Abstract
Rev Bras Ter Intensiva. 2019;31(4):504-510
DOI 10.5935/0103-507X.20190067
To evaluate the risk factors for protein-caloric inadequacy in critically ill patients.
Prospective cohort study of patients hospitalized in an adult intensive care unit between February and November 2017. Patients were followed for 7 days. The conditional probability of inadequacy was calculated using the Kaplan-Meier method and the 95% log-rank test. To assess the risk of inadequacy, crude and adjusted hazard ratios (HR) were calculated using Cox regression with a 95% confidence interval.
Of the 130 patients, 63.8% were male, 73.8% were <60 years of age, and 49.2% were diagnosed with trauma. The mean APACHE II score was 24 points, and 70.0% of the patients had a protein-caloric adequacy >80%. In the univariate analysis, the significant variables for inadequacy were use of vasoactive drugs, interruptions of diet and failure to initiate nutrition early. In the final model, patients who presented with vomiting/gastric residue (adjusted HR = 22.5; 95%CI 5.14 - 98.87) and fasting for extubation (adjusted HR = 14.75; 95%CI 3.59 - 60.63) and for examinations and interventions (adjusted HR = 12.46; 95%CI 4.52 - 34.36) had a higher risk of not achieving protein-caloric adequacy.
Achievement of nutritional goals > 80.0% occurred in 70.0% of patients. The risk factors for protein-caloric inadequacy were nutritional interruptions, especially due to vomiting/gastric residue and fasting for extubation, exams and surgical procedures.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):511-520
DOI 10.5935/0103-507X.20190088
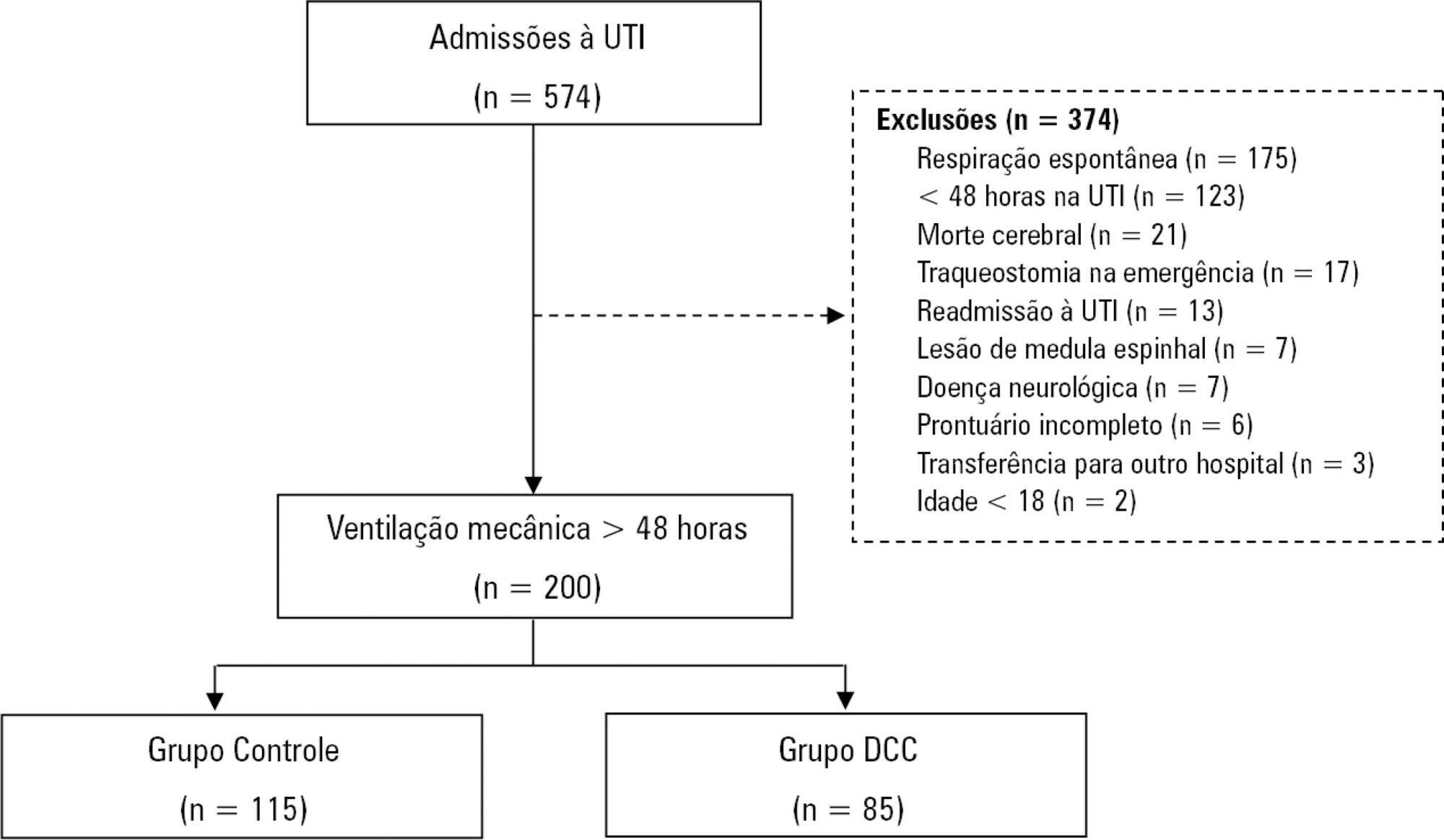
To characterize patients with chronic critical illness and identify predictors of development of chronic critical illness.
Prospective data was collected for 1 year in the intensive care unit of a general hospital in Southern Brazil. Three logistic regression models were constructed to identify factors associated with chronic critical illness.
Among the 574 subjects admitted to the intensive care unit, 200 were submitted to mechanical ventilation. Of these patients, 85 (43.5%) developed chronic critical illness, composing 14.8% of all the patients admitted to the intensive care unit. The regression model that evaluated the association of chronic critical illness with conditions present prior to intensive care unit admission identified chronic renal failure in patients undergoing hemodialysis (OR 3.57; p = 0.04) and a neurological diagnosis at hospital admission (OR 2.25; p = 0.008) as independent factors. In the model that evaluated the association of chronic critical illness with situations that occurred during intensive care unit stay, muscle weakness (OR 2.86; p = 0.01) and pressure ulcers (OR 9.54; p < 0.001) had the strongest associations. In the global multivariate analysis (that assessed previous factors and situations that occurred in the intensive care unit), hospital admission due to neurological diseases (OR 2.61; p = 0.03) and the development of pressure ulcers (OR 9.08; p < 0.001) had the strongest associations.
The incidence of chronic critical illness in this study was similar to that observed in other studies and had a strong association with the diagnosis of neurological diseases at hospital admission and chronic renal failure in patients undergoing hemodialysis, as well as complications developed during hospitalization, such as pressure ulcers and muscle weakness.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):521-528
DOI 10.5935/0103-507X.20190065
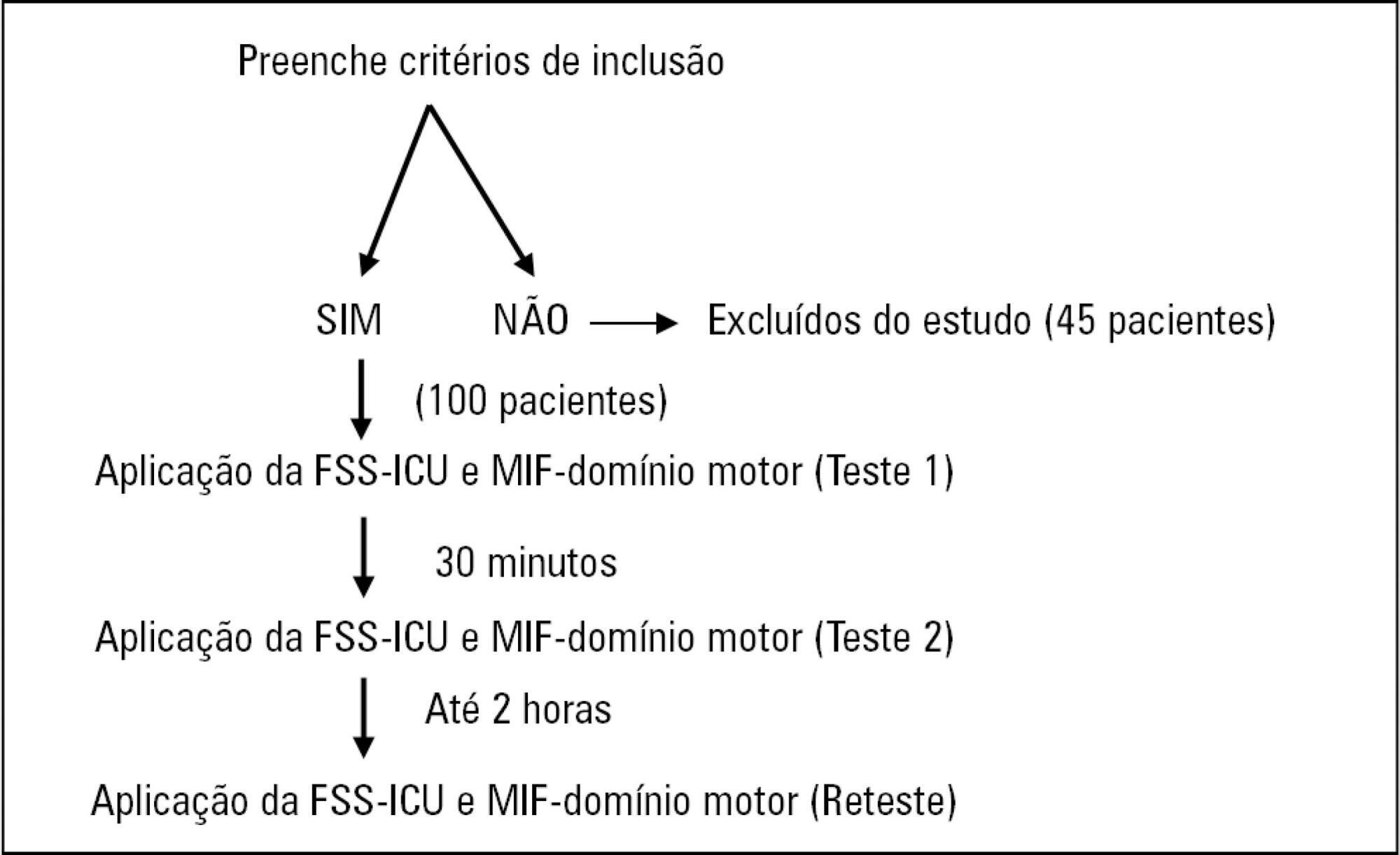
To compare the measurement properties (internal consistency, intra and interrater reliability, construct validity, and ceiling and floor effects) of the Functional Status Score for the ICU (FSS-ICU) and the Functional Independence Measure (FIM-motor domain).
In this study of measurement properties, the FSS-ICU and FIM were applied to 100 patients (72.1 ± 15.9 years; 53% male; Sequential Organ Failure Assessment = 11.0 ± 3.5 points, Simplified Acute Physiology Score 3 = 50.2 ± 16.8 points) in an intensive care unit at baseline and after 2 hours by physiotherapist 1 (test and retest) and 30 minutes after baseline by physiotherapist 2. The measurement properties evaluated were internal consistency (Cronbach's alpha), intra- and interrater reliability (intraclass correlation coefficient), agreement (standard error of measurement) and minimum detectable change at a 90% confidence level, ceiling and floor effects (frequency of maximum and minimum scores) and construct validity (Pearson's correlation).
The FSS-ICU and FIM presented adequate internal consistency (Cronbach's alpha, FSS-ICU = 0.95 and FIM = 0.86), intra-and interrater reliability for overall FSS-ICU and FIM score (ICC > 0.75), agreement (minimum detectable change at a 90% confidence level: FSS-ICU and FIM = 1.0 point; standard error of measurement: FSS-ICU = 2% and FIM = 1%) and construct validity (r = 0.94; p < 0.001). However, the FSS-ICU and FIM presented ceiling effects (maximum score for 16% of patients for the FSS-ICU and 18% for the FIM).
The FSS-ICU and FIM present adequate measurement properties to assess functionality in critically ill patients, although they present ceiling effects.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):529-535
DOI 10.5935/0103-507X.20190066
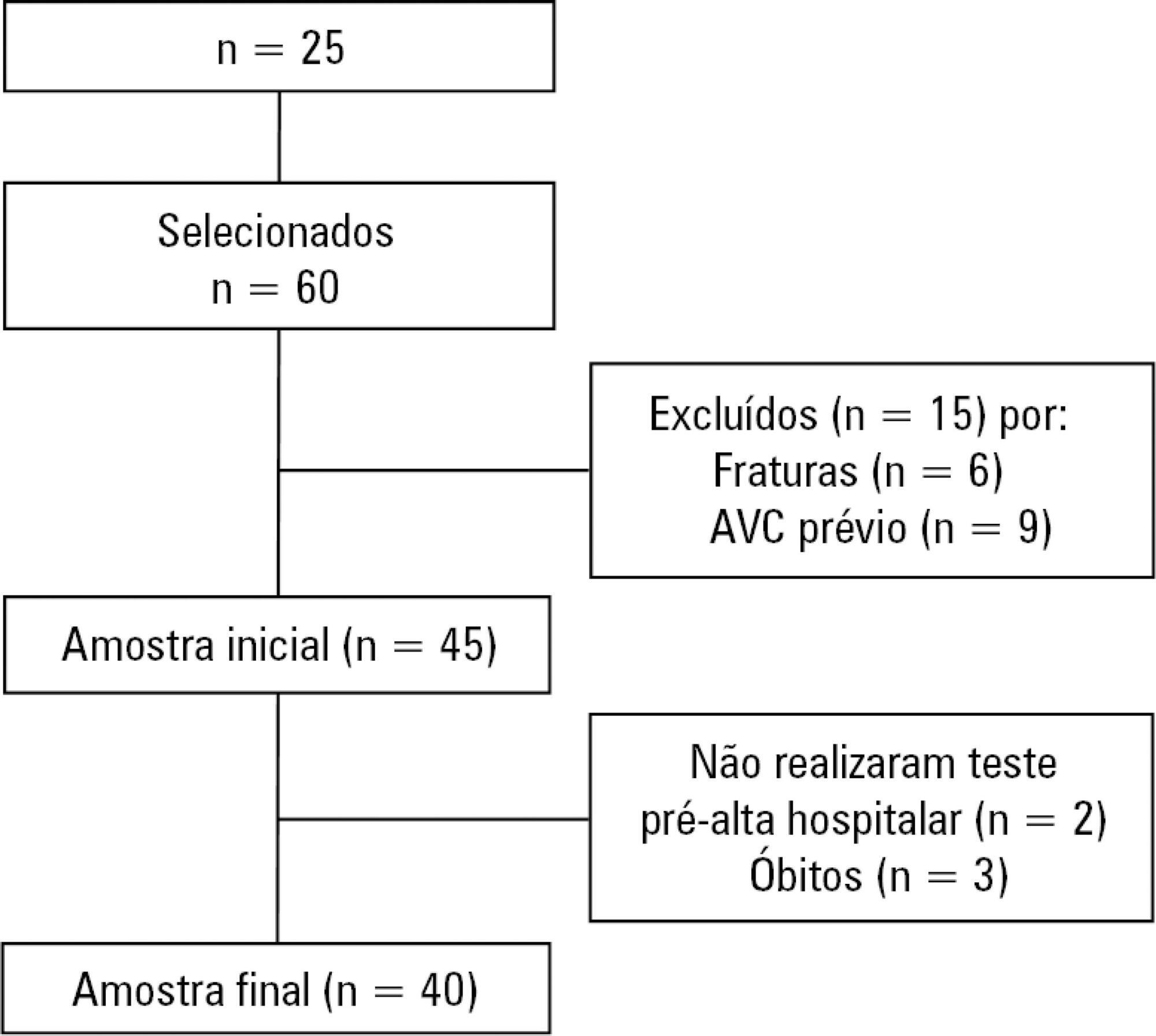
To measure and compare the functionality of patients after discharge from the intensive care unit and at the time of hospital discharge.
Quantitative study of a prospective cohort performed between August of 2016 and December of 2017 at a university hospital. A 10-meter walk test was performed at 2 timepoints: after discharge from the intensive care unit and prior to hospital discharge. The data were analyzed using Student's t-test and Pearson or Spearman correlation. Statistical Package for Social Science (SPSS) version 21.0 was used for the analysis, and p ≤ 0.05 was adopted as the level of significance.
Forty patients, with a mean age of 57.1 ± 12.2 years and with a predominance of males (60%), were evaluated. For the post-intensive care unit test, a mean speed of 0.48m/s was observed, and for the pre-hospital discharge test, there was an increase to 0.71m/s, evidencing functional evolution during the hospital stay (p < 0.001).
There was significant improvement in walking speed at the time of hospital discharge when compared to the walking speed at the time of intensive care unit discharge.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):333-339
DOI 10.5935/0103-507X.20190045
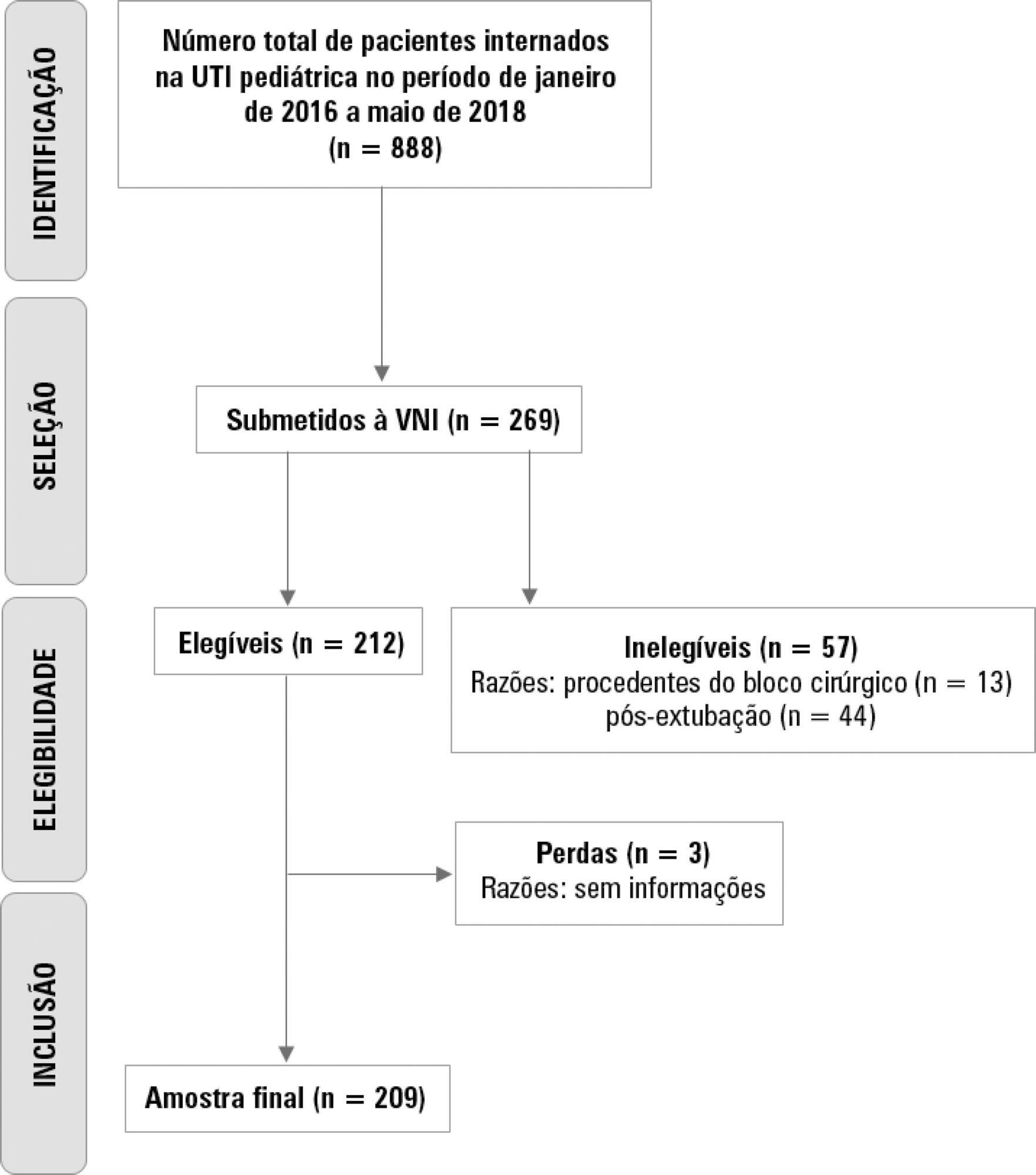
To describe the use of noninvasive ventilation to prevent tracheal intubation in children in a pediatric intensive care unit and to analyze the factors related to respiratory failure.
A retrospective cohort study was performed from January 2016 to May 2018. The study population included children aged 1 to 14 years who were subjected to noninvasive ventilation as the first therapeutic choice for acute respiratory failure. Biological, clinical and managerial data were analyzed by applying a model with the variables that obtained significance ≤ 0.20 in a bivariate analysis. Logistic regression was performed using the ENTER method. The level of significance was set at 5%.
The children had a mean age of 68.7 ± 42.3 months, 96.6% had respiratory disease as a primary diagnosis, and 15.8% had comorbidities. Of the 209 patients, noninvasive ventilation was the first option for ventilatory support in 86.6% of the patients, and the fraction of inspired oxygen was ≥ 0.40 in 47% of the cases. The lethality rate was 1.4%. The data for the use of noninvasive ventilation showed a high success rate of 95.3% (84.32 - 106). The Pediatric Risk of Mortality (PRISM) score and the length of stay in the intensive care unit were the significant clinical variables for the success or failure of noninvasive ventilation.
A high rate of effectiveness was found for the use of noninvasive ventilation for acute episodes of respiratory failure. A higher PRISM score on admission, comorbidities associated with respiratory symptoms and oxygen use ≥ 40% were independent factors related to noninvasive ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):340-346
DOI 10.5935/0103-507X.20190049
To identify the underlying factors that affect fluid resuscitation in septic patients.
The present study was a case-control study of 181 consecutive patients admitted to a Medical Intensive Care Unit between 2012 and 2016 with a diagnosis of sepsis. Demographic, clinical, radiological and laboratory data were analyzed.
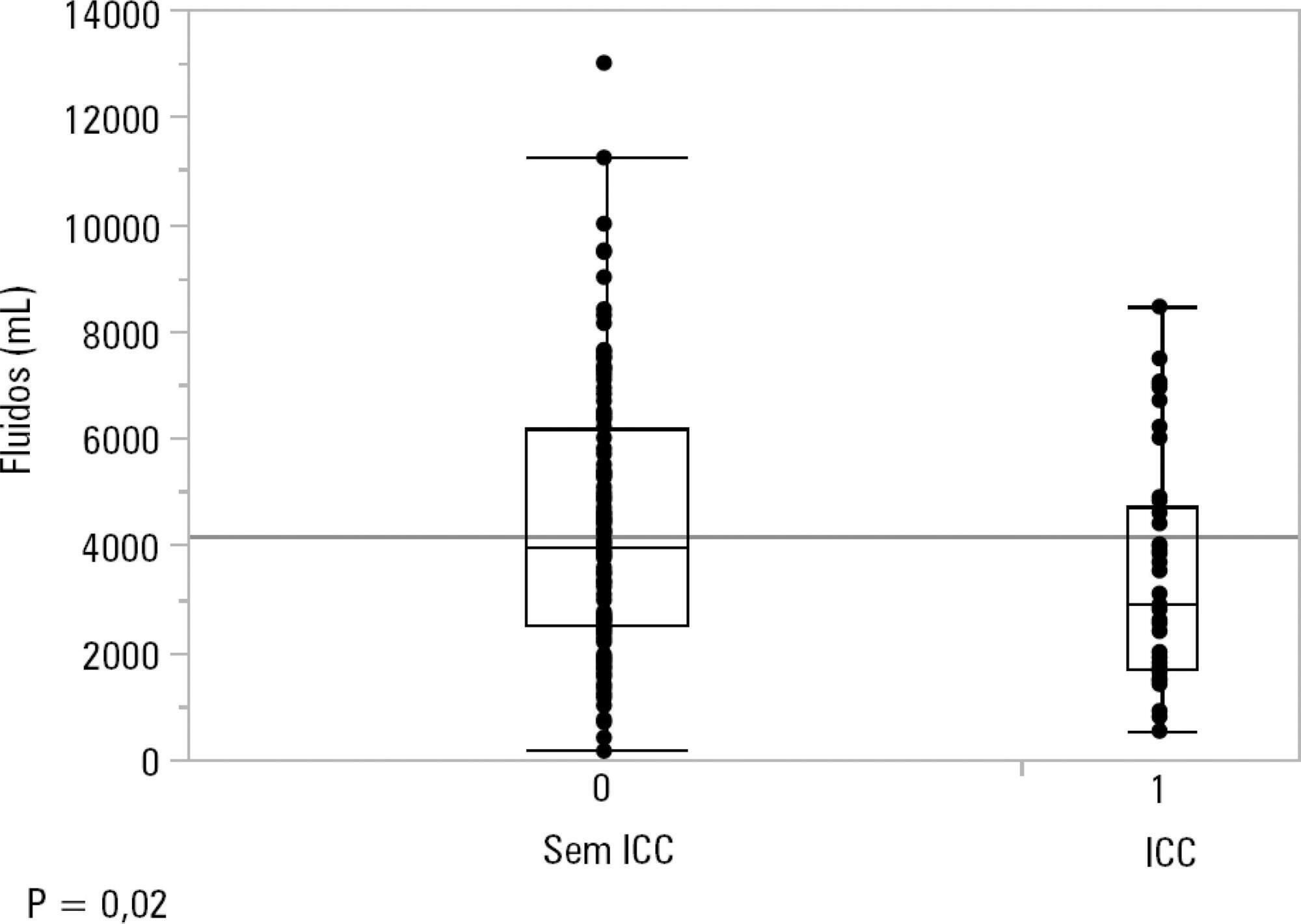
One hundred-thirty patients (72%) received ≥ 30mL/kg of IV fluids on admission. On univariate analyses, a past history of coronary artery disease and heart failure was associated with less fluid therapy. On multivariate analyses, a history of heart failure (OR = 2.31; 95%CI 1.04 - 5.14) remained significantly associated with receiving less IV fluids. Left ventricular ejection fraction, systolic/diastolic function, left ventricular hypertrophy and pulmonary hypertension were not associated with IV fluids. The amount of IV fluids was not associated with differences in mortality. During the first 24 hours, patients with a past history of heart failure received 2,900mLof IV fluids [1,688 - 4,714mL] versus 3,977mL [2,500 - 6,200mL] received by those without a history of heart failure, p = 0.02.
Septic patients with a past history of heart failure received 1L less IV fluids in the first 24 hours with no difference in mortality.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):347-353
DOI 10.5935/0103-507X.20190047
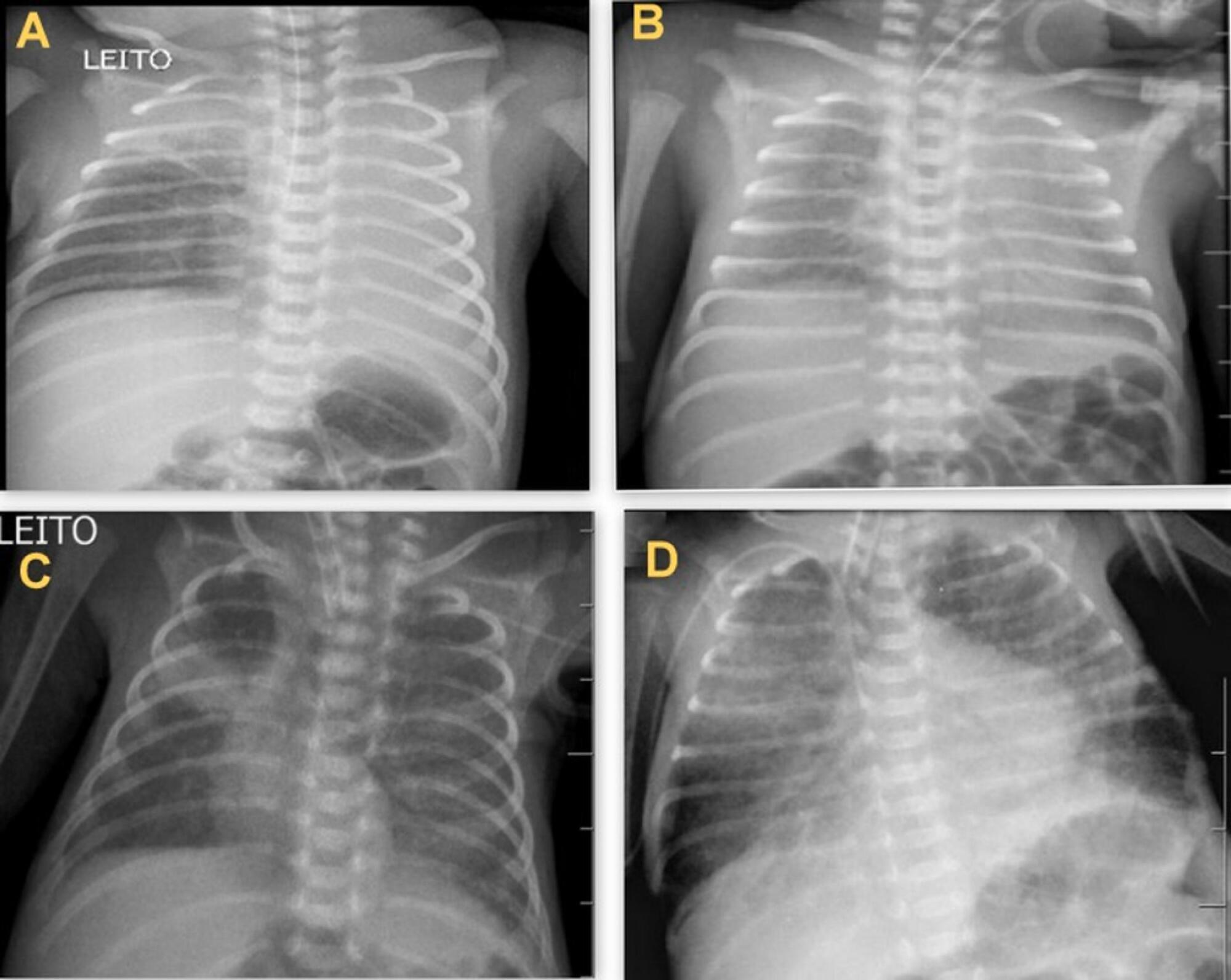
To determine the occurrence and characteristics of atelectasis, opacities, hypolucency and pulmonary infiltrates observed on chest X-rays of preterm infants in a neonatal intensive care unit.
This was a cross-sectional observational study. From August to December 2017, all chest radiographs of newborn infants were analyzed. The study included the chest radiographs of preterm neonates with gestational ages up to 36 weeks in the neonatal period that showed clear changes or suspected changes, which were confirmed after a radiologist’s report. Radiological changes were associated with possible predisposing factors.
During the study period, 450 radiographs were performed on preterm neonates, and 37 lung changes were identified and classified into 4 types: 12 (2.66%) changes were described as opacities, 11 (2.44%) were described as atelectasis, 10 (2.22%) were described as pulmonary infiltrate, and 4 (0.88%) were described as hypolucency. A higher occurrence of atelectasis was noted in the right lung (81.8%). Among the abnormal radiographs, 25 (67.6%) newborn infants were receiving invasive mechanical ventilation.
Considering the radiological report, no significance was found for the observed changes. Atelectasis was not the most frequently observed change. The predisposing factors for these changes were extreme prematurity, low weight, male sex, a poorly positioned endotracheal tube and the use of invasive mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):354-360
DOI 10.5935/0103-507X.20190058
To evaluate the agreement between intensive care physicians with similar training in the use of bedside lung ultrasonography in identifying pulmonary B lines, visualized in real time, to verify the reproducibility of the method.
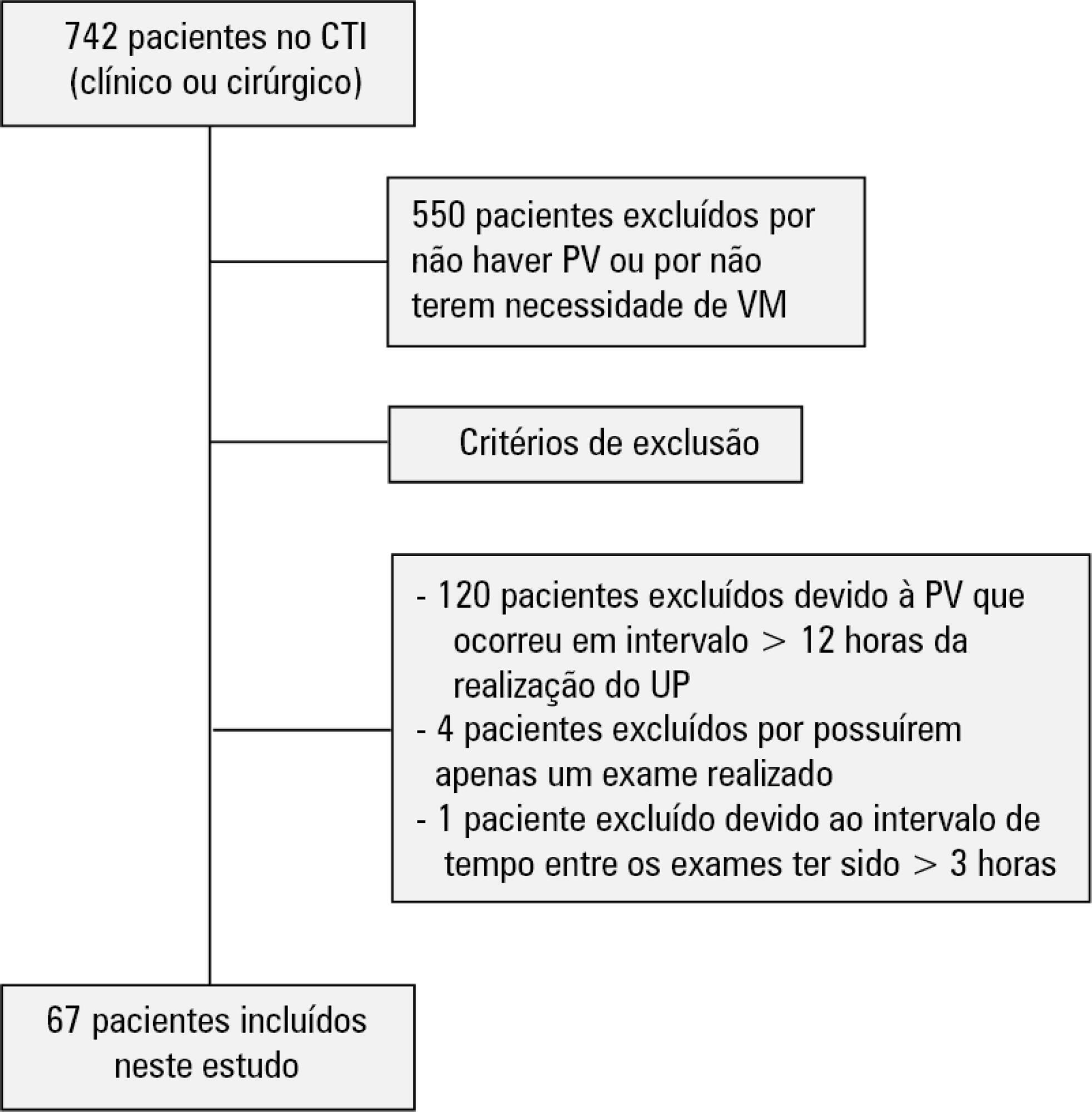
A total of 67 patients with some ventilatory deterioration identified within 12 hours after a pulmonary ultrasonography in the period from November 2016 to March 2017 were analyzed, and all were admitted to an intensive care unit of a private hospital in Belo Horizonte, Minas Gerais. The lung ultrasonographies were performed by three different professionals, termed A, B and C, and the time interval between each lung ultrasonography was less than 3 hours. The only visualized chest zones were the anterior and lateral, defined as right and left anterior (1) zones (Z1R and Z1L, respectively), which were delimited by the clavicle, the sternum and the horizontal line perpendicular to the xiphoid process and anterior axillary line. The right and left lateral (2) zones (Z2R and Z2L, respectively) covered the lateral area between the anterior and posterior axillary lines, with the lower limit being the same horizontal line corresponding to the height of the xiphoid process. A lung zone was considered positive for B lines upon visualization of three or more of these lines, suggesting the presence of alveolar-interstitial syndrome. Using the Kappa value, we evaluated the agreement among the four zones according to the execution of each pair of professionals (AB, AC and BC).
Approximately 80% of the areas that were visualized showed a moderate to substantial agreement, with the Kappa values ranging from 0.41 - 079 (p < 0.05; 95% CI). The highest levels of agreement occurred in the upper zones Z1R and Z1L between subgroups AC and BC, with a Kappa of approximately 0.65 (p < 0.001). In turn, Z2L showed one of the lowest agreements, with a Kappa of 0.36.
The possible limitation of an examiner-dependent effect on lung ultrasounds was not found in this study, suggesting the good reproducibility of this diagnostic modality at the bedside.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)