Abstract
Rev Bras Ter Intensiva. 2020;32(1):133-142
DOI 10.5935/0103-507X.20200019
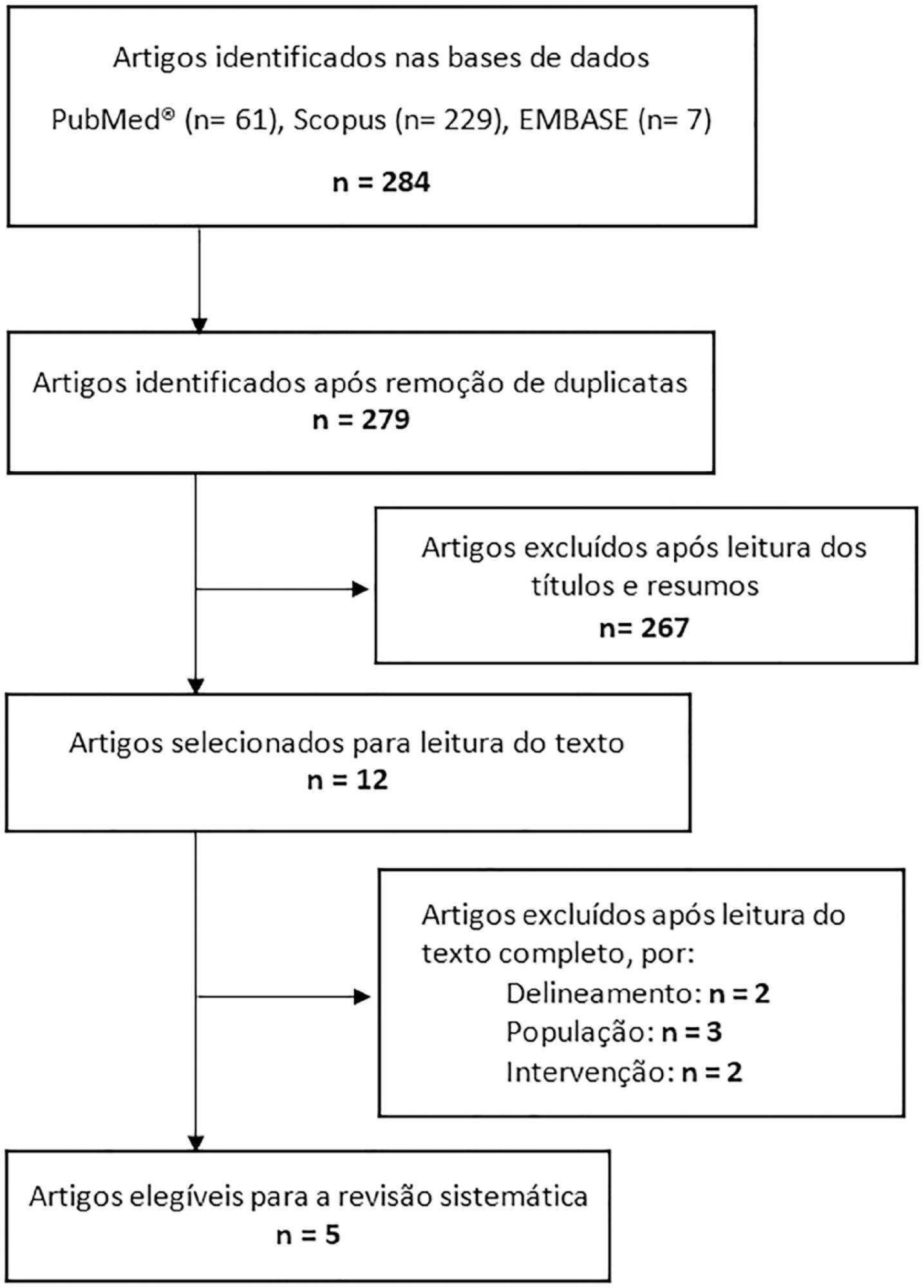
This systematic review of longitudinal studies aimed to evaluate the effect of enteral feeding of critically ill adult and pediatric patients in the prone position on gastric residual volume and other clinical outcomes. A literature search was conducted in the databases PubMed, Scopus and Embase using terms related to population and intervention. Two independent reviewers analyzed the titles and abstracts, and data collection was performed using a standardized form. Discrepancies were resolved by a third reviewer. The methodological quality of the studies was evaluated considering the potential for systematic errors, and the data were qualitatively analyzed. Four studies with adult patients and one with preterm patients were included. The gastric residual volume was evaluated as the main outcome: three studies did not show differences in the gastric residual volume between the prone and supine positions (p > 0.05), while one study showed a higher gastric residual volume during enteral feeding in the prone position (27.6mL versus 10.6mL; p < 0.05), and another group observed a greater gastric residual volume in the supine position (reduction of the gastric residual volume by 23.3% in the supine position versus 43.9% in the prone position; p < 0.01). Two studies evaluated the frequency of vomiting; one study found that it was higher in the prone position (30 versus 26 episodes; p < 0.001), while the other study found no significant difference (p > 0.05). The incidence of aspiration pneumonia and death were evaluated in one study, with no difference between groups (p > 0.05). The literature on the administration of enteral feeding in the prone position in critically ill patients is sparse and of limited quality, and the results regarding gastric residual volume are contradictory. Observational studies with appropriate sample sizes should be conducted to support conclusions on the subject.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):504-510
DOI 10.5935/0103-507X.20190067
To evaluate the risk factors for protein-caloric inadequacy in critically ill patients.
Prospective cohort study of patients hospitalized in an adult intensive care unit between February and November 2017. Patients were followed for 7 days. The conditional probability of inadequacy was calculated using the Kaplan-Meier method and the 95% log-rank test. To assess the risk of inadequacy, crude and adjusted hazard ratios (HR) were calculated using Cox regression with a 95% confidence interval.
Of the 130 patients, 63.8% were male, 73.8% were <60 years of age, and 49.2% were diagnosed with trauma. The mean APACHE II score was 24 points, and 70.0% of the patients had a protein-caloric adequacy >80%. In the univariate analysis, the significant variables for inadequacy were use of vasoactive drugs, interruptions of diet and failure to initiate nutrition early. In the final model, patients who presented with vomiting/gastric residue (adjusted HR = 22.5; 95%CI 5.14 - 98.87) and fasting for extubation (adjusted HR = 14.75; 95%CI 3.59 - 60.63) and for examinations and interventions (adjusted HR = 12.46; 95%CI 4.52 - 34.36) had a higher risk of not achieving protein-caloric adequacy.
Achievement of nutritional goals > 80.0% occurred in 70.0% of patients. The risk factors for protein-caloric inadequacy were nutritional interruptions, especially due to vomiting/gastric residue and fasting for extubation, exams and surgical procedures.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):155-162
DOI 10.5935/0103-507X.20140023
To determine the factors that influence the adequacy of enteral nutritional therapy in an intensive care unit.
This prospective observational study was conducted in an intensive care unit between 2010 and 2012. Patients >18 years of age underwent exclusive enteral nutritional therapy for ≥72 hours. The energy and protein requirements were calculated according to the ICU protocols. The data regarding enteral nutrition, the causes of non-compliance, and the biochemical test results were collected daily.
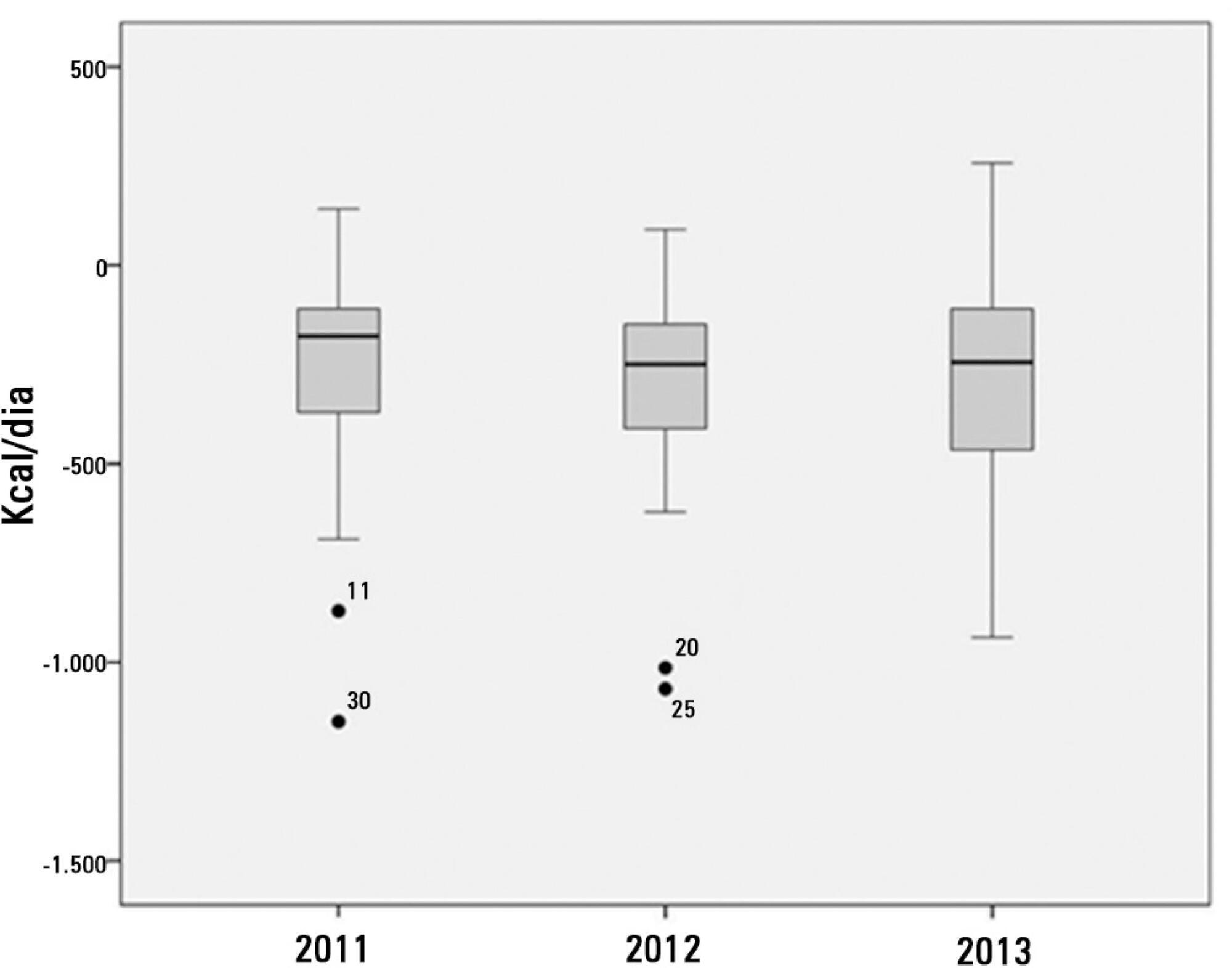
Ninety-three patients admitted to the intensive care unit were evaluated. Among these patients, 82% underwent early enteral nutritional therapy, and 80% reached the nutritional goal in <36 hours. In addition, 81.6%±15.4% of the enteral nutrition volume was infused, with an adequacy of 82.2%±16.0% for calories, 82.2%±15.9% for proteins, and a mean energy balance of -289.9±277.1kcal/day. A negative correlation of C-reactive protein with the volume infused and the energy and protein balance was observed. In contrast, a positive correlation was found between C-reactive protein and the time required to reach nutritional goals. Extubation was the main cause for interrupting the enteral nutritional therapy (29.9% of the interruption hours), and the patients >60 years of age exhibited a lower percentage of recovery of the oral route compared with the younger patients (p=0.014).
Early enteral nutritional therapy and the adequacy for both energy and protein of the nutritional volume infused were in accordance with the established guidelines. Possible inadequacies of energy and protein balance appeared to be associated with an acute inflammatory response, which was characterized by elevated C-reactive protein levels. The main cause of interruption of the enteral nutritional therapy was the time spent in extubation.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):162-167
DOI 10.5935/0103-507X.20130028
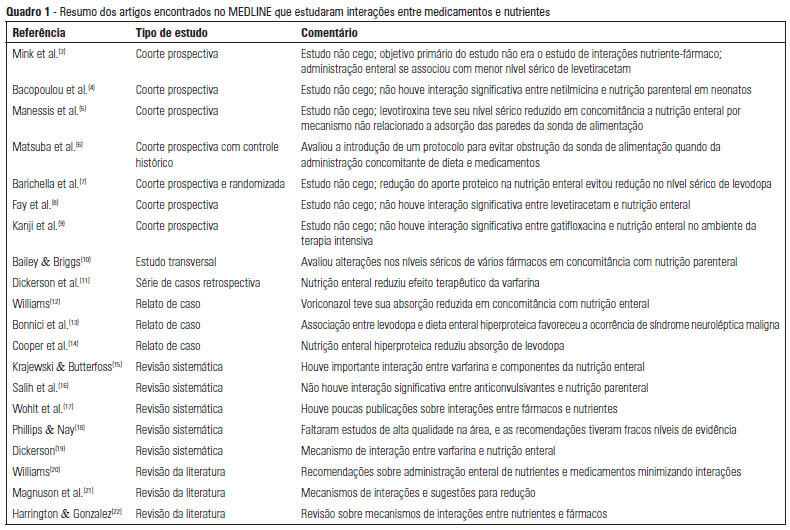
OBJECTIVE: To describe the interactions between drugs and nutrients and their frequency in the intensive care unit and to assess the professional team's awareness regarding this subject. METHODS: The keywords "drug interactions" and "nutrition therapy" were searched in the PubMed (specifically MeSH) electronic database. The studies were systematically reviewed for descriptions of the types of interactions between drugs and nutrients, including their frequency and consequences. RESULTS: Sixty-seven articles were found. Among these, 20 articles were appropriate for the methodology adopted and accomplished the objectives of the study. Of these 20 articles, 14 articles described interactions between drugs and enteral nutrition, three described interactions between drugs and parenteral nutrition, and three described the importance and care required to avoid such interactions. CONCLUSIONS: The literature about drug and nutrient interactions is limited and suggests the inability of health care teams to recognize the potential for these interactions. Possibly, the elaboration of a protocol to evaluate drug-nutrient interactions will increase the safety and efficacy of therapeutics.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):17-24
DOI 10.1590/S0103-507X2013000100005
OBJECTIVE: Evaluate the compliance of septic patients' nutritional management with enteral nutrition guidelines for critically ill patients. METHODS: Prospective cohort study with 92 septic patients, age ≥18 years, hospitalized in an intensive care unit, under enteral nutrition, evaluated according to enteral nutrition guidelines for critically ill patients, compliance with caloric and protein goals, and reasons for not starting enteral nutrition early or for discontinuing it. Prognostic scores, length of intensive care unit stay, clinical progression, and nutritional status were also analyzed. RESULTS: The patients had a mean age of 63.4±15.1 years, were predominantly male, were diagnosed predominantly with septic shock (56.5%), had a mean intensive care unit stay of 11 (7.2 to 18.0) days, had 8.2±4.2 SOFA and 24.1±9.6 APACHE II scores, and had 39.1% mortality. Enteral nutrition was initiated early in 63% of patients. Approximately 50% met the caloric and protein goals on the third day of intensive care unit stay, a percentage that decreased to 30% at day 7. Reasons for the late start of enteral nutrition included gastrointestinal tract complications (35.3%) and hemodynamic instability (32.3%). Clinical procedures were the most frequent reason to discontinue enteral nutrition (44.1%). There was no association between compliance with the guidelines and nutritional status, length of intensive care unit stay, severity, or progression. CONCLUSION: Although the number of septic patients under early enteral nutrition was significant, caloric and protein goals at day 3 of intensive care unit stay were met by only half of them, a percentage that decreased at day 7.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):49-55
DOI 10.1590/S0103-507X2013000100010
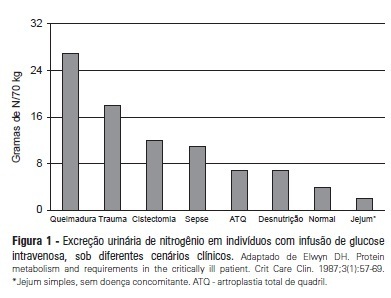
Recent evidence suggests that a negative protein balance secondary to severe disease is associated with increased morbidity. A loss of total body protein is inevitable in this scenario, even with an aggressive nutritional approach, primarily due to the catabolism of skeletal muscle fibers. The ubiquitin-proteasome system is the primary metabolic and biochemical mechanism involved in this process; paradoxically, this system consumes adenosine triphosphate as its energy source. It is possible that a neutral protein balance in these clinical situations is important for improving outcomes and achieving the caloric goals estimated or measured by indirect calorimetry. Recent studies have suggested that the use of higher protein concentrations in nutritional therapy for critically ill patients may help to reduce mortality. The purpose of this study was to review some of the nutrition therapy principles related to protein metabolism, evaluate the main assertions of the guidelines of specialty societies and review the recent studies that address these issues using critical insights from the authors' clinical experience.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):263-269
DOI 10.1590/S0103-507X2012000300010
OBJECTIVE: This study evaluated the relationship between nutritional intake and protein and caloric requirements and observed clinical outcomes on the 7th day of intensive care unit stay. METHODS: This was a retrospective cohort study of 126 patients who were admitted to the intensive care unit for >7 days. The patients were categorized according to the adequacy of energy and protein intake in relation to requirements (a >60% Adequate Intake Group and a <60% Inadequate Intake Group). The length of stay, ventilator free time and mortality in the intensive care unit and hospital were evaluated. RESULTS: Enteral nutrition was used in 95.6% of the 126 included patients, and nutrition was initiated 41 hours after admission to the intensive care unit. The adequacy of intake was 84% for energy and 72.5% for protein. No differences in the length of stay [16 (11-23) versus 15 (11-21) days, p=0.862], ventilator free time [2 (0-7) versus 3 (0-6) days, p=0.985] or mortality in the intensive care unit [12 (41.4%) versus 38 (39.1%), p=0.831] and hospital [15 (51.7%) versus 44 (45.4%), p=0.348] were observed between the adequate and inadequate energy intake groups, respectively. Similar results in protein intake and the length of hospital stay [15 (12-21) versus 15 (11-21) days, p=0.996], ventilator free time [2 (0-7) versus 3 (0-6) days, p=0.846], and mortality in the intensive care unit [15 (28.3%) versus 35 (47.9%), p=0.536)] and hospital [18 (52.9%) versus 41 (44.6%), p=0.262] were observed between groups. CONCLUSION: The results did not establish that energy and protein intakes of greater or less than 60% of nutritional requirements were reliable dividers of clinical outcomes.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):97-105
DOI 10.1590/S0103-507X2012000100015
This article reviews the literature, organizes the major findings, and generates the best evidence-based recommendations on nutrition therapy for head trauma patients. Despite recent advances in head trauma diagnosis and therapy, the mortality associated with this condition remains high. Few therapeutic interventions have been proven to effectively improve this condition. Head trauma causes multiple metabolic and electrolytic disorders; it is characterized by a hypermetabolic state that is associated with intensive catabolism, leading to specific nutritional needs. The current literature lacks specific guidelines for nutrition therapy in severe head trauma patients, although a substantial amount of data has been reported and relevant issues are currently being studied; these data may allow better nutrition therapy guidelines for these patients. In addition to a well-trained multi-disciplinary team, the following recommendations appear to improve outcomes: introducing nutrition therapy early; preferred enteral administration; appropriate energy intake; formulations that are tailored to specific patients, including appropriate nutrients; and strict electrolytic and metabolic monitoring. Understanding the pathophysiology and the consequences of therapy is fundamental.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)