Abstract
Rev Bras Ter Intensiva. 2019;31(3):393-402
DOI 10.5935/0103-507X.20190062
To review the scientific evidence regarding the initiation of enteral nutrition in the pediatric burn population.
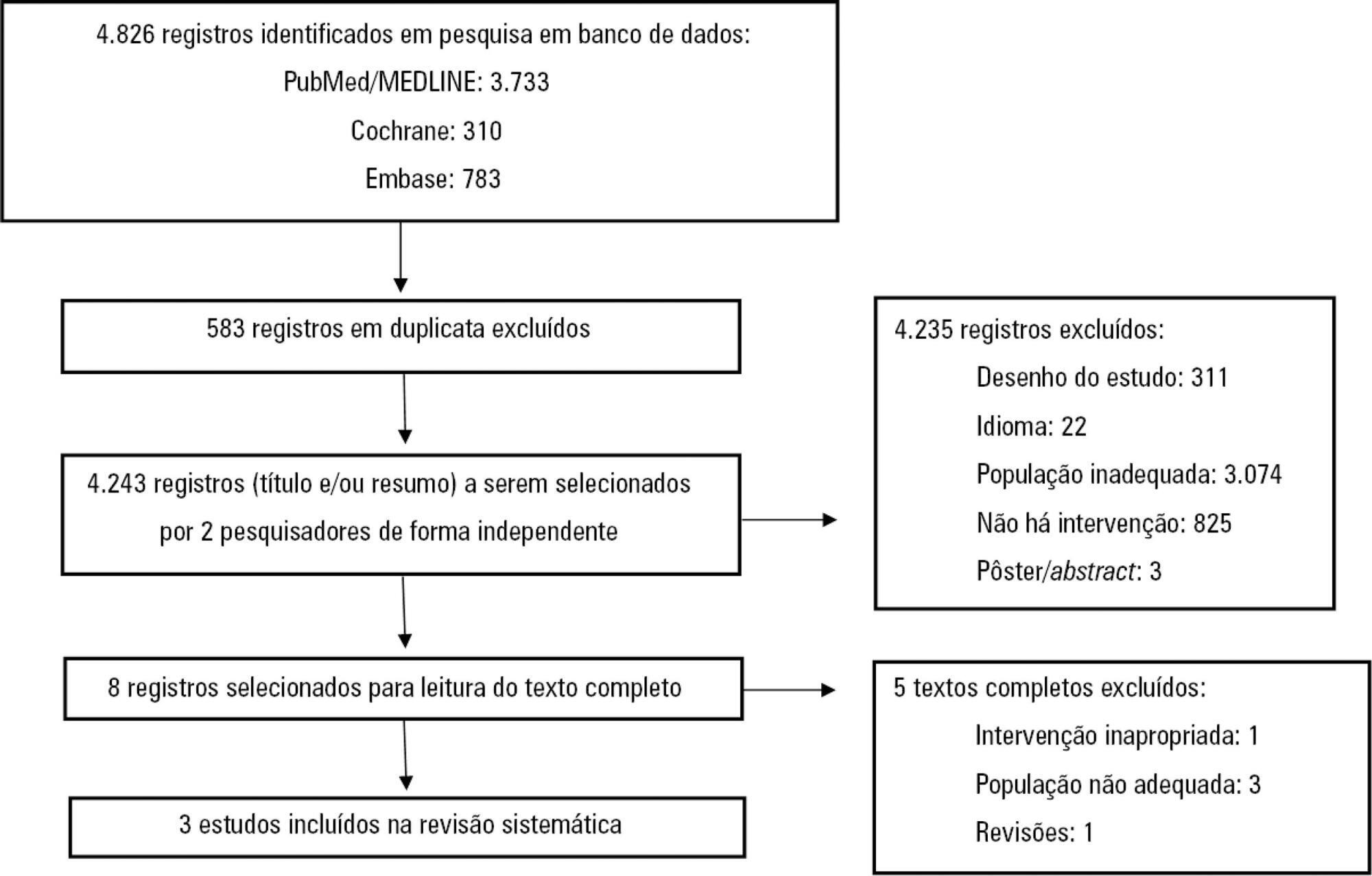
This study was a systematic review and meta-analysis of randomized clinical trials comparing early enteral nutrition and late enteral nutrition in individuals aged 1 month to 18 years with burns. The MEDLINE/PubMed, Embase and Cochrane Library databases were searched using the terms "burns", "fires", "child nutrition disorders", "nutritional support" and related terms.
Three articles that included a total of 781 patients were identified. There was no significant difference in the mortality rate between the early and late groups (OR = 0.72, 95%CI = 0.46 - 1.15, p = 0.17). Patients who received early enteral nutrition had a 3.69-day reduction in the length of hospital stay (mean difference = -3.69, 95%CI = -4.11 - -3.27, p < 0.00001). There was a higher incidence of diarrhea and vomiting and decreased intestinal permeability in the early group. This group also presented higher a serum insulin concentration and insulin/glucagon ratio as well as lower caloric deficit and weight loss when compared to the control group.
Analysis of the different intragroup variables suggests the importance of starting nutritional support early. Considering the number of pediatric burn patients, there is a need for robust studies with greater scientific impact.
Abstract
Rev Bras Ter Intensiva. 2014;26(3):299-304
DOI 10.5935/0103-507X.20140042
To assess the opinions and practices of intensive care professionals with regard to diarrhea in critically ill patients.
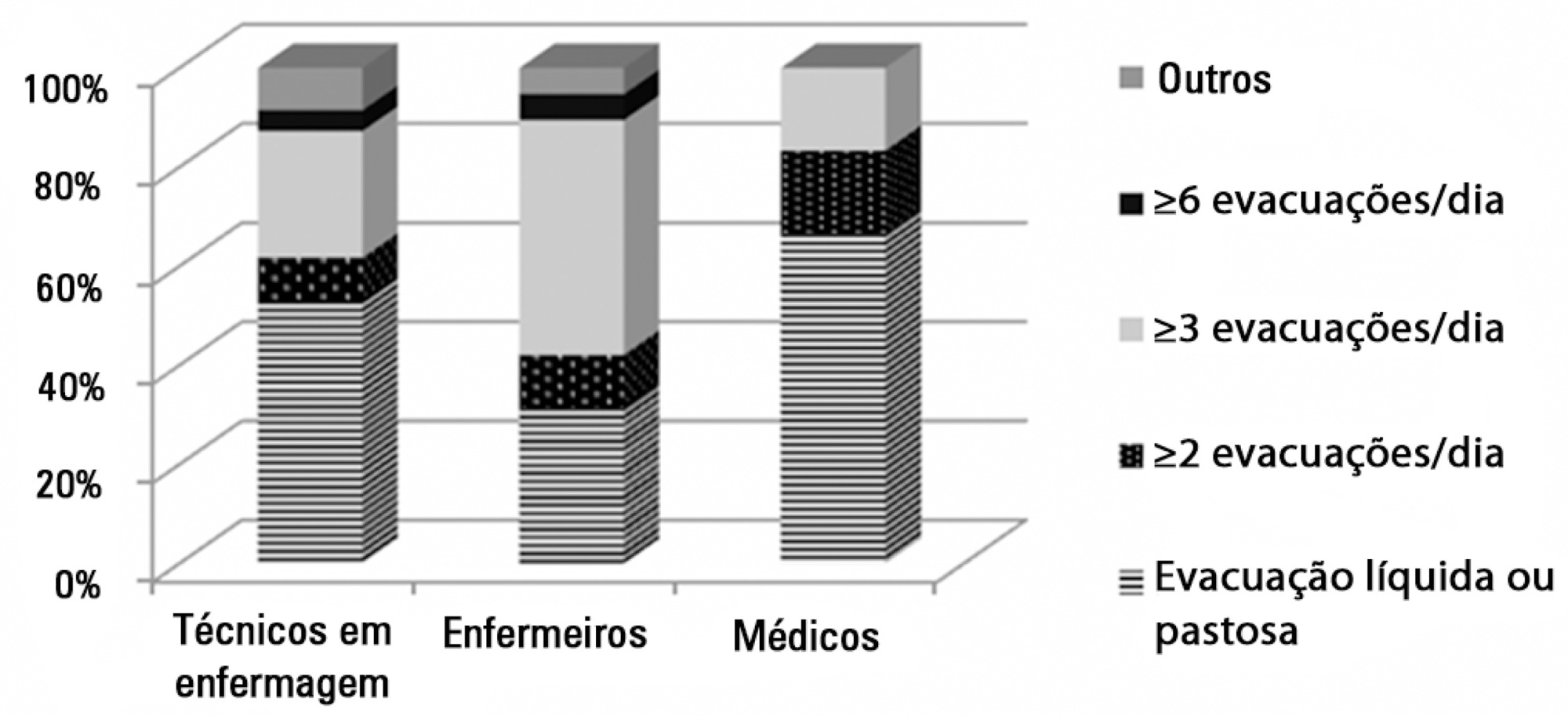
A multicenter cross-sectional study was conducted among health care professionals working at three adult intensive care units. Participants responded individually to a self-administered questionnaire about their length of work experience in intensive care; the definition, characterization, and causes of diarrhea; types of records in the patient's medical record; and training received.
A total of 78 professionals participated in this study, of whom 59.0% were nurse technicians, 25.7% were nurses, and 15.3% were physicians; 77.0% of them had worked in intensive care for over 1 year. Only 37.2% had received training on this topic. Half of the interviewees defined diarrhea as "liquid and/or pasty stools" regardless of frequency, while the other 50.0% defined diarrhea based on the increased number of daily bowel movements. The majority of them mentioned diet as the main cause of diarrhea, followed by "use of medications" (p<0.001). Distinct nutritional practices were observed among the analyzed professionals regarding episodes of diarrhea, such as discontinuing, maintaining, or reducing the volume of enteral nutrition; physicians reported that they do not routinely communicate the problem to other professionals (for example, to a nutritionist) and do not routinely record and quantify diarrhea events in patients' medical records.
Different opinions and practices were observed in intensive care professionals with regard to diarrhea.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):157-161
DOI 10.1590/S0103-507X2012000200010
OBJECTIVE: Because patients hospitalized in intensive care units are at risk for poor nutrition, and nutritional therapy is not always started at an appropriate time, the present study aimed to correlate nutritional status, early nutrition, and hyperglycemia with patient mortality in an intensive care unit. METHODS: This archival cohort study used the secondary database of 453 patients who stayed at least 48 hours in an intensive care unit and were assessed for 8 days of hospitalization. Patient nutritional status was defined according to the body mass index. Early nutrition was defined as an feeding energy within the first 48 hours of hospitalization, regardless of the administration route. Blood glucose levels were monitored using a glucometer. RESULTS: A majority of patients were male (54.2%), and approximately half of patients were overweight (48.4%). At the end of the first 48 hours, 69.4% of patients had received nutrition, and only 13.5% of patients still exhibited hyperglycemia. The patients who received early nutritional therapy exhibited lower a mortality risk (p = 0.002), regardless of the presence of other factors associated with mortality. CONCLUSIONS: The significant correlation between early nutritional therapy and survival emphasizes the importance of nutrition in severely ill patients. The low frequency of hyperglycemia found in this study might indicate that the prescription of nutritional therapy and the application of an insulin protocol are appropriate at institutional intensive care units.
Abstract
Rev Bras Ter Intensiva. 2010;22(4):346-350
DOI 10.1590/S0103-507X2010000400006
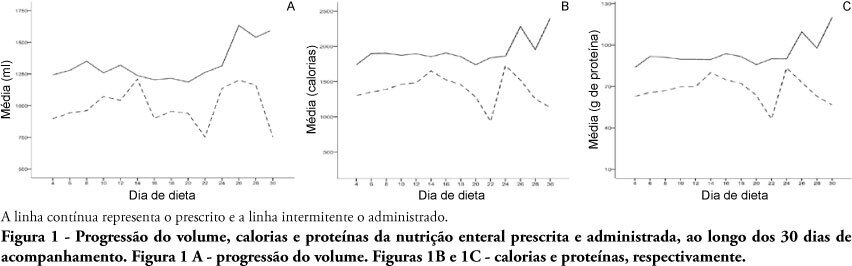
OBJECTIVES: Different conditions require that critically ill patients to receive lower than prescribed enteral nutrition volumes, energy and protein. This study objective was to evaluate the prescribed versus administered enteral nutrition difference in adults admitted to an intensive care unit. METHODS: In 2009, patients were followed for 30 days from the start of enteral nutrition to its discontinuation, or discharge from the intensive care unit. Parametric and nonparametric tests were used to evaluate prescribed versus administered differences. RESULTS: Eighty five patients were enrolled; mean age was 58.6±18.0 years and 40% were male. The patients remained in hospital for 29.5 days (IQ: 15.2 - 48.7) and were under enteral nutrition for 10 (IQ: 4.2 - 27.5) days. Lower than enteral nutrition prescribed volume (-428±243ml/day), energy (-665±412 Kcal/day) and protein (-30±19 g protein/day) was received. Individual patients' evaluation demonstrated that about 40% of the prescribed volume was not actually given. The main reasons for enteral nutrition interruptions were nausea and vomiting, abdominal distension, constipation and clinical complications (52%); diagnostic procedures (41.6%); and transition to oral feeding (5.6%). CONCLUSION: Patients admitted to intensive care unit receive less than the prescribed enteral nutrition. The routine care and gastrointestinal tract complications lead to enteral nutrition interruptions, contributing to less than prescribed calories administration.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):376-383
DOI 10.1590/S0103-507X2009000400007
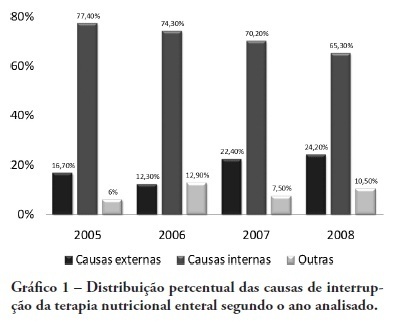
OBJECTIVE: Monitor the adequacy of enteral nutritional therapy at the intensive care unit aiming to improve the quality of nutritional assistance. METHODS: Prospective and observational study developed at the adult intensive care unit from 2005 to 2008. Patients over 18 years of age with exclusive enteral nutritional therapy for over 72h participated in the sample. The average values and the percentile adequacy of energy and proteins calculated, prescribed and administered in each year were analyzed. The factors responsible for the non-conformity of the administration planned were classified into intensive care unit extrinsic or intrinsic causes. The quality indicators proposed by the ILSI Brazil were applied, and expressed into percentile goals. In the statistic analyses, confidence interval and the t Student e Mann-Whitney (p<0.05) tests were used, according to the Epi Info program. RESULTS: One hundred and sixteen patients were followed up. There were statically difference in values of energy and protein administered in 2005 and in 2006, when compared to those in 2008. The adequacy calculated/prescribed remained close to 100% in all the surveys and the adequacy administered/prescribed increased from 74% in 2005, to 89% in 2008. An increase in interruptions of enteral nutritional therapy for external factors and the decrease in interruptions for intensive care unit internal factors were verified. The quality indicators equally reflect the evolution of the patient care. CONCLUSION: In the four yearly surveys, a progressive enhancement of nutritional support was verified. Quality indicators allow nutritional care evolution monitoring, the comparison to other services data, and are a new perspective for enteral nutritional therapy assessment.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):241-248
DOI 10.1590/S0103-507X2008000300006
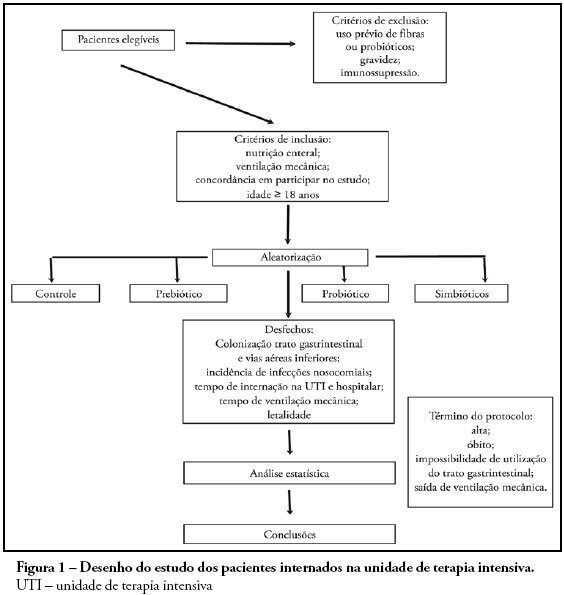
OBJECTIVES: Sepsis is the main cause of death in the intensive care unit. New preventive measures for nosocomial infections have been researched, such as pre, pro and symbiotic usage, due to its immunoregulatory properties. The objective was to evaluate the effect of administration of pre, pro and symbiotic on gastrointestinal and inferior airway colonization and on nosocomial infections, particularly ventilator-associated pneumonia. METHODS: Patients who were admitted to the intensive care unit at Hospital Universitário Clementino Fraga Filho between November 2004 and September 2006 and mechanically ventilated were randomized in one of four groups: control (n = 16), prebiotic (n = 10), probiotic (n = 12) or symbiotic (n = 11). Treatment was administered for fourteen days. Outcomes measured were: a) Colonization of the gastrointestinal tract and trachea; b) incidence of nosocomial infections, particularly ventilator associated pneumonia; c) duration of mechanical ventilation, length of stay in the intensive care unit, duration of hospitalization, mortality rates, and d) development of organ dysfunction. RESULTS: Forty-nine patients were evaluated. intensive care unit's mortality was 34% and in-hospital mortality was 53%, APACHE II median was 20 (13 -25). The groups were matched at admission. There was no difference between the groups in relation to the incidence of ventilator associated pneumonia or nosocomial infection. There was a non-significant increase in the proportion of enterobacteria in the trachea at the seventh day in the pre and probiotic groups compared to control. There was a non-significant decrease in the number of bacteria found in the stomach in the pre, pro and symbiotic group at day 7. No significant difference, in regards to the remaining measured parameters, could be found. CONCLUSIONS: Probiotic therapy was not efficient in the prevention of nosocomial infection but there was a tendency to reduction in tracheal colonization by non-fermenting bacteria.
Abstract
Rev Bras Ter Intensiva. 2007;19(1):90-97
DOI 10.1590/S0103-507X2007000100012
BACKGROUND AND OBJECTIVES: The purpose of this review is to approach the main necessary aspects for the accomplishment of safety and efficient nutritional therapy to the critically ill patient. CONTENTS: Bibliographical survey with didactic books and scientific articles was made in Portuguese, English and Spanish with results of the last 20 years. Nutritional support is an integrant part in the care of patients in intensive care units. The success of the nutritional therapy involves the stages of nutritional assessment, determines the route of diet infusion and the calories and nutrients needs. CONCLUSIONS: The use of nutrients with immune function (immunonutrients) is each more frequents, however, its use is not well established for critical illness. More clinical studies are necessary to establish the best form to nourish the critical ill patient.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)