Abstract
Rev Bras Ter Intensiva. 2018;30(1):116-120
DOI 10.5935/0103-507X.20180002
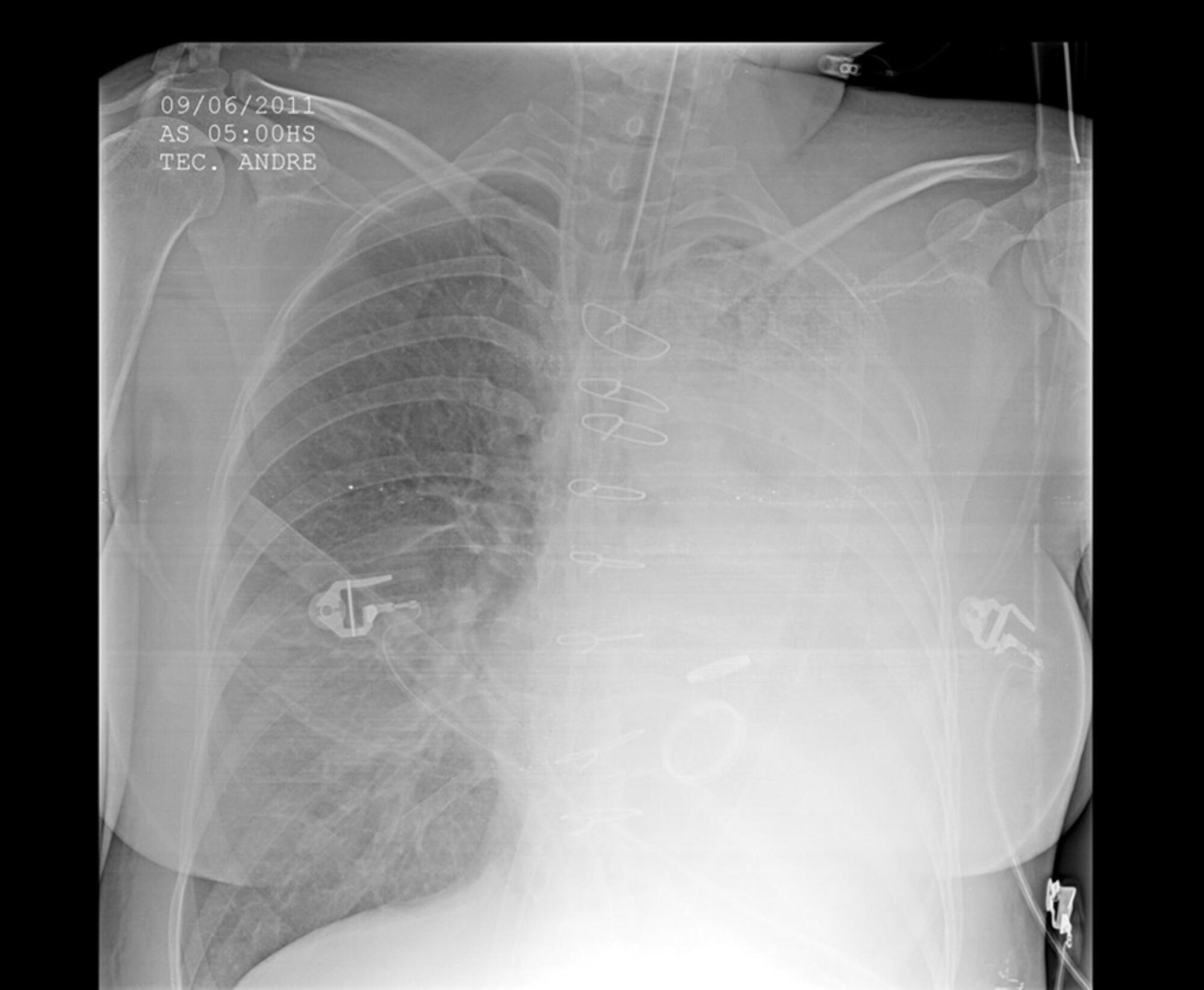
Extracorporeal membrane oxygenation has been used to treat refractory hypoxemia in numerous clinical scenarios. The fundamental principles for the management of massive hemoptysis patients include protecting the airway and healthy lung, locating the source of bleeding and controlling the hemorrhage. We report the case of a patient with acute respiratory failure associated with massive hemoptysis secondary to lung laceration during cardiac surgery. The use of extracorporeal membrane oxygenation allowed patient survival. However, due to the great difficulty in managing pulmonary clots after hemoptysis, it was necessary to use an unusual therapy involving endobronchial infusion of a thrombolytic agent as described in rare cases in the literature.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):127-130
DOI 10.5935/0103-507X.20180019
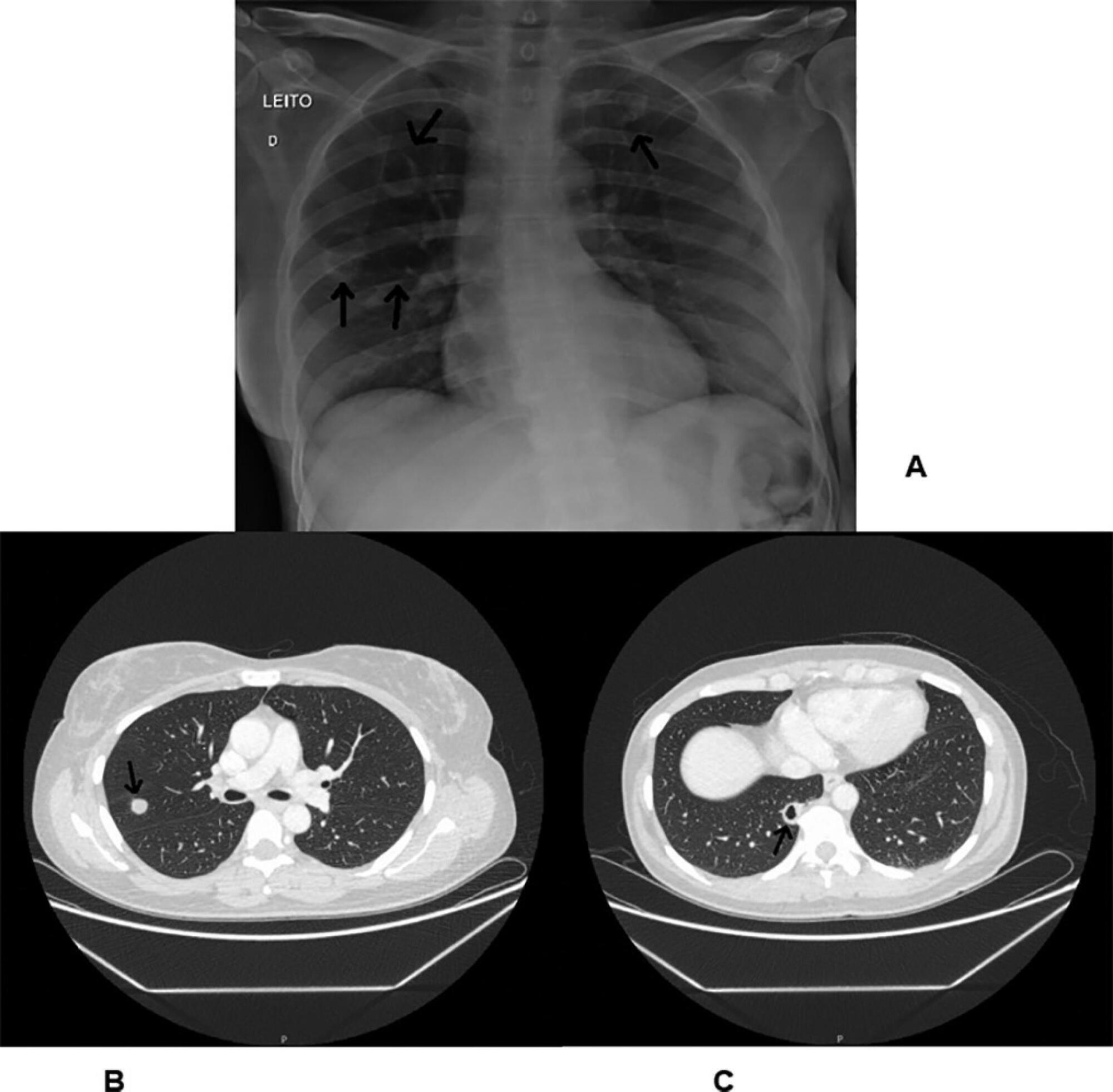
In the 2014 - 2015 season, most influenza infections were due to A (H3N2) viruses. More than two-thirds of circulating A (H3N2) viruses are antigenically and genetically different (drifted) from the A (H3N2) vaccine component of 2014 - 2015 northern and southern Hemisphere seasonal influenza vaccines. The purpose of this paper is to report a case of seasonal influenza A non-H1N1 infection that occurred in June 2015 in an adult cystic fibrosis patient with severe lung disease previously vaccinated with the anti-flu trivalent vaccine. The patient evolved to respiratory and renal failure (without rhabdomyolysis) and was placed under mechanical ventilation and hemodialysis. The clinical outcome was positive after 39 days of hospital stay. In addition, the patient was clinically stable after 18 months of follow-up. With the recent advances in critical care medicine and in cystic fibrosis treatment, survival with advanced pulmonary disease in cystic fibrosis presents new questions and potential problems, which are still being formulated.

Abstract
Rev Bras Ter Intensiva. 2018;30(1):112-115
DOI 10.5935/0103-507X.20180017
Among the main causes of death in our country are car accidents, drowning and accidental burns. Strangulation is a potentially fatal injury and an important cause of homicide and suicide among adults and adolescents. In children, its occurrence is usually accidental. However, in recent years, several cases of accidental strangulation in children around the world have been reported. A 2-year-old male patient was strangled in a car window. The patient was admitted to the pediatric intensive care unit with a Glasgow Coma Scale score of 8 and presented with progressive worsening of respiratory dysfunction and torpor. The patient also presented acute respiratory distress syndrome, acute pulmonary edema and shock. He was managed with protective mechanical ventilation, vasoactive drugs and antibiotic therapy. He was discharged from the intensive care unit without neurological or pulmonary sequelae. After 12 days of hospitalization, he was discharged from the hospital, and his state was very good. The incidence of automobile window strangulation is rare but of high morbidity and mortality due to the resulting choking mechanism. Fortunately, newer cars have devices that stop the automatic closing of the windows if resistance is encountered. However, considering the severity of complications strangulated patients experience, the intensive neuro-ventilatory and hemodynamic management of the pathologies involved is important to reduce morbidity and mortality, as is the need to implement new campaigns for the education of parents and caregivers of children, aiming to avoid easily preventable accidents and to optimize safety mechanisms in cars with electric windows.

Abstract
Rev Bras Ter Intensiva. 2018;30(2):233-236
DOI 10.5935/0103-507X.20180029
We report the case of a female patient, 58 years of age, without known heart disease, who underwent liver transplantation without complications. On the second postoperative day, the patient developed cardiogenic shock secondary to stress-induced cardiomyopathy (Takotsubo-like syndrome). The patient was successfully managed with veno-arterial peripheral extracorporeal membrane oxygenation for 6 days, with complete recovery of cardiac function and of the hepatic graft. Coronary syndrome and acute myocarditis were excluded as the causes of the shock. The use of extracorporeal membrane oxygenation in this scenario is possible and safe, considering its specialized protocols and treatment.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):386-390
DOI 10.5935/0103-507X.20170052
Granulomatosis with polyangiitis is a rare systemic inflammatory disorder characterized by vasculitis of the small arteries, the arterioles and the capillaries together with necrotizing granulomatous lesions. This case reports on a young female patient, previously diagnosed with granulomatosis with polyangiitis, who was admitted to the intensive care unit with seizures and hemodynamic instability due to a complete atrioventricular heart block. The event was associated with multiple episodes of sustained ventricular tachycardia without any structural heart changes or electrolyte disturbances. In the intensive care unit, the patient was fitted with a provisory pacemaker, followed by immunosuppression with corticosteroids and immunobiological therapy, resulting in a total hemodynamic improvement. Severe conduction disorders in patients presenting granulomatosis with polyangiitis are rare but can contribute to increased morbidity. Early detection and specific intervention can prevent unfavorable outcomes, specifically in the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):253-258
DOI 10.5935/0103-507X.20170035
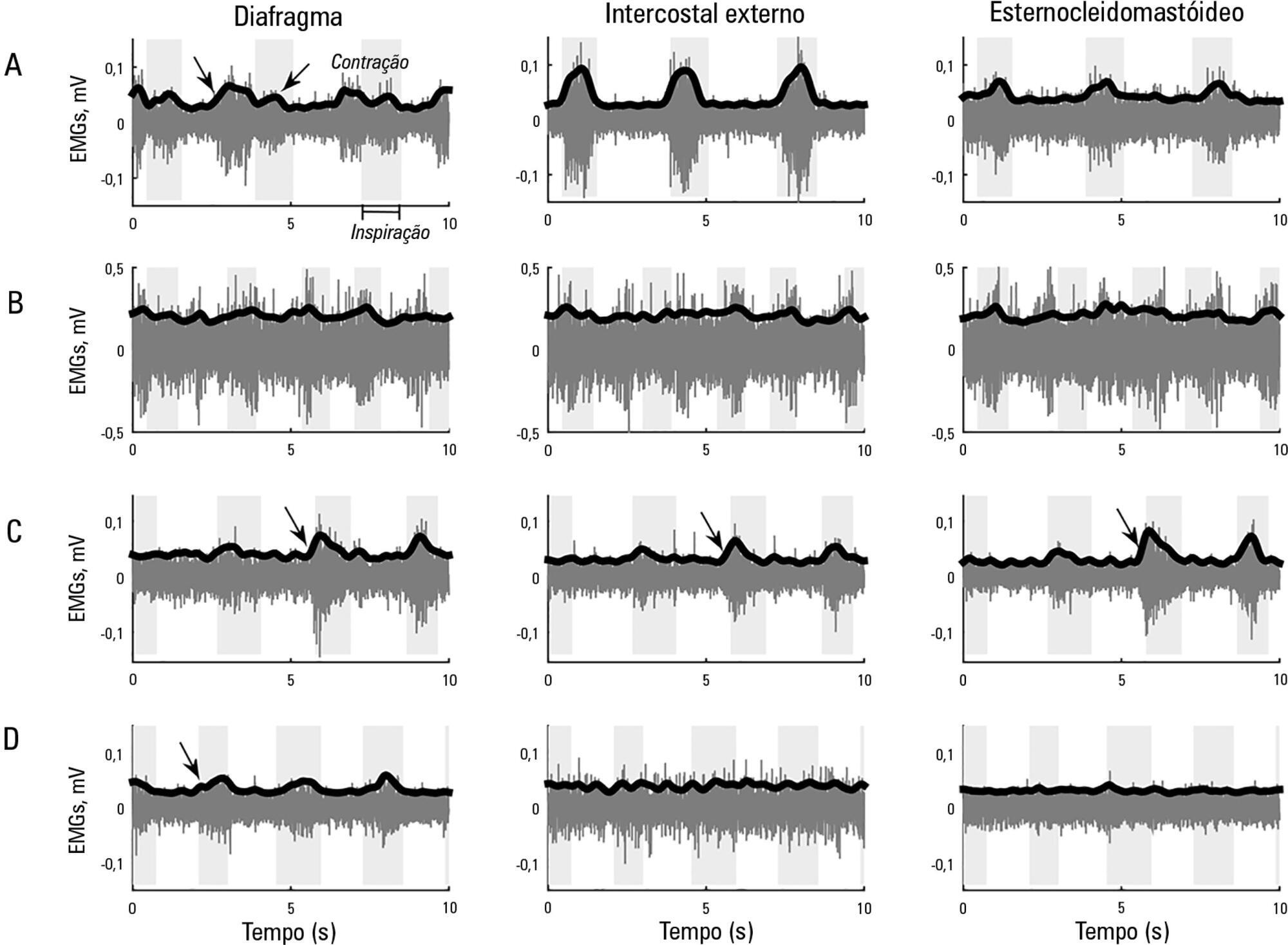
This study aimed to explore the usefulness of measuring respiratory muscle activity in mechanically ventilated patients suffering from acute organophosphate poisoning, with a view towards providing complementary information to determine the best time to suspend ventilatory support. Surface electromyography in respiratory muscles (diaphragm, external intercostal and sternocleidomastoid muscles) was recorded in a young man affected by self-poisoning with an unknown amount of parathion to determine the muscle activity level during several weaning attempts from mechanical ventilation. The energy distribution of each surface electromyography signal frequency, the synchronization between machine and patient and between muscles, acetylcholinesterase enzyme activity, and work of breathing and rapid shallow breathing indices were calculated in each weaning attempt. The work of breathing and rapid shallow breathing indices were not correlated with the failure/success of the weaning attempt. The diaphragm gradually increased its engagement with ventilation, achieving a maximal response that correlated with successful weaning and maximal acetylcholinesterase enzyme activity; in contrast, the activity of accessory respiratory muscles showed an opposite trend.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):105-110
DOI 10.5935/0103-507X.20170015
Acute respiratory distress syndrome is characterized by diffuse inflammatory lung injury and is classified as mild, moderate, and severe. Clinically, hypoxemia, bilateral opacities in lung images, and decreased pulmonary compliance are observed. Sepsis is one of the most prevalent causes of this condition (30 - 50%). Among the direct causes of acute respiratory distress syndrome, chlorine inhalation is an uncommon cause, generating mucosal and airway irritation in most cases. We present a case of severe acute respiratory distress syndrome after accidental inhalation of chlorine in a swimming pool, with noninvasive ventilation used as a treatment with good response in this case. We classified severe acute respiratory distress syndrome based on an oxygen partial pressure/oxygen inspired fraction ratio <100, although the Berlin classification is limited in considering patients with severe hypoxemia managed exclusively with noninvasive ventilation. The failure rate of noninvasive ventilation in cases of acute respiratory distress syndrome is approximately 52% and is associated with higher mortality. The possible complications of using noninvasive positive-pressure mechanical ventilation in cases of acute respiratory distress syndrome include delays in orotracheal intubation, which is performed in cases of poor clinical condition and with high support pressure levels, and deep inspiratory efforts, generating high tidal volumes and excessive transpulmonary pressures, which contribute to ventilation-related lung injury. Despite these complications, some studies have shown a decrease in the rates of orotracheal intubation in patients with acute respiratory distress syndrome with low severity scores, hemodynamic stability, and the absence of other organ dysfunctions.

Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98) Septic shock (25)