Abstract
Rev Bras Ter Intensiva. 2020;32(1):133-142
DOI 10.5935/0103-507X.20200019
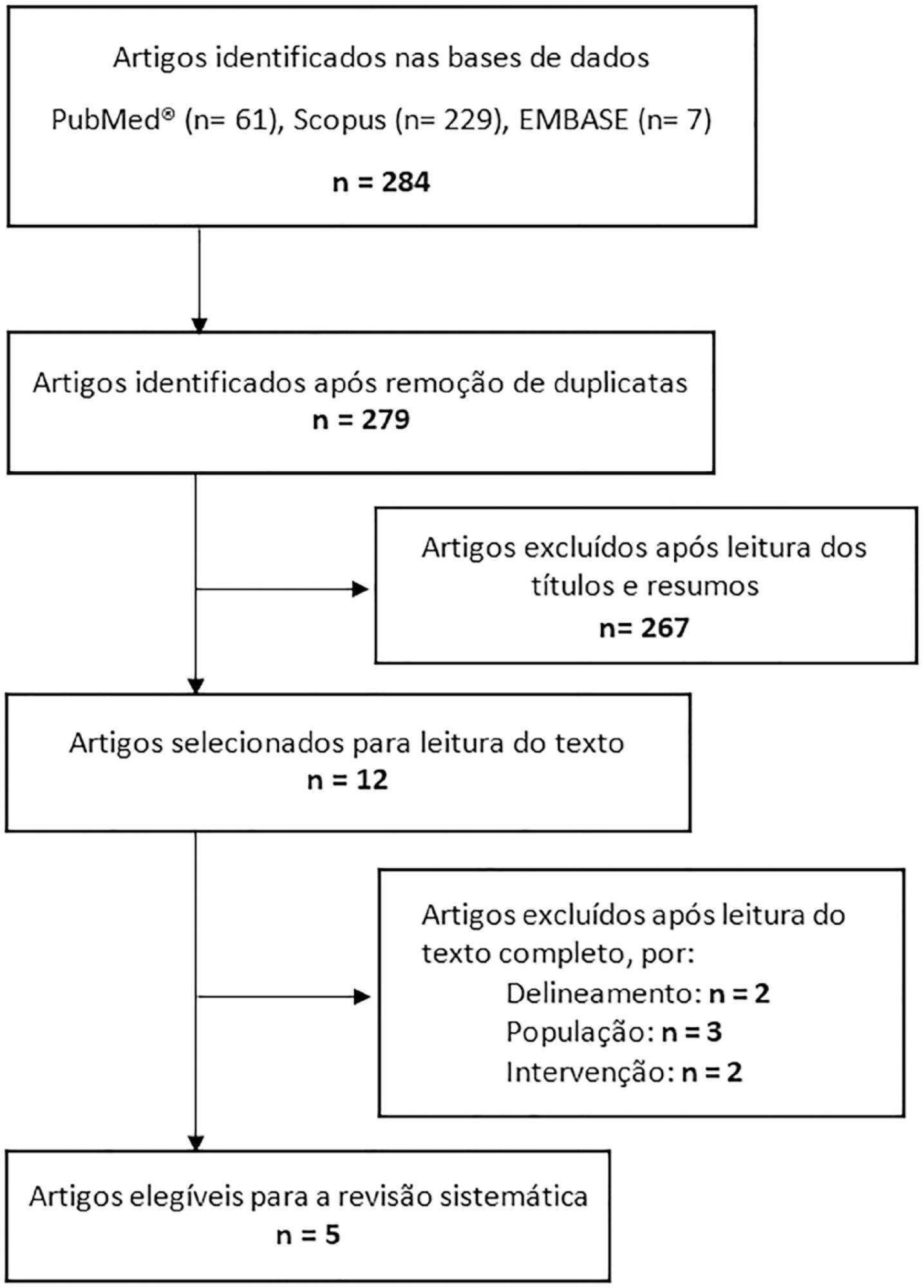
This systematic review of longitudinal studies aimed to evaluate the effect of enteral feeding of critically ill adult and pediatric patients in the prone position on gastric residual volume and other clinical outcomes. A literature search was conducted in the databases PubMed, Scopus and Embase using terms related to population and intervention. Two independent reviewers analyzed the titles and abstracts, and data collection was performed using a standardized form. Discrepancies were resolved by a third reviewer. The methodological quality of the studies was evaluated considering the potential for systematic errors, and the data were qualitatively analyzed. Four studies with adult patients and one with preterm patients were included. The gastric residual volume was evaluated as the main outcome: three studies did not show differences in the gastric residual volume between the prone and supine positions (p > 0.05), while one study showed a higher gastric residual volume during enteral feeding in the prone position (27.6mL versus 10.6mL; p < 0.05), and another group observed a greater gastric residual volume in the supine position (reduction of the gastric residual volume by 23.3% in the supine position versus 43.9% in the prone position; p < 0.01). Two studies evaluated the frequency of vomiting; one study found that it was higher in the prone position (30 versus 26 episodes; p < 0.001), while the other study found no significant difference (p > 0.05). The incidence of aspiration pneumonia and death were evaluated in one study, with no difference between groups (p > 0.05). The literature on the administration of enteral feeding in the prone position in critically ill patients is sparse and of limited quality, and the results regarding gastric residual volume are contradictory. Observational studies with appropriate sample sizes should be conducted to support conclusions on the subject.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):504-510
DOI 10.5935/0103-507X.20190067
To evaluate the risk factors for protein-caloric inadequacy in critically ill patients.
Prospective cohort study of patients hospitalized in an adult intensive care unit between February and November 2017. Patients were followed for 7 days. The conditional probability of inadequacy was calculated using the Kaplan-Meier method and the 95% log-rank test. To assess the risk of inadequacy, crude and adjusted hazard ratios (HR) were calculated using Cox regression with a 95% confidence interval.
Of the 130 patients, 63.8% were male, 73.8% were <60 years of age, and 49.2% were diagnosed with trauma. The mean APACHE II score was 24 points, and 70.0% of the patients had a protein-caloric adequacy >80%. In the univariate analysis, the significant variables for inadequacy were use of vasoactive drugs, interruptions of diet and failure to initiate nutrition early. In the final model, patients who presented with vomiting/gastric residue (adjusted HR = 22.5; 95%CI 5.14 - 98.87) and fasting for extubation (adjusted HR = 14.75; 95%CI 3.59 - 60.63) and for examinations and interventions (adjusted HR = 12.46; 95%CI 4.52 - 34.36) had a higher risk of not achieving protein-caloric adequacy.
Achievement of nutritional goals > 80.0% occurred in 70.0% of patients. The risk factors for protein-caloric inadequacy were nutritional interruptions, especially due to vomiting/gastric residue and fasting for extubation, exams and surgical procedures.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):393-402
DOI 10.5935/0103-507X.20190062
To review the scientific evidence regarding the initiation of enteral nutrition in the pediatric burn population.
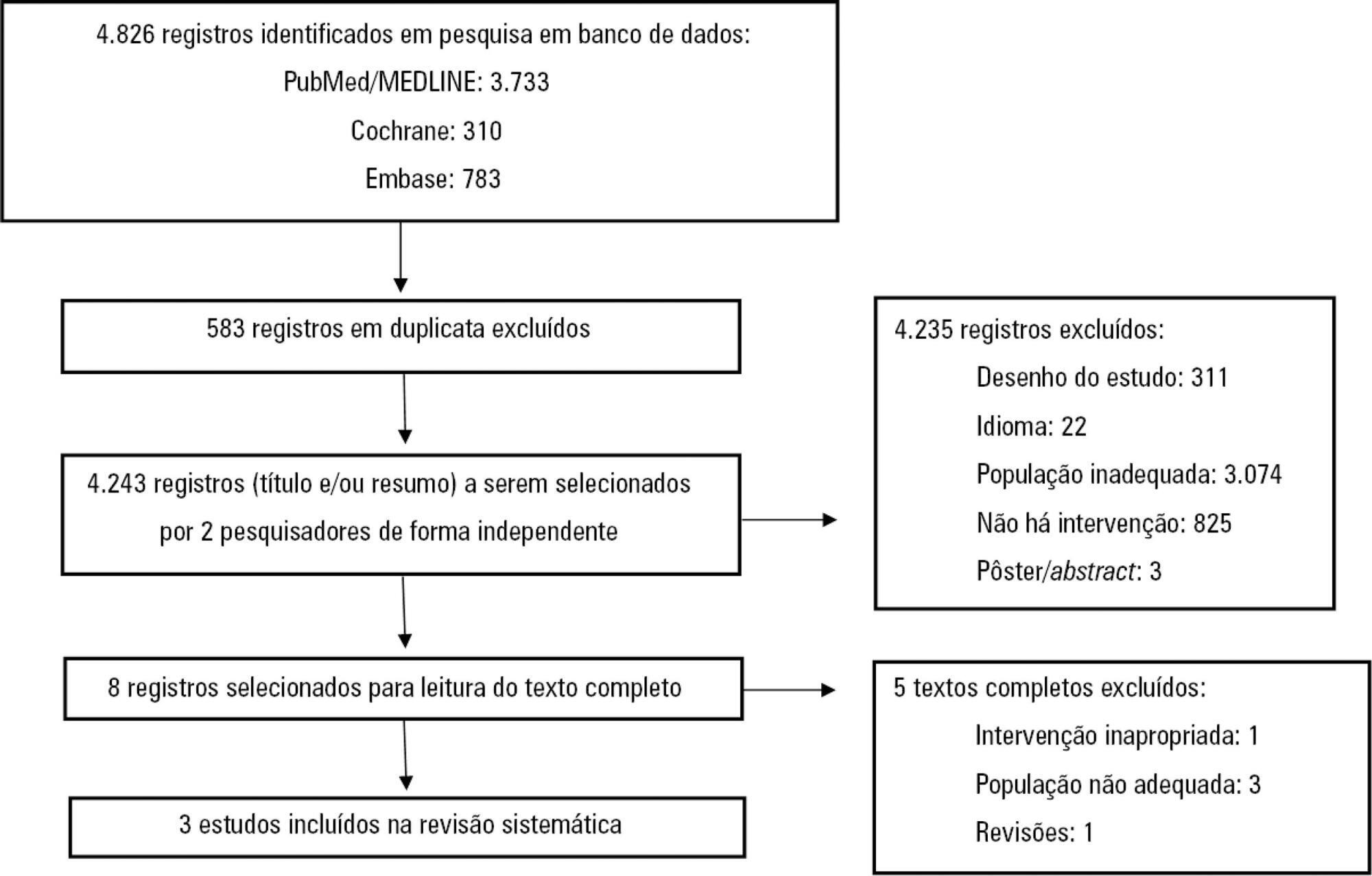
This study was a systematic review and meta-analysis of randomized clinical trials comparing early enteral nutrition and late enteral nutrition in individuals aged 1 month to 18 years with burns. The MEDLINE/PubMed, Embase and Cochrane Library databases were searched using the terms "burns", "fires", "child nutrition disorders", "nutritional support" and related terms.
Three articles that included a total of 781 patients were identified. There was no significant difference in the mortality rate between the early and late groups (OR = 0.72, 95%CI = 0.46 - 1.15, p = 0.17). Patients who received early enteral nutrition had a 3.69-day reduction in the length of hospital stay (mean difference = -3.69, 95%CI = -4.11 - -3.27, p < 0.00001). There was a higher incidence of diarrhea and vomiting and decreased intestinal permeability in the early group. This group also presented higher a serum insulin concentration and insulin/glucagon ratio as well as lower caloric deficit and weight loss when compared to the control group.
Analysis of the different intragroup variables suggests the importance of starting nutritional support early. Considering the number of pediatric burn patients, there is a need for robust studies with greater scientific impact.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):202-209
DOI 10.5935/0103-507X.20190032
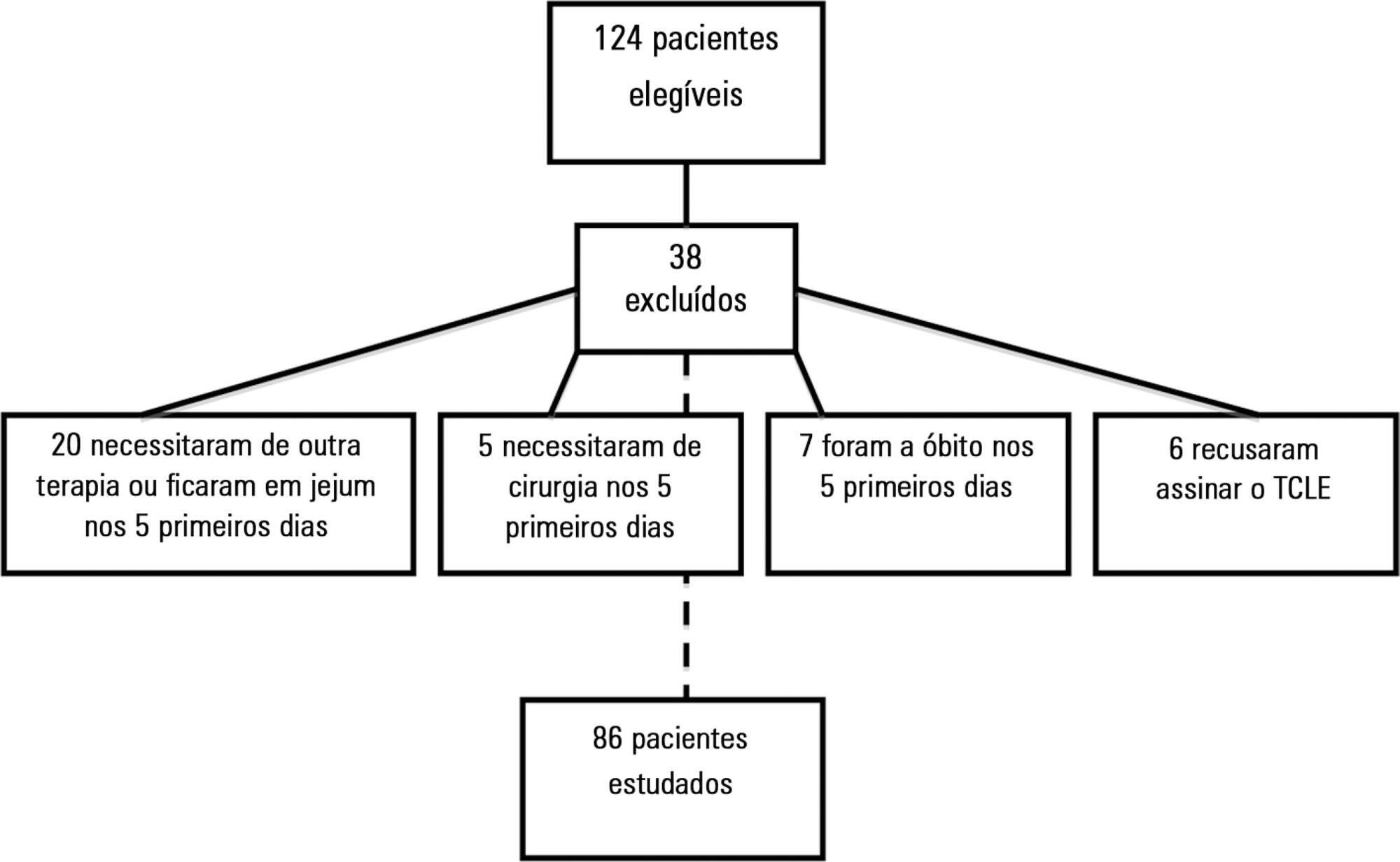
To evaluate the effects of intravenous infusion of fluids and sodium on the first day of admission on infusion of enteral nutrition in the first 5 days in intensive care patients.
A prospective cohort study was conducted with critical nonsurgical patients admitted for at least 5 days who were on mechanical ventilation and receiving enteral nutrition. The amount of intravenous fluids and sodium infused on the first day and the volume of enteral nutrition infused in the first 5 days were investigated. The volume of intravenous fluids > 35mL/kg or ≤ 35mL/kg of body weight and sodium (above or below the 25th percentile) infused on the first day was compared with infused enteral nutrition.
A total of 86 patients were studied, with a mean (± standard deviation) of 65 ± 17 years, of which 54.7% were female. On the first day, 3,393.7 ± 1,417.0mL of fluid (48.2 ± 23.0mL/kg) and 12.2 ± 5.1g of sodium were administered. Fifty-eight (67.4%) patients received more than 35mL/kg of fluids. In 5 days, 67 ± 19.8% (2,993.8 ± 1,324.4mL) of the prescribed enteral nutrition was received. Patients who received > 35mL/kg of intravenous fluids also received less enteral nutrition in 5 days (2,781.4 ± 1,337.9 versus 3,433.6 ± 1,202.2mL; p = 0.03) versus those who received ≤ 35mL/kg. Patients with intravenous sodium infusion above the 25th percentile (≥ 8.73g) on the first day received less enteral nutrition volume in 5 days (2,827.2 ± 1,398.0 versus 3,509.3 ± 911.9mL; p = 0.02).
The results of this study support the assumption that the administration of intravenous fluids > 35mL/kg and sodium ≥ 8.73g on the first day of hospitalization may contribute to the lower infusion of enteral nutrition in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):34-38
DOI 10.5935/0103-507X.20190004
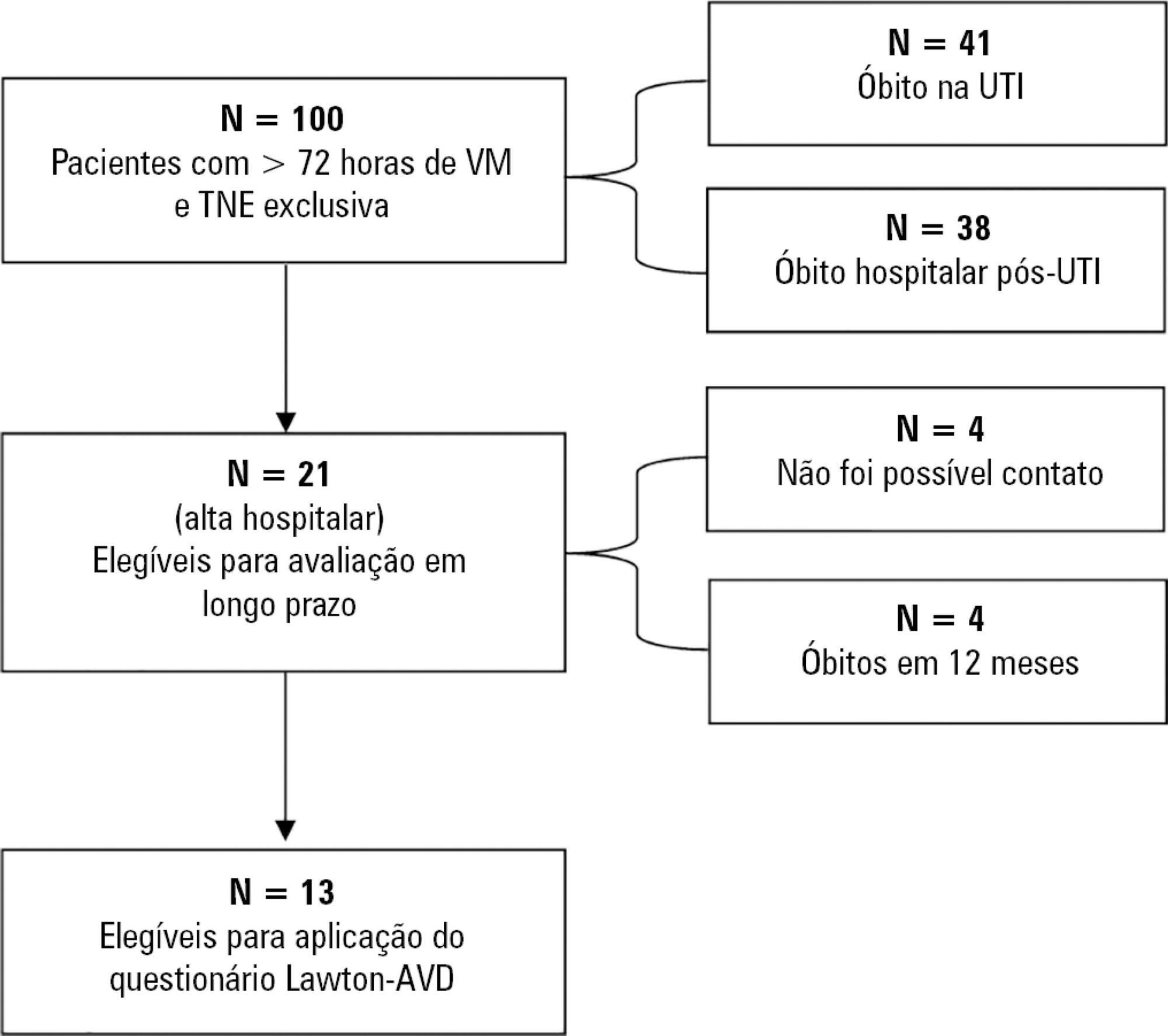
To correlate short-term (duration of mechanical ventilation and length of intensive care unit stay) and long-term (functional capacity) clinical outcomes of patients who reached nutritional adequacy ≥ 70% of predicted in the first 72 hours of hospitalization in the intensive care unit.
This was a prospective observational pilot study conducted in an 18-bed intensive care unit. A total of 100 mechanically ventilated patients receiving exclusive enteral nutritional support and receiving intensive care for more than 72 hours were included. Patients who never received enteral nutrition, those with spinal cord trauma, pregnant women, organ donors and cases of family refusal were excluded. The variables studied were nutritional adequacy ≥ 70% of predicted in the first 72 hours of hospitalization, length of intensive care unit stay, duration of mechanical ventilation and the ability to perform activities of daily living after 12 months, assessed via telephone contact using the Lawton Activities of Daily Living Scale.
The mean duration of mechanical ventilation was 18 ± 9 days, and the mean intensive care unit length of stay was 19 ± 8 days. Only 45% of the patients received more than 70% of the target nutrition in 72 hours. There was no association between nutritional adequacy and short-term (duration of mechanical ventilation, length of stay in the intensive care unit and mortality) or long-term (functional capacity and mortality) clinical outcomes.
Critically ill patients receiving caloric intake ≥ 70% in the first 72 hours of hospitalization did not present better outcomes in the short term or after 1 year.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):155-162
DOI 10.5935/0103-507X.20140023
To determine the factors that influence the adequacy of enteral nutritional therapy in an intensive care unit.
This prospective observational study was conducted in an intensive care unit between 2010 and 2012. Patients >18 years of age underwent exclusive enteral nutritional therapy for ≥72 hours. The energy and protein requirements were calculated according to the ICU protocols. The data regarding enteral nutrition, the causes of non-compliance, and the biochemical test results were collected daily.
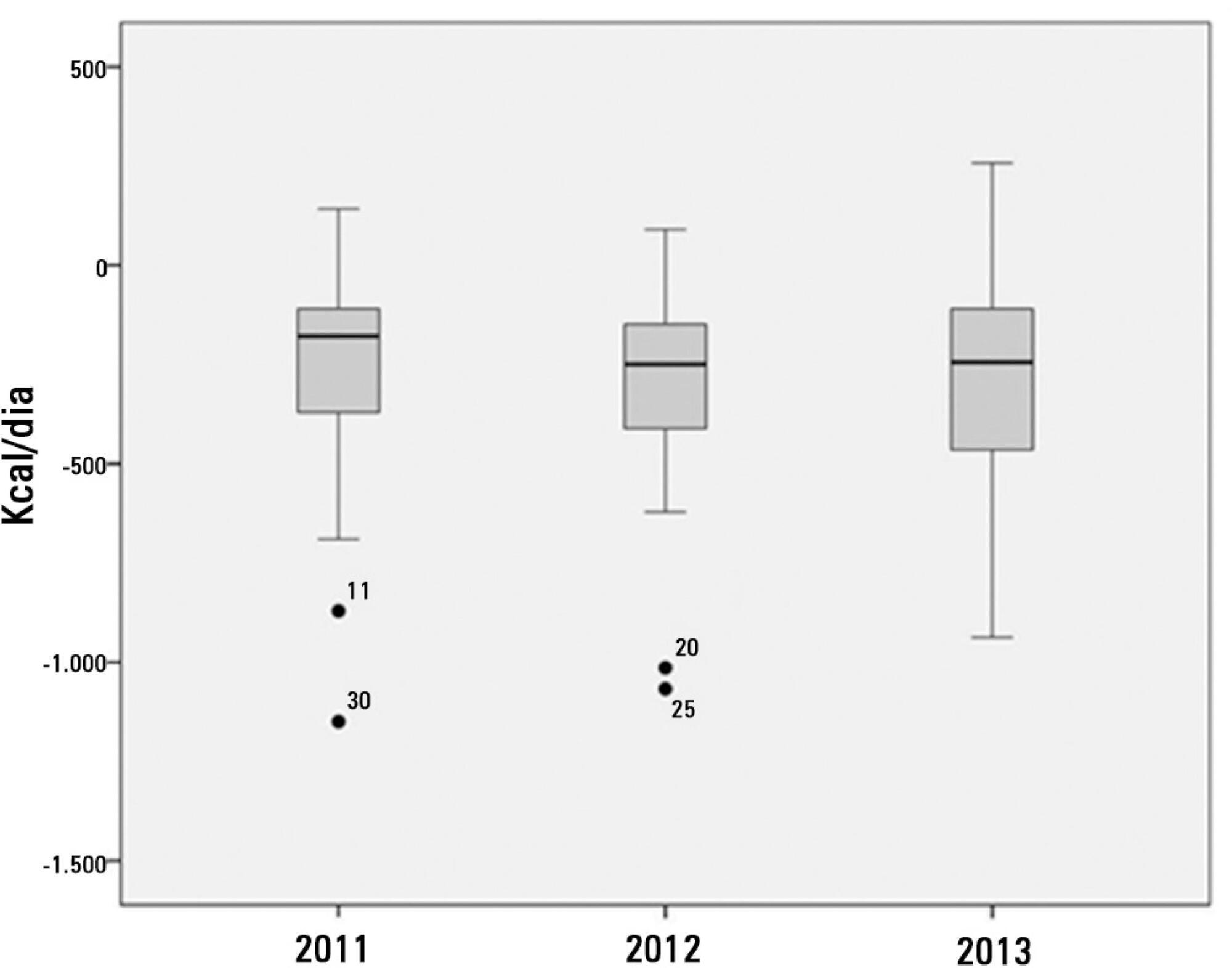
Ninety-three patients admitted to the intensive care unit were evaluated. Among these patients, 82% underwent early enteral nutritional therapy, and 80% reached the nutritional goal in <36 hours. In addition, 81.6%±15.4% of the enteral nutrition volume was infused, with an adequacy of 82.2%±16.0% for calories, 82.2%±15.9% for proteins, and a mean energy balance of -289.9±277.1kcal/day. A negative correlation of C-reactive protein with the volume infused and the energy and protein balance was observed. In contrast, a positive correlation was found between C-reactive protein and the time required to reach nutritional goals. Extubation was the main cause for interrupting the enteral nutritional therapy (29.9% of the interruption hours), and the patients >60 years of age exhibited a lower percentage of recovery of the oral route compared with the younger patients (p=0.014).
Early enteral nutritional therapy and the adequacy for both energy and protein of the nutritional volume infused were in accordance with the established guidelines. Possible inadequacies of energy and protein balance appeared to be associated with an acute inflammatory response, which was characterized by elevated C-reactive protein levels. The main cause of interruption of the enteral nutritional therapy was the time spent in extubation.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):17-24
DOI 10.1590/S0103-507X2013000100005
OBJECTIVE: Evaluate the compliance of septic patients' nutritional management with enteral nutrition guidelines for critically ill patients. METHODS: Prospective cohort study with 92 septic patients, age ≥18 years, hospitalized in an intensive care unit, under enteral nutrition, evaluated according to enteral nutrition guidelines for critically ill patients, compliance with caloric and protein goals, and reasons for not starting enteral nutrition early or for discontinuing it. Prognostic scores, length of intensive care unit stay, clinical progression, and nutritional status were also analyzed. RESULTS: The patients had a mean age of 63.4±15.1 years, were predominantly male, were diagnosed predominantly with septic shock (56.5%), had a mean intensive care unit stay of 11 (7.2 to 18.0) days, had 8.2±4.2 SOFA and 24.1±9.6 APACHE II scores, and had 39.1% mortality. Enteral nutrition was initiated early in 63% of patients. Approximately 50% met the caloric and protein goals on the third day of intensive care unit stay, a percentage that decreased to 30% at day 7. Reasons for the late start of enteral nutrition included gastrointestinal tract complications (35.3%) and hemodynamic instability (32.3%). Clinical procedures were the most frequent reason to discontinue enteral nutrition (44.1%). There was no association between compliance with the guidelines and nutritional status, length of intensive care unit stay, severity, or progression. CONCLUSION: Although the number of septic patients under early enteral nutrition was significant, caloric and protein goals at day 3 of intensive care unit stay were met by only half of them, a percentage that decreased at day 7.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)