Abstract
Rev Bras Ter Intensiva. 2021;33(1):75-81
DOI 10.5935/0103-507X.20210007
To detect early respiratory and hemodynamic instability to characterize pulmonary impairment in patients with severe COVID-19.
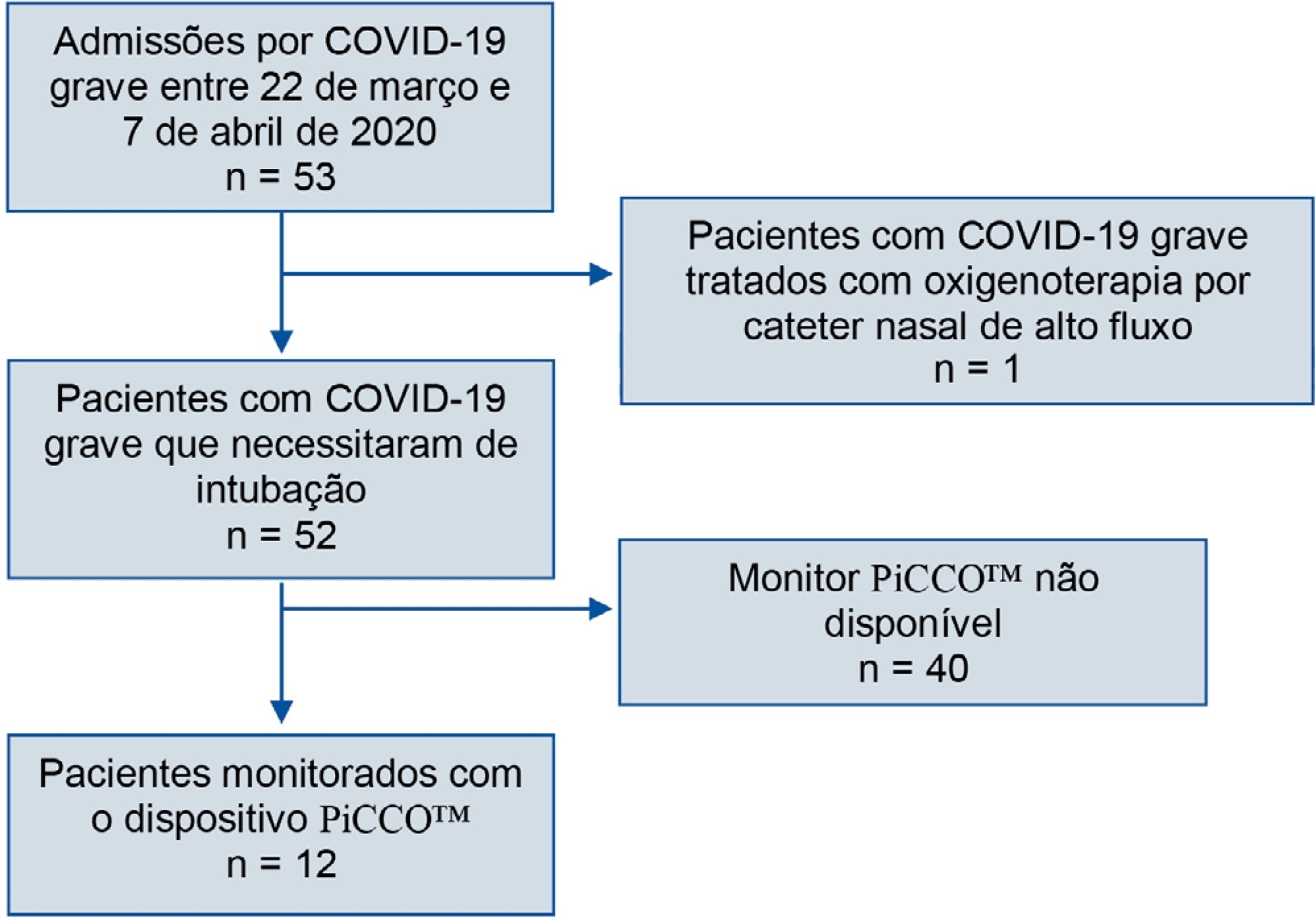
We retrospectively analyzed data collected from COVID-19 patients suffering from acute respiratory failure requiring intubation and mechanical ventilation. We used transpulmonary thermodilution assessment with a PiCCO™ device. We collected demographic, respiratory, hemodynamic and echocardiographic data within the first 48 hours after admission. Descriptive statistics were used to summarize the data.
Fifty-three patients with severe COVID-19 were admitted between March 22nd and April 7th. Twelve of them (22.6%) were monitored with a PiCCO™ device. Upon admission, the global-end diastolic volume indexed was normal (mean 738.8mL ± 209.2) and moderately increased at H48 (879mL ± 179), and the cardiac index was subnormal (2.84 ± 0.65). All patients showed extravascular lung water over 8mL/kg on admission (17.9 ± 8.9). We did not identify any argument for cardiogenic failure.
In the case of severe COVID-19 pneumonia, hemodynamic and respiratory presentation is consistent with pulmonary edema without evidence of cardiogenic origin, favoring the diagnosis of acute respiratory distress syndrome.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):112-115
DOI 10.5935/0103-507X.20180017
Among the main causes of death in our country are car accidents, drowning and accidental burns. Strangulation is a potentially fatal injury and an important cause of homicide and suicide among adults and adolescents. In children, its occurrence is usually accidental. However, in recent years, several cases of accidental strangulation in children around the world have been reported. A 2-year-old male patient was strangled in a car window. The patient was admitted to the pediatric intensive care unit with a Glasgow Coma Scale score of 8 and presented with progressive worsening of respiratory dysfunction and torpor. The patient also presented acute respiratory distress syndrome, acute pulmonary edema and shock. He was managed with protective mechanical ventilation, vasoactive drugs and antibiotic therapy. He was discharged from the intensive care unit without neurological or pulmonary sequelae. After 12 days of hospitalization, he was discharged from the hospital, and his state was very good. The incidence of automobile window strangulation is rare but of high morbidity and mortality due to the resulting choking mechanism. Fortunately, newer cars have devices that stop the automatic closing of the windows if resistance is encountered. However, considering the severity of complications strangulated patients experience, the intensive neuro-ventilatory and hemodynamic management of the pathologies involved is important to reduce morbidity and mortality, as is the need to implement new campaigns for the education of parents and caregivers of children, aiming to avoid easily preventable accidents and to optimize safety mechanisms in cars with electric windows.

Abstract
Rev Bras Ter Intensiva. 2017;29(3):279-286
DOI 10.5935/0103-507X.20170038
We aimed to investigate a potential association between B-lines and weaning failure.
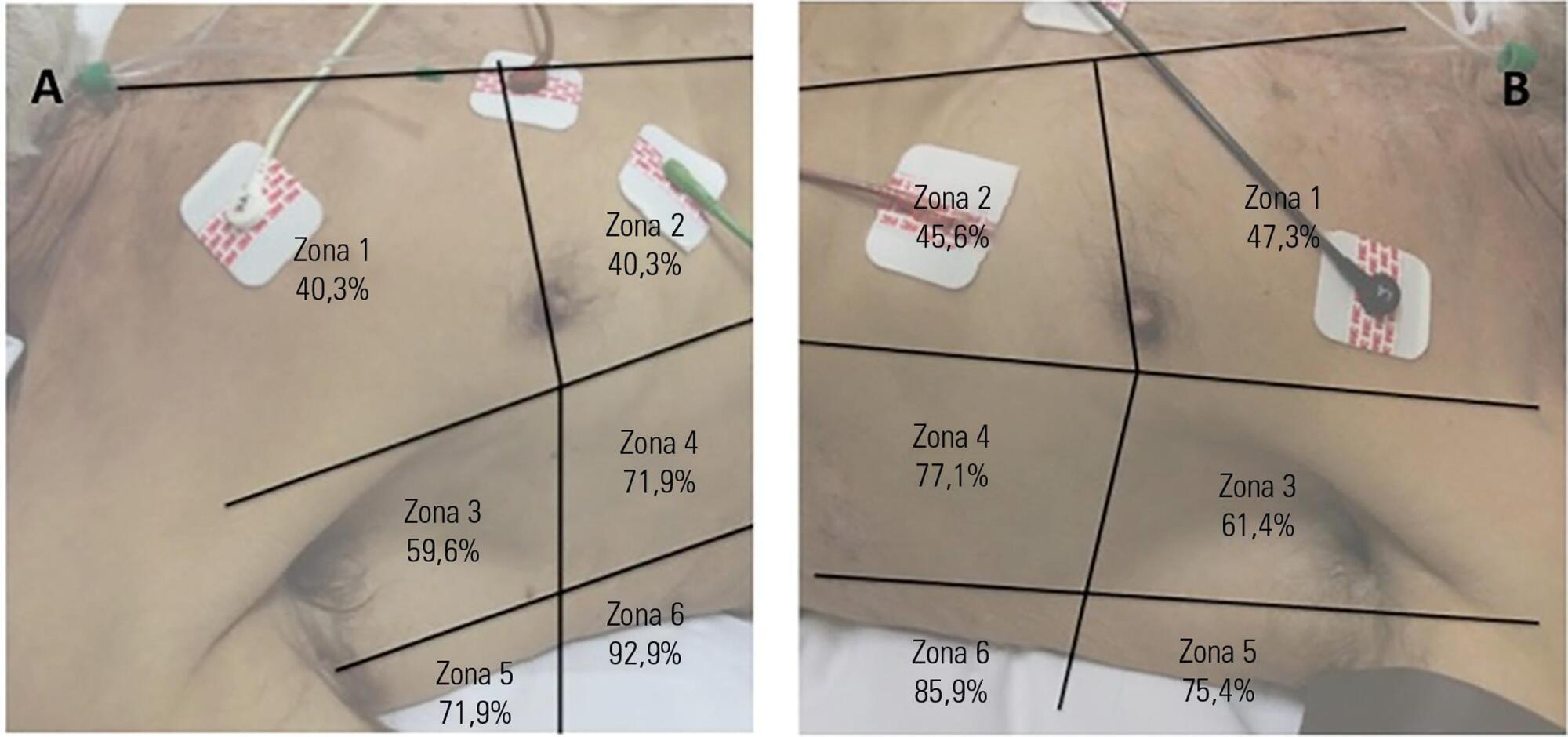
Fifty-seven subjects eligible for ventilation liberation were enrolled. Patients with tracheostomy were excluded. Lung ultrasound assessments of six thoracic zones were performed immediately before and at the exnd of the spontaneous breathing trial. B-predominance was defined as any profile with anterior bilateral B-pattern. Patients were followed up to 48 hours after extubation.
Thirty-eight individuals were successfully extubated; 11 failed the spontaneous breathing trial and 8 needed reintubation within 48 hours of extubation. At the beginning of the T-piece trial, B-pattern or consolidation was already found at the lower and posterior lung regions in more than half of the individuals and remained non-aerated at the end of the trial. A trend toward loss of lung aeration during spontaneous breathing trials was observed only in the spontaneous breathing trial-failure group (p = 0.07), and there was higher B-predominance at the end of the trial (p = 0.01).
A loss of lung aeration during the spontaneous breathing trial in non-dependent lung zones was demonstrated in subjects who failed to wean.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):278-283
DOI 10.1590/S0103-507X2012000300012
OBJECTIVE: This study analyzed acute respiratory failure caused by acute pulmonary edema, as well as chronic obstructive pulmonary disease exacerbation, that was treated with non-invasive mechanical ventilation to identify the factors that are associated with the success or failure non-invasive mechanical ventilation in urgent and emergency service. METHODS: This study was a prospective, descriptive and analytical study. We included patients of both genders aged >18 years who used non-invasive mechanical ventilation due to acute respiratory failure that was secondary to acute pulmonary edema or chronic obstructive pulmonary disease exacerbation. Patients with acute respiratory failure that was secondary to pathologies other than acute pulmonary edema and chronic obstructive pulmonary disease or who presented with contraindications for the technique were excluded. Expiratory pressures between 5 and 8 cmH2O and inspiratory pressures between 10 and 12 cmH2O were used. Supplemental oxygen maintained peripheral oxygen saturation at >90%. The primary outcome was endotracheal intubation. RESULTS: A total of 152 patients were included. The median non-invasive mechanical ventilation time was 6 hours (range 1 - 32 hours) for chronic obstructive pulmonary disease patients (n=60) and 5 hours (range 2 - 32 hours) for acute pulmonary edema patients (n=92). Most (75.7%) patients progressed successfully. However, reduced APACHE II scores and lower peripheral oxygen saturation were observed. These results were statistically significant in patients who progressed to intubation (p<0.001). BiPAP (Bi-level Positive Airway Pressure portable ventilator), as continuous positive airway pressure use increased the probability of endotracheal intubation 2.3 times (p=0.032). Patients with acute pulmonary edema and elevated GCS scores also increased the probability of success. CONCLUSION: Respiratory frequency >25 rpm, higher APACHE II scores, BiPAP use and chronic obstructive pulmonary disease diagnosis were associated with endotracheal intubation. Higher GCS and SpO2 values were associated with NIV success. Non-invasive mechanical ventilation can be used in emergency services in acute respiratory failure cases caused by acute pulmonary edema and chronic obstructive pulmonary disease exacerbation, but patients with variables related to a higher percentage of endotracheal intubation should be specially monitored.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):91-96
DOI 10.1590/S0103-507X2012000100014
Neurogenic pulmonary edema in the setting of critically ill neurologic patients is a condition that is not fully understood, and it is a relatively rare condition. Severe brain damage, such as cerebral and subarachnoid hemorrhage, head injuries and seizures, represents a risk factor for developing neurogenic pulmonary edema. Misdiagnosis and inappropriate management may worsen cerebral damage because of secondary brain injury from hypoxemia or reduced cerebral perfusion pressure. These factors may increase morbidity and mortality. This study aimed to review the current concepts on pathophysiologic mechanisms involved in the development of neurogenic pulmonary edema and discuss the associated clinical and therapeutic aspects.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)