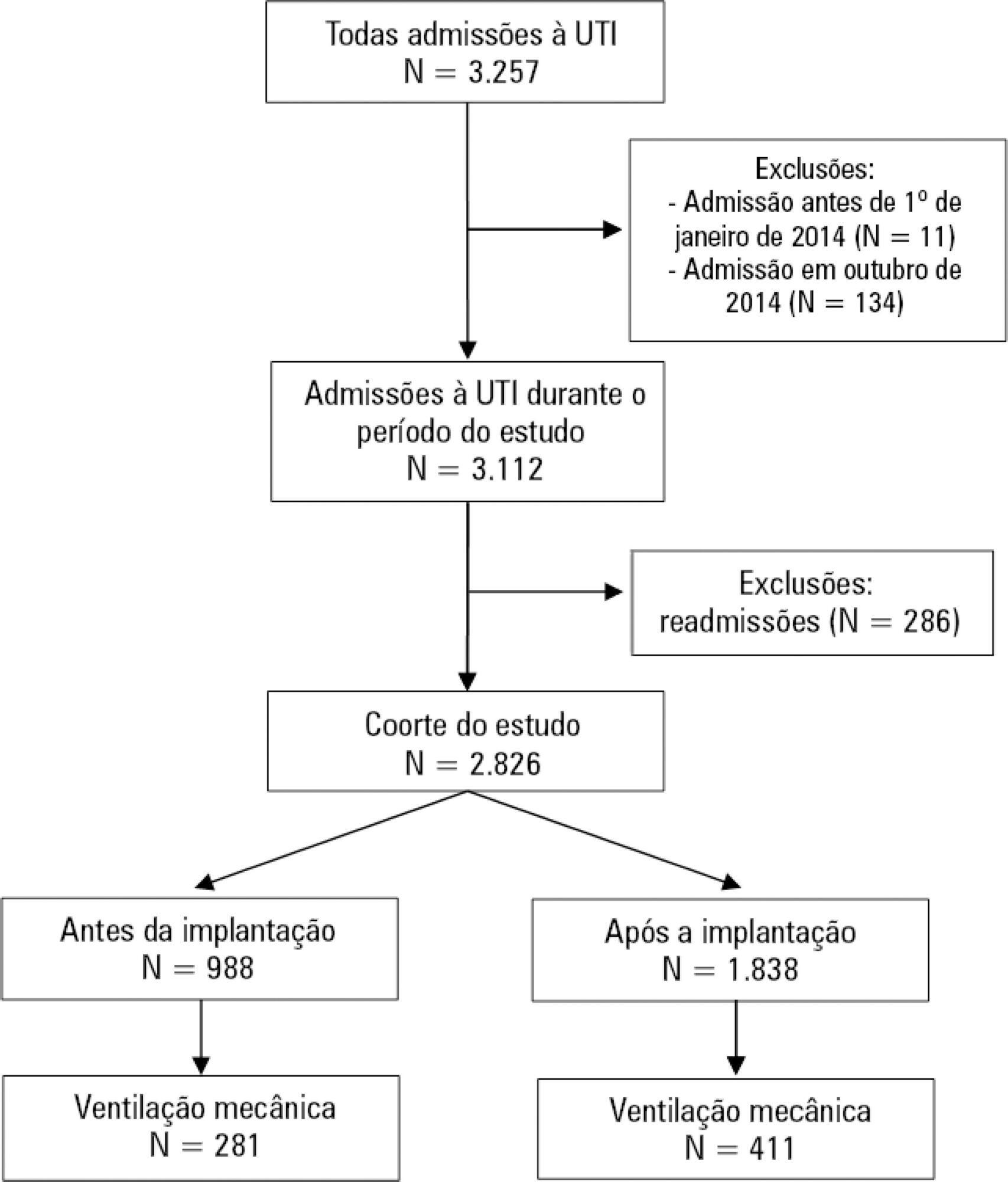
To evaluate the impact of an opioid-sparing pain management protocol on overall opioid consumption and clinical outcomes.
This was a single-center, quasi-experimental, retrospective, before and after cohort study. We used an interrupted time series to analyze changes in the levels and trends of the utilization of different analgesics. We used bivariate comparisons in the before and after cohorts as well as logistic regression and quantile regression for adjusted estimates.
We included 988 patients in the preintervention period and 1,838 in the postintervention period. Fentanyl consumption was slightly increasing before the intervention (β = 16; 95%CI 7 - 25; p = 0.002) but substantially decreased in level with the intervention (β = - 128; 95%CI -195 - -62; p = 0.001) and then progressively decreased (β = - 24; 95%CI -35 - -13; p < 0.001). There was an increasing trend in the utilization of dipyrone. The mechanical ventilation duration was significantly lower (median difference: - 1 day; 95%CI -1 - 0; p < 0.001), especially for patients who were mechanically ventilated for a longer time (50th percentile difference: -0.78; 95%CI -1.51 - -0.05; p = 0.036; 75th percentile difference: -2.23; 95%CI -3.47 - -0.98; p < 0.001).
A pain management protocol could reduce the intensive care unit consumption of fentanyl. This strategy was associated with a shorter mechanical ventilation duration.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):456-463
DOI 10.5935/0103-507X.20190078
To evaluate the level of activity that Nintendo WiiTM can elicit in intensive care unit patients and its associated safety and patient satisfaction.
Experimental, single-center study performed at a tertiary care hospital. Patients ≥ 18 years old who were admitted to the intensive care unit, participated in videogames as part of their physical therapy sessions and did not have mobility restrictions were included. Th exclusion criteria were the inability to comprehend instructions and the inability to follow simple commands. We included n = 60 patients and performed 100 sessions. We used the Nintendo WiiTM gaming system in the sessions. An accelerometer measured the level of physical activity of patients while they played videogames. We evaluated the level of activity, the modified Borg scale scores, the adverse events and the responses to a questionnaire on satisfaction with the activity.
One hundred physical therapy sessions were analyzed. When the patients played the videogame, they reached a light level of activity for 59% of the session duration and a moderate level of activity for 38% of the session duration. No adverse events occurred. A total of 86% of the patients reported that they would like to play the videogame in their future physical therapy sessions.
Virtual rehabilitation elicited light to moderate levels of activity in intensive care unit patients. This therapy is a safe tool and is likely to be chosen by the patient during physical therapy.

Abstract
Rev Bras Ter Intensiva. 2019;31(4):464-473
DOI 10.5935/0103-507X.20190072
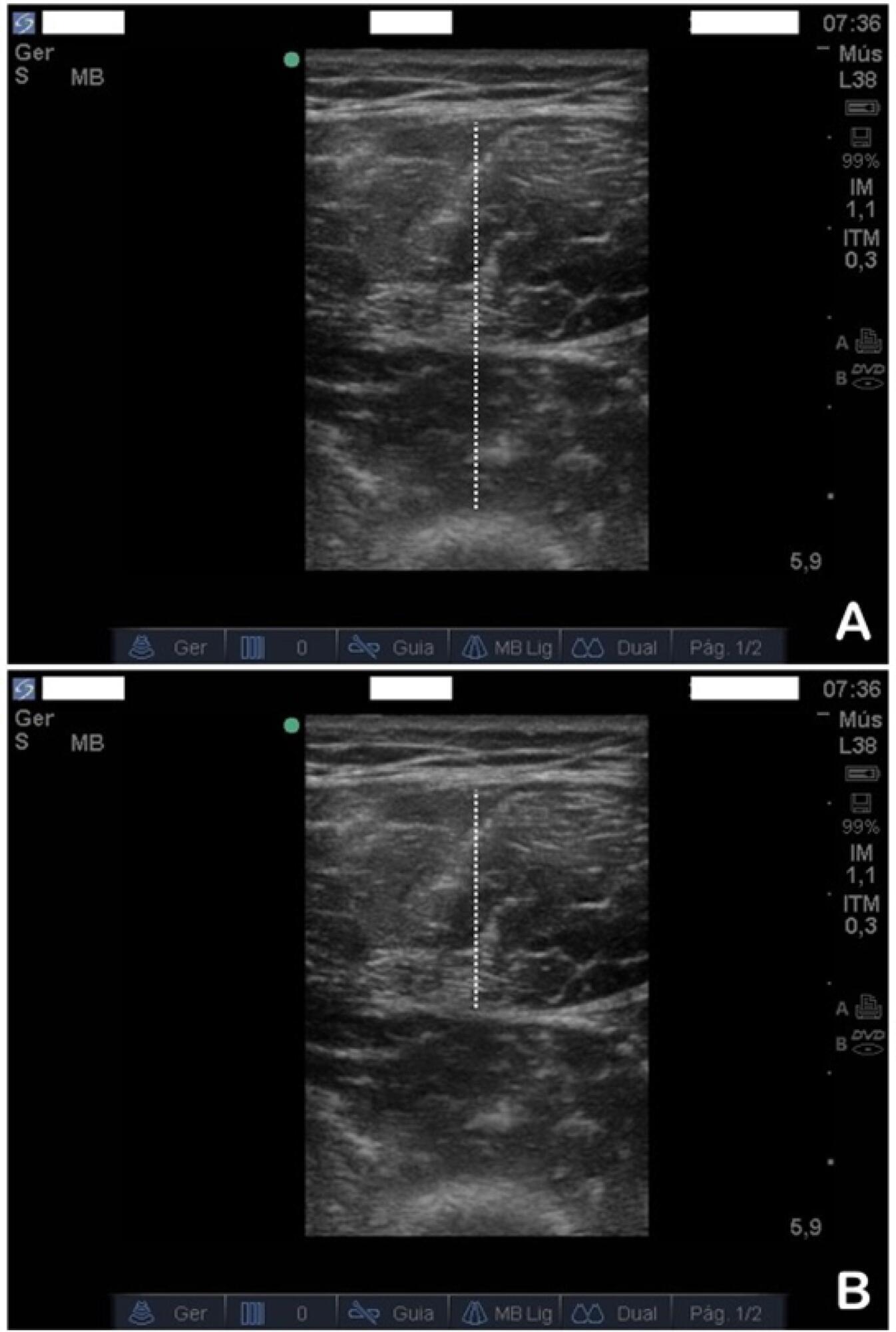
To evaluate the safety and feasibility of the ultrasound assessment of quadriceps in the emergency setting. To assess the intra- and interrater reliability for the acquisition and analysis of ultrasound images of muscle thickness and echogenicity in critically ill trauma patients between health professionals with different levels of expertise.
Diagnostic accuracy study. Two examiners (expert and novice) acquired ultrasound images from ten patients; an experienced, blinded analyst quantified the images. In a separate group of ten patients, two analysts (expert and novice) quantified quadriceps muscle thickness and echogenicity (square or trace method) from images acquired by one examiner.
Excellent reliability was found for image acquisition and analysis (intraclass correlation coefficients > 0.987; p < 0.001). The standard error of the measurement values ranged from 0.01 - 0.06cm for muscle thickness and from 0.75 - 2.04 arbitrary units for muscle echogenicity. The coefficients of variation were < 6% for thickness and echogenicity. The echogenicity values were higher when using the square technique than when using the tracing technique (p = 0.003).
Ultrasound is safe, feasible, and reliable for muscle assessment in critically ill trauma patients, regardless of the assessor's level of expertise.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):474-482
DOI 10.5935/0103-507X.20190073
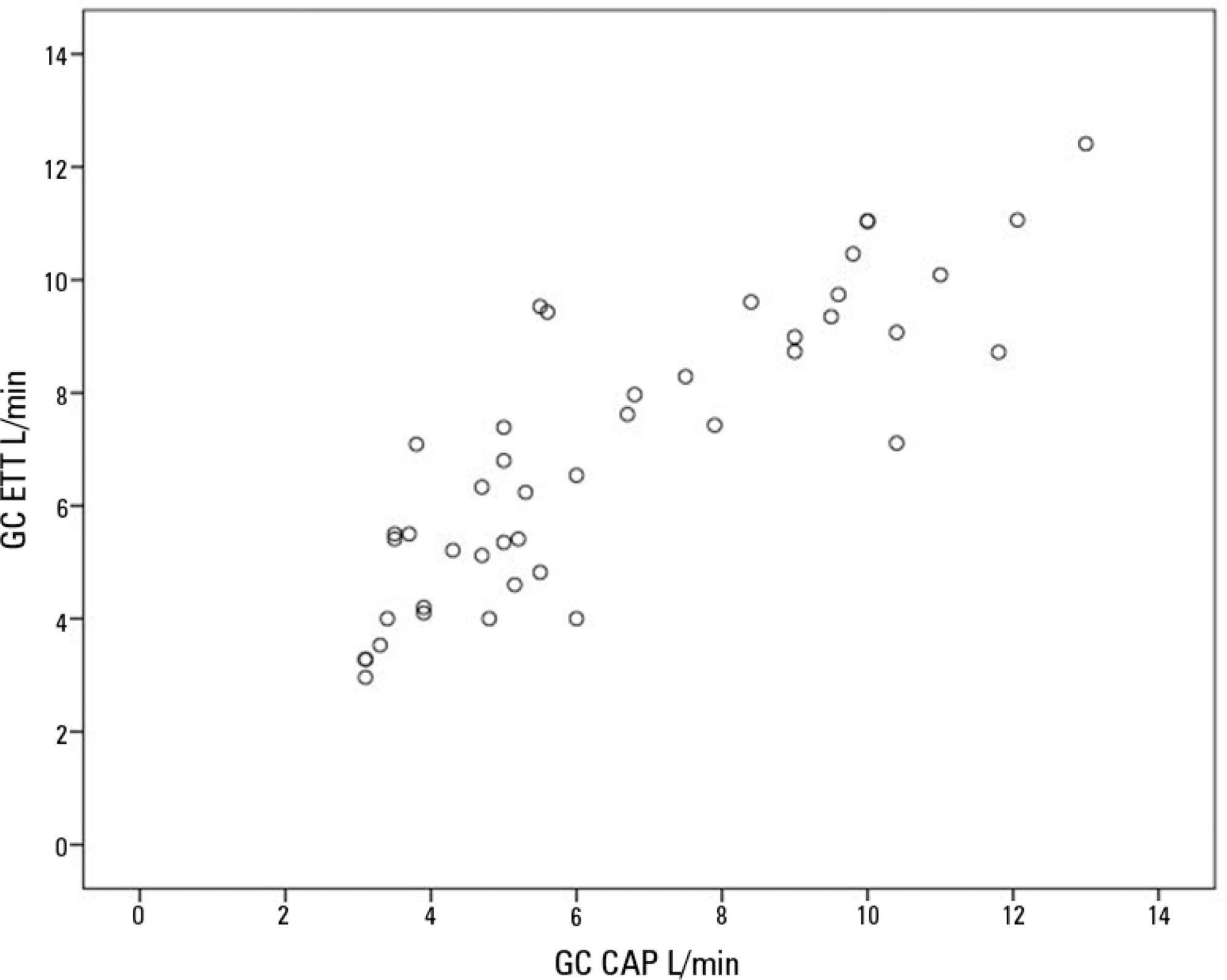
To compare cardiac output measurements by transthoracic echocardiography and a pulmonary artery catheter in mechanically ventilated patients with high positive end-expiratory pressure. To evaluate the effect of tricuspid regurgitation.
Sixteen mechanically ventilated patients were studied. Cardiac output was measured by pulmonary artery catheterization and transthoracic echocardiography. Measurements were performed at different levels of positive end-expiratory pressure (10cmH2O, 15cmH2O, and 20cmH2O). The effect of tricuspid regurgitation on cardiac output measurement was evaluated. The intraclass correlation coefficient was studied; the mean error and limits of agreement were studied with the Bland-Altman plot. The error rate was calculated.
Forty-four pairs of cardiac output measurements were obtained. An intraclass correlation coefficient of 0.908 was found (p < 0.001). The mean error was 0.44L/min for cardiac output values between 5 and 13L/min. The limits of agreement were 3.25L/min and -2.37L/min. With tricuspid insufficiency, the intraclass correlation coefficient was 0.791, and without tricuspid insufficiency, 0.935. Tricuspid insufficiency increased the error rate from 32% to 52%.
In patients with high positive end-expiratory pressure, cardiac output measurement by transthoracic echocardiography is comparable to that with a pulmonary artery catheter. Tricuspid regurgitation influences the intraclass correlation coefficient. In patients with high positive end-expiratory pressure, the use of transthoracic echocardiography to measure cardiac output is comparable to invasive measures.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):483-489
DOI 10.5935/0103-507X.20190071
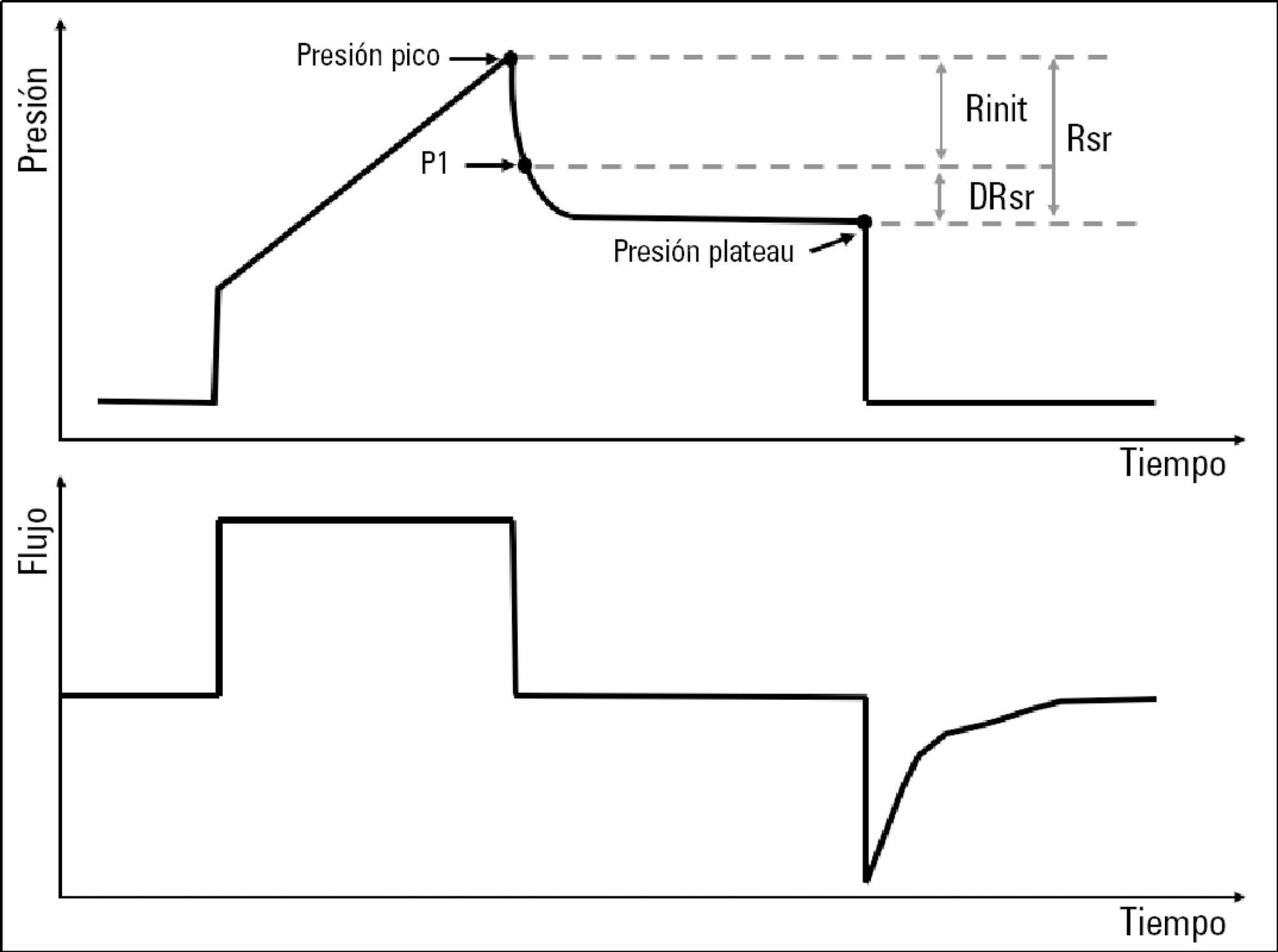
To describe the behavior of inspiratory resistance components when positive end-expiratory pressure (PEEP) increases in patients with acute respiratory distress syndrome under a protective ventilation strategy.
In volume-controlled mode, at 6mL/kg and constant flow, end-inspiratory occlusions were performed at 0, 5 10, 15 and 20cmH2O PEEP. Peak, initial and plateau pressure values were assessed, calculating the maximum, minimum and differential resistances. The results were compared by repeated measures analysis of variance (ANOVA) with post hoc Bonferroni correction, considering p < 0.05 significant.
The highest maximum resistance was observed at the lowest PEEP levels. The values for 10 and 15cmH2O PEEP significantly differed from those for 5 and 0cmH2O PEEP, whereas that for 20cmH2O PEEP only significantly differed from that for 0cmH2O PEEP (p < 0.05). The minimum resistance behaved similarly to the maximum resistance; the values for PEEP levels from 10cmH2O to 20cmH2O significantly differed from those for 0 and 5cmH2O PEEP (p < 0.05). Differential resistance showed the opposite variation to the maximum and minimum resistances. The only PEEP level that showed significant differences from 0 and 5cmH2O PEEP was 20cmH2O PEEP. Significant differences were also found between 15 and 5cmH2O PEEP (p < 0.05).
During protective ventilation in patients with acute respiratory distress syndrome, the maximum resistance of the respiratory system decreases with PEEP, reflecting the minimum resistance response, whereas differential resistance increases with PEEP.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):490-496
DOI 10.5935/0103-507X.20190086
To evaluate the concordance between the modified NUTRIC and NUTRIC with C-reactive protein instruments in identifying nutritional risk patients and predicting mortality in critically ill patients. The risk of death in patient groups was also investigated according to nutritional risk and malnutrition detected by subjective global assessment.
A cohort study of patients admitted to an intensive care unit. Nutritional risk was assessed by modified NUTRIC and a version of NUTRIC with C-reactive protein. Subjective global assessment was applied to diagnose malnutrition. Kappa statistics were calculated, and an ROC curve was constructed considering modified NUTRIC as a reference. The predictive validity was assessed considering mortality in 28 days (whether in the intensive care unit or after discharge) as the outcome.
A total of 130 patients were studied (63.05 ± 16.46 years, 53.8% males). According to NUTRIC with C-reactive protein, 34.4% were classified as having a high score, while 28.5% of patients had this classification with modified NUTRIC. According to SGA 48.1% of patients were malnourished. There was excellent agreement between modified NUTRIC and NUTRIC with C-reactive protein (Kappa = 0.88, p < 0.001). The area under the ROC curve was equal to 0.942 (0.881 - 1.000) for NUTRIC with C-reactive protein. The risk of death within 28 days was increased in patients with high modified NUTRIC (HR = 1.827; 95%CI 1.029 - 3.244; p = 0.040) and NUTRIC with C-reactive protein (HR = 2.685; 95%CI 1.423 - 5.064; p = 0.002) scores. A high risk of death was observed in patients with high nutritional risk and malnutrition, independent of the version of the NUTRIC score applied.
An excellent agreement between modified NUTRIC and NUTRIC with C-reactive protein was observed. In addition, combining NUTRIC and subjective global assessment may increase the accuracy of predicting mortality in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):497-503
DOI 10.5935/0103-507X.20190087
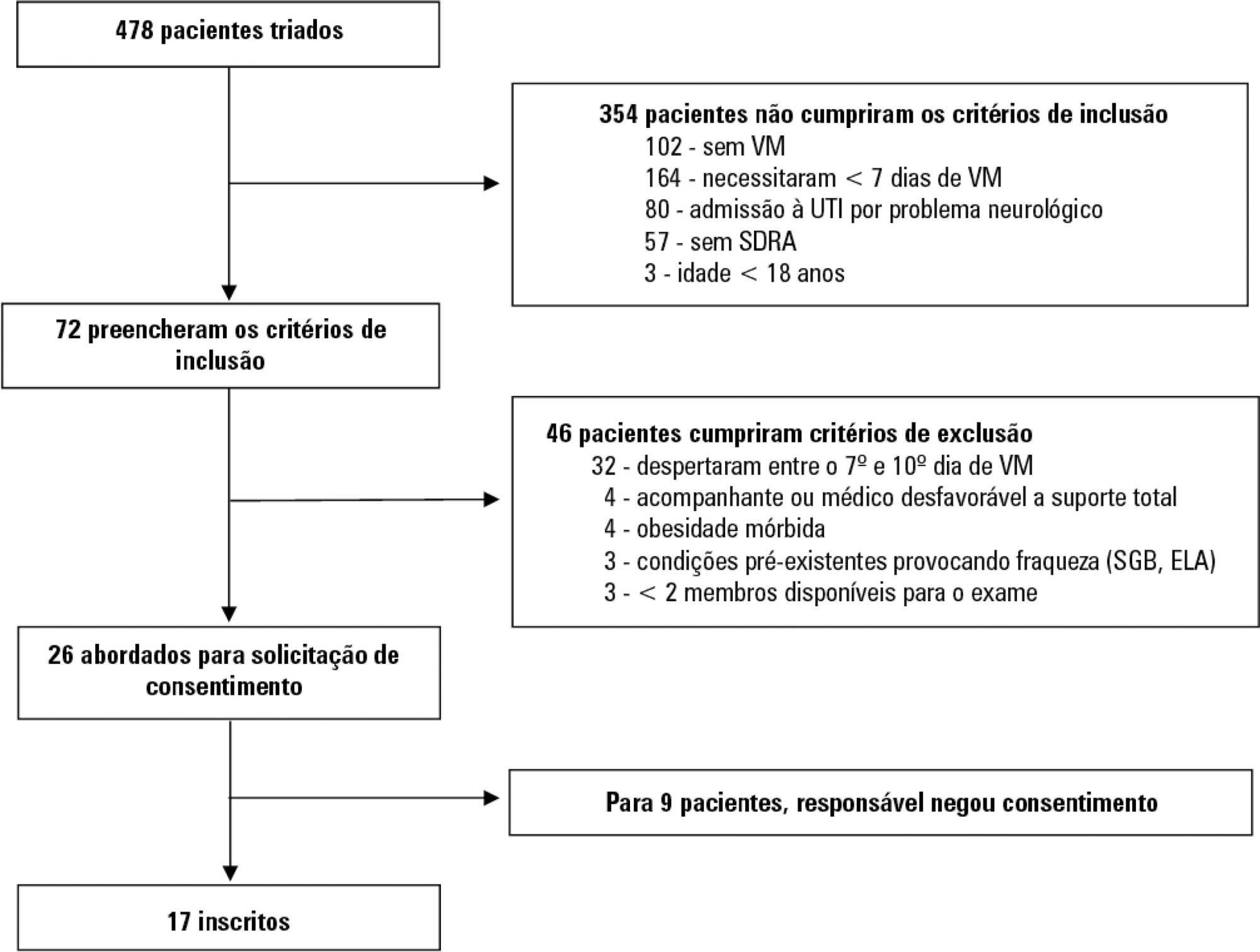
To evaluate whether electromyographical findings could predict intensive care unit mortality among mechanically ventilated septic patients under profound sedation.
A prospective cohort study that consecutively enrolled moderate-severe acute respiratory distress syndrome (partial pressure of oxygen/fraction of inspired oxygen < 200) patients who were ≥ 18 years of age, dependent on mechanical ventilation for ≥ 7 days, and under profound sedation (Richmond Agitation Sedation Scale ≤ -4) was conducted. Electromyographic studies of the limbs were performed in all patients between the 7th and the 10th day of mechanical ventilation. Sensory nerve action potentials were recorded from the median and sural nerves. The compound muscle action potentials were recorded from the median (abductor pollicis brevis muscle) and common peroneal (extensor digitorum brevis muscle) nerves.
Seventeen patients were enrolled during the seven months of the study. Nine patients (53%) had electromyographic signs of critical illness myopathy or neuropathy. The risk of death during the intensive care unit stay was increased in patients with electromyographical signs of critical illness myopathy or neuropathy in comparison to those without these diagnostics (77.7% versus 12.5%, log-rank p = 0.02).
Electromyographical signs of critical illness myopathy or neuropathy between the 7th and the 10th day of mechanical ventilation may be associated with intensive care unit mortality among moderate-severe acute respiratory distress syndrome patients under profound sedation, in whom clinical strength assessment is not possible.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) ICU (25) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)