Abstract
Crit Care Sci. 2024;36:e20240158en
DOI 10.62675/2965-2774.20240158-pt
To evaluate the association of biomarkers with successful ventilatory weaning in COVID-19 patients.
An observational, retrospective, and single-center study was conducted between March 2020 and April 2021. C-reactive protein, total lymphocytes, and the neutrophil/lymphocyte ratio were evaluated during attrition and extubation, and the variation in these biomarker values was measured. The primary outcome was successful extubation. ROC curves were drawn to find the best cutoff points for the biomarkers based on sensitivity and specificity. Statistical analysis was performed using logistic regression.
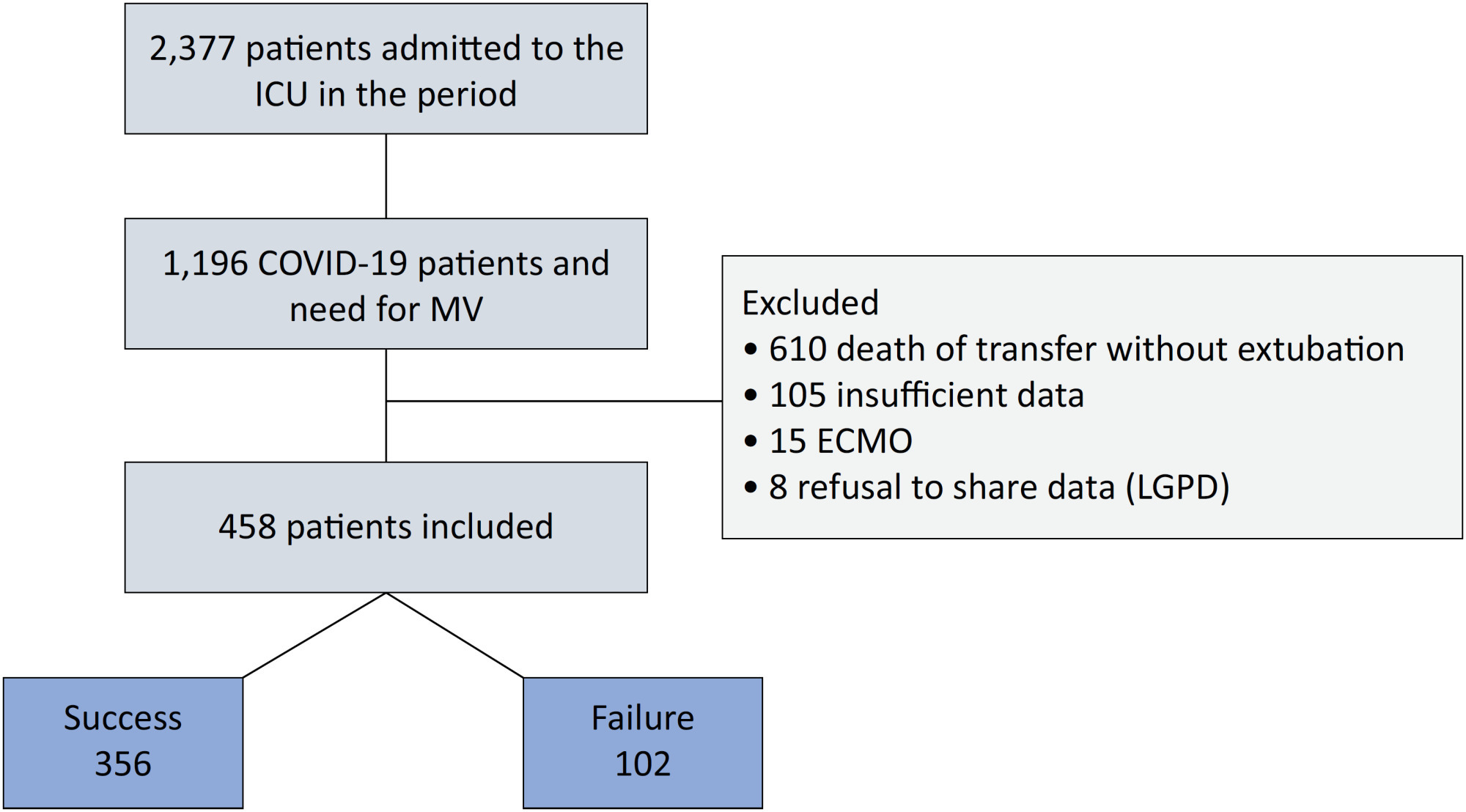
Of the 2,377 patients admitted to the intensive care unit, 458 were included in the analysis, 356 in the Successful Weaning Group and 102 in the Failure Group. The cutoff points found from the ROC curves were −62.4% for C-reactive protein, +45.7% for total lymphocytes, and −32.9% for neutrophil/lymphocyte ratio. These points were significantly associated with greater extubation success. In the multivariate analysis, only C-reactive protein variation remained statistically significant (OR 2.6; 95%CI 1.51 – 4.5; p < 0.001).
In this study, a decrease in C-reactive protein levels was associated with successful extubation in COVID-19 patients. Total lymphocytes and the neutrophil/lymphocyte ratio did not maintain the association after multivariate analysis. However, a decrease in C-reactive protein levels should not be used as a sole variable to identify COVID-19 patients suitable for weaning; as in our study, the area under the ROC curve demonstrated poor accuracy in discriminating extubation outcomes, with low sensitivity and specificity.
Abstract
Crit Care Sci. 2023;35(2):163-167
DOI 10.5935/2965-2774.20230009-pt
To assess the outcome of extubation in COVID-19 patients and the use of noninvasive ventilation in the weaning process.
This retrospective, observational, single-center study was conducted in COVID-19 patients aged 18 years or older who were admitted to an intensive care unit between April 2020 and December 2021, placed under mechanical ventilation for more than 48 hours and progressed to weaning. Early extubation was defined as extubation without a spontaneous breathing trial and immediate use of noninvasive ventilation after extubation. In patients who underwent a spontaneous breathing trial, noninvasive ventilation could be used as prophylactic ventilatory assistance when started immediately after extubation (prophylactic noninvasive ventilation) or as rescue therapy in cases of postextubation respiratory failure (therapeutic noninvasive ventilation). The primary outcome was extubation failure during the intensive care unit stay.
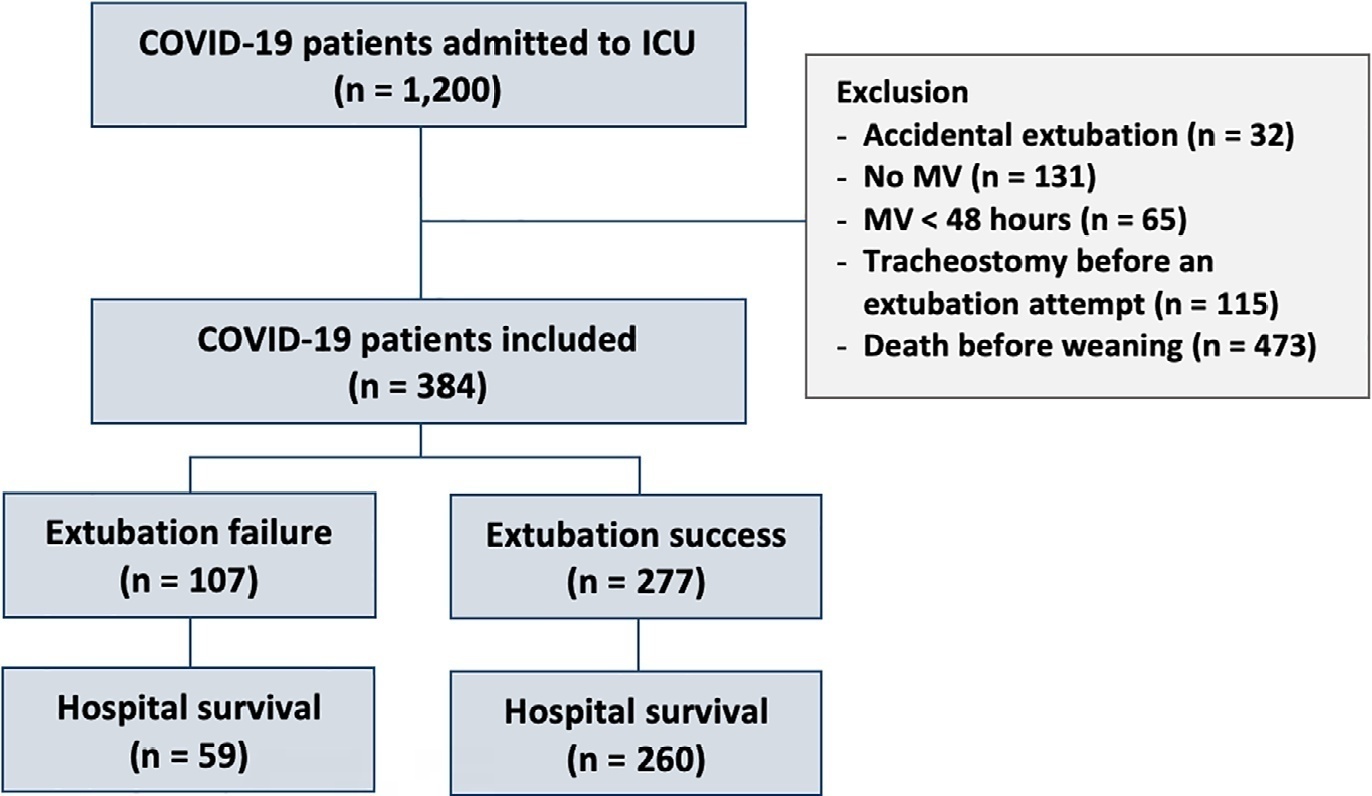
Three hundred eighty-four extubated patients were included. Extubation failure was observed in 107 (27.9%) patients. Forty-seven (12.2%) patients received prophylactic noninvasive ventilation. In 26 (6.8%) patients, early extubation was performed with immediate use of noninvasive ventilation. Noninvasive ventilation for the management of postextubation respiratory failure was administered to 64 (16.7%) patients.
We found that COVID-19 patients had a high rate of extubation failure. Despite the high risk of extubation failure, we observed low use of prophylactic noninvasive ventilation in these patients.
Abstract
Crit Care Sci. 2023;35(2):168-176
DOI 10.5935/2965-2774.20230410-pt
We hypothesized that the use of mechanical insufflation-exsufflation can reduce the incidence of acute respiratory failure within the 48-hour post-extubation period in intensive care unit-acquired weakness patients.
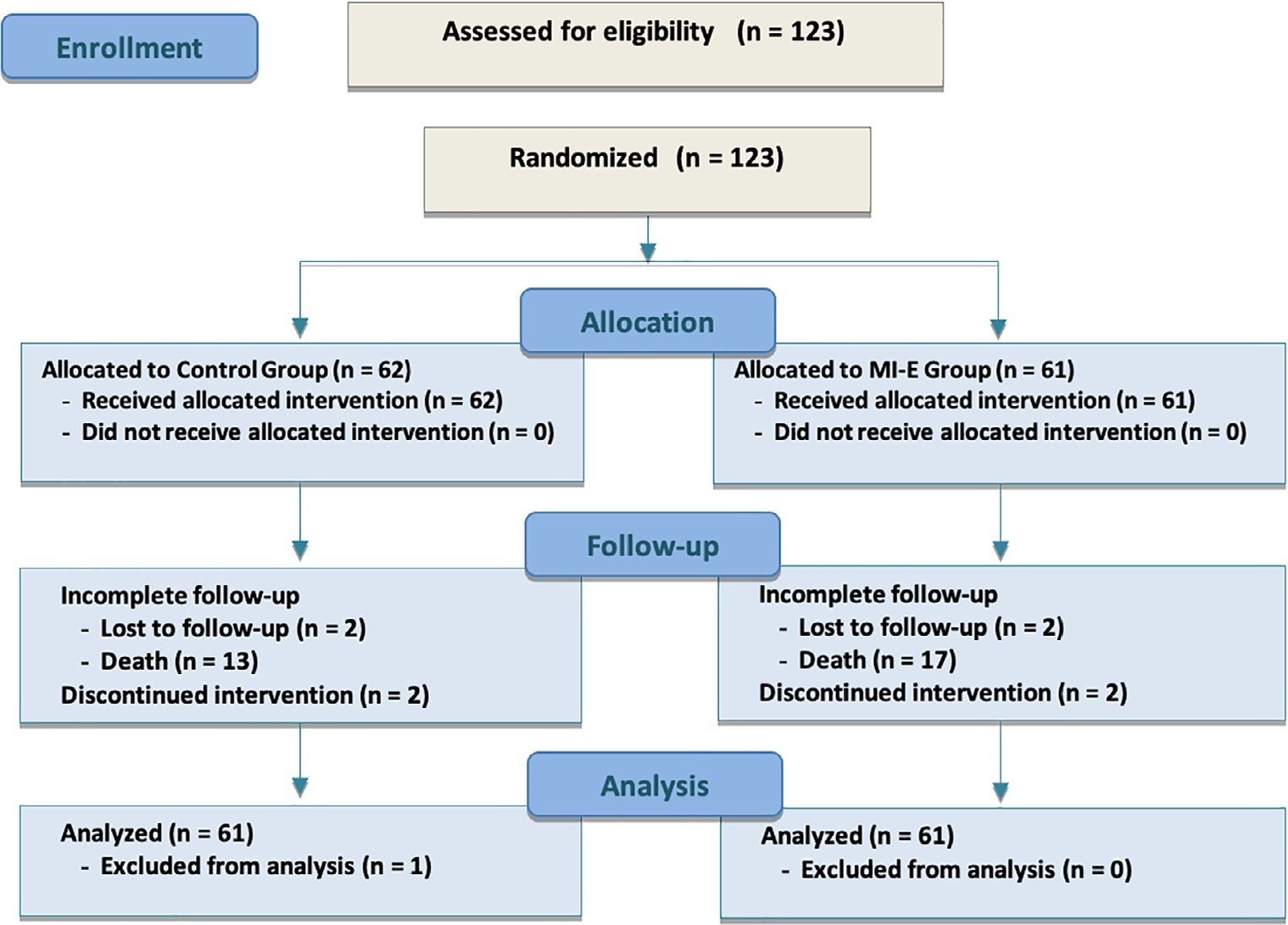
This was a prospective randomized controlled open-label trial. Patients diagnosed with intensive care unit-acquired weakness were consecutively enrolled based on a Medical Research Council score ≤ 48/60. The patients randomly received two daily sessions; in the control group, conventional chest physiotherapy was performed, while in the intervention group, chest physiotherapy was associated with mechanical insufflation-exsufflation. The incidence of acute respiratory failure within 48 hours of extubation was evaluated. Similarly, the reintubation rate, intensive care unit length of stay, mortality at 28 days, and survival probability at 90 days were assessed. The study was stopped after futility results in the interim analysis.
We included 122 consecutive patients (n = 61 per group). There was no significant difference in the incidence of acute respiratory failure between treatments (11.5% control group versus 16.4%, intervention group; p = 0.60), the need for reintubation (3.6% versus 10.7%; p = 0.27), mean length of stay (3 versus 4 days; p = 0.33), mortality at Day 28 (9.8% versus 15.0%; p = 0.42), or survival probability at Day 90 (21.3% versus 28.3%; p = 0.41).
Mechanical insufflation-exsufflation combined with chest physiotherapy seems to have no impact in preventing postextubation acute respiratory failure in intensive care unit-acquired weakness patients. Similarly, mortality and survival probability were similar in both groups. Nevertheless, given the early termination of the trial, further clinical investigation is strongly recommended.
Abstract
Crit Care Sci. 2023;35(1):44-56
DOI 10.5935/2965-2774.20230340-pt
To investigate whether protocol-directed weaning in neurocritical patients would reduce the rate of extubation failure (as a primary outcome) and the associated complications (as a secondary outcome) compared with conventional weaning.
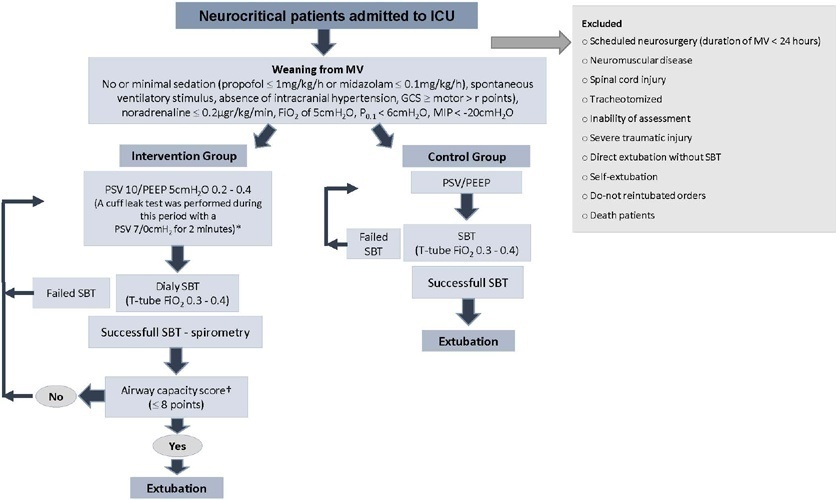
A quasi-experimental study was conducted in a medical-surgical intensive care unit from January 2016 to December 2018. Patients aged 18 years or older with an acute neurological disease who were on mechanical ventilation > 24 hours were included. All patients included in the study were ready to wean, with no or minimal sedation, Glasgow coma score ≥ 9, spontaneous ventilatory stimulus, noradrenaline ≤ 0.2μgr/kg/ minute, fraction of inspired oxygen ≤ 0.5, positive end-expiratory pressure ≤ 5cmH2O, maximal inspiratory pressure < -20cmH2O, and occlusion pressure < 6cmH2O.
Ninety-four of 314 patients admitted to the intensive care unit were included (50 in the Intervention Group and 44 in the Control Group). There was no significant difference in spontaneous breathing trial failure (18% in the Intervention Group versus 34% in the Control Group, p = 0.12). More patients in the Intervention Group were extubated than in the Control Group (100% versus 79%, p = 0.01). The rate of extubation failure was not signifiantly diffrent between the groups (18% in the Intervention Group versus 17% in the Control Group; relative risk 1.02; 95%CI 0.64 - 1.61; p = 1.00). The reintubation rate was lower in the Control Group (16% in the Intervention Group versus 11% in the Control Group; relative risk 1.15; 95%CI 0.74 - 1.82; p = 0.75). The need for tracheotomy was lower in the Intervention Group [4 (8%) versus 11 (25%) in the Control Group; relative risk 0.32; 95%CI 0.11 - 0.93; p = 0.04]. At Day 28, the patients in the Intervention Group had more ventilator-free days than those in the Control Group [28 (26 - 28) days versus 26 (19 - 28) days; p = 0.01]. The total duration of mechanical ventilation was shorter in the Intervention Group than in the Control Group [5 (2 - 13) days versus 9 (3 - 22) days; p = 0.01]. There were no diffrences in the length of intensive care unit stay, 28-day free from mechanical ventilation, hospital stay or 90-day mortality.
Considering the limitations of our study, the application of a weaning protocol for neurocritical patients led to a high percentage of extubation, a reduced need for tracheotomy and a shortened duration of mechanical ventilation. However, there was no reduction in extubation failure or the 28-day free of from mechanical ventilation compared with the Control Group.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):452-460
DOI 10.5935/0103-507X.20220087-en
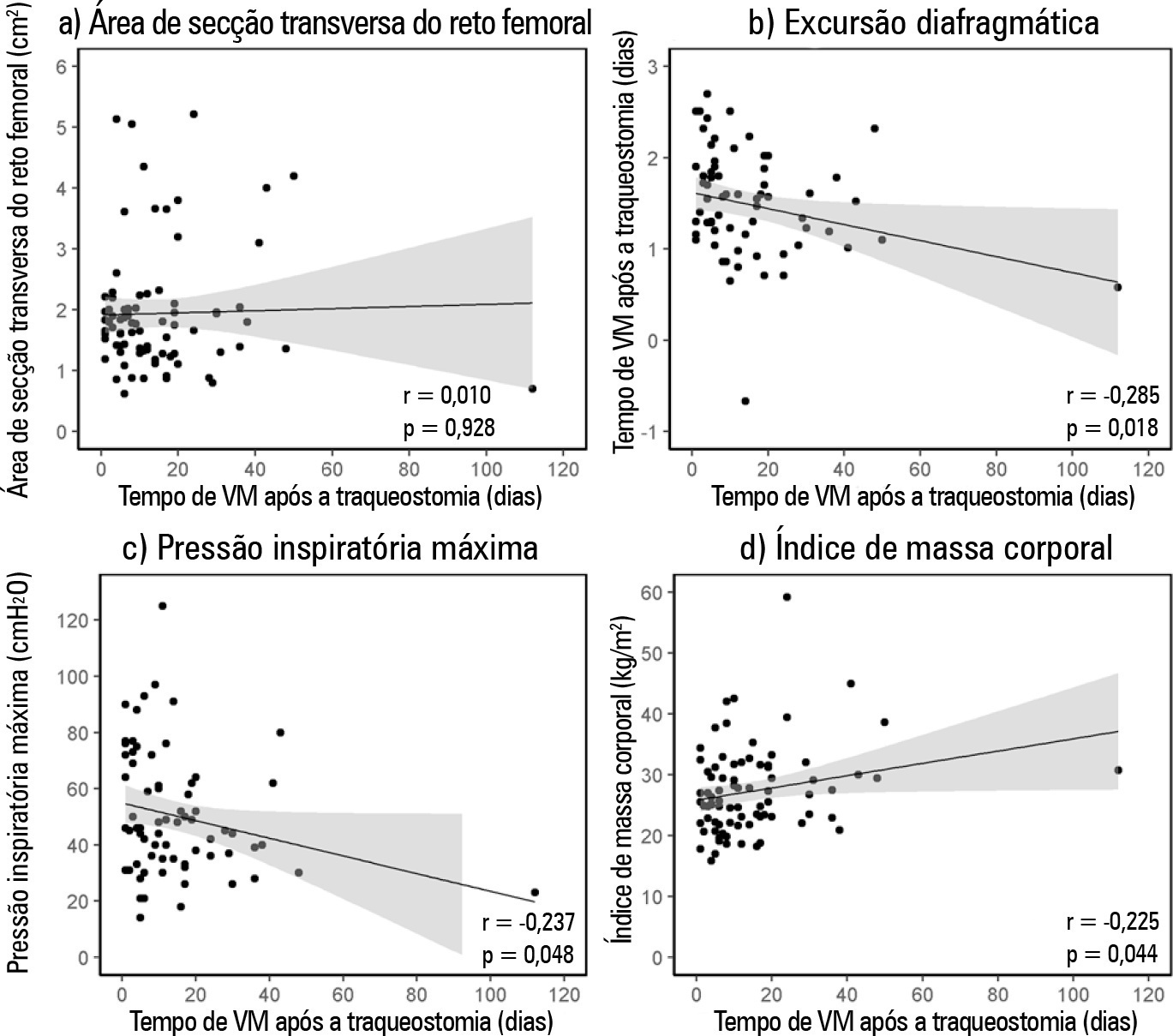
To verify the relationship between the rectus femoris cross-sectional area and diaphragmatic excursion with successful weaning from mechanical ventilation in chronic critically tracheostomized patients.
This was a prospective observational cohort study. We included chronic critically ill patients (those who underwent tracheostomy placement after 10 days under mechanical ventilation). The rectus femoris cross-sectional area and diaphragmatic excursion were obtained by ultrasonography performed within the first 48 hours after tracheostomy. We measured rectus femoris cross-sectional area and diaphragmatic excursion to assess their association with weaning from mechanical ventilation, including their potential to predict successful weaning and survival throughout the intensive care unit stay.
Eighty-one patients were included. Forty-five patients (55%) were weaned from mechanical ventilation. The mortality rates were 42% and 61.7% in the intensive care unit and hospital, respectively. The fail group in relation to the success group at weaning presented a lower rectus femoris cross-sectional area (1.4 [0.8] versus 1.84 [0.76]cm2, p = 0.014) and lower diaphragmatic excursion (1.29 ± 0.62 versus 1.62 ± 0.51cm, p = 0.019). When rectus femoris cross-sectional area ≥ 1.80cm2 and diaphragmatic excursion ≥ 1.25cm was a combined condition, it had a strong association with successful weaning (adjusted OR = 20.81, 95%CI 2.38 - 182.28; p = 0.006) but not with intensive care unit survival (adjusted OR = 0.19, 95%CI 0.03 - 1.08; p = 0.061).
Successful weaning from mechanical ventilation in chronic critically ill patients was associated with higher measurements of rectus femoris cross-sectional area and diaphragmatic excursion.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):445-456
DOI 10.5935/0103-507X.20210060
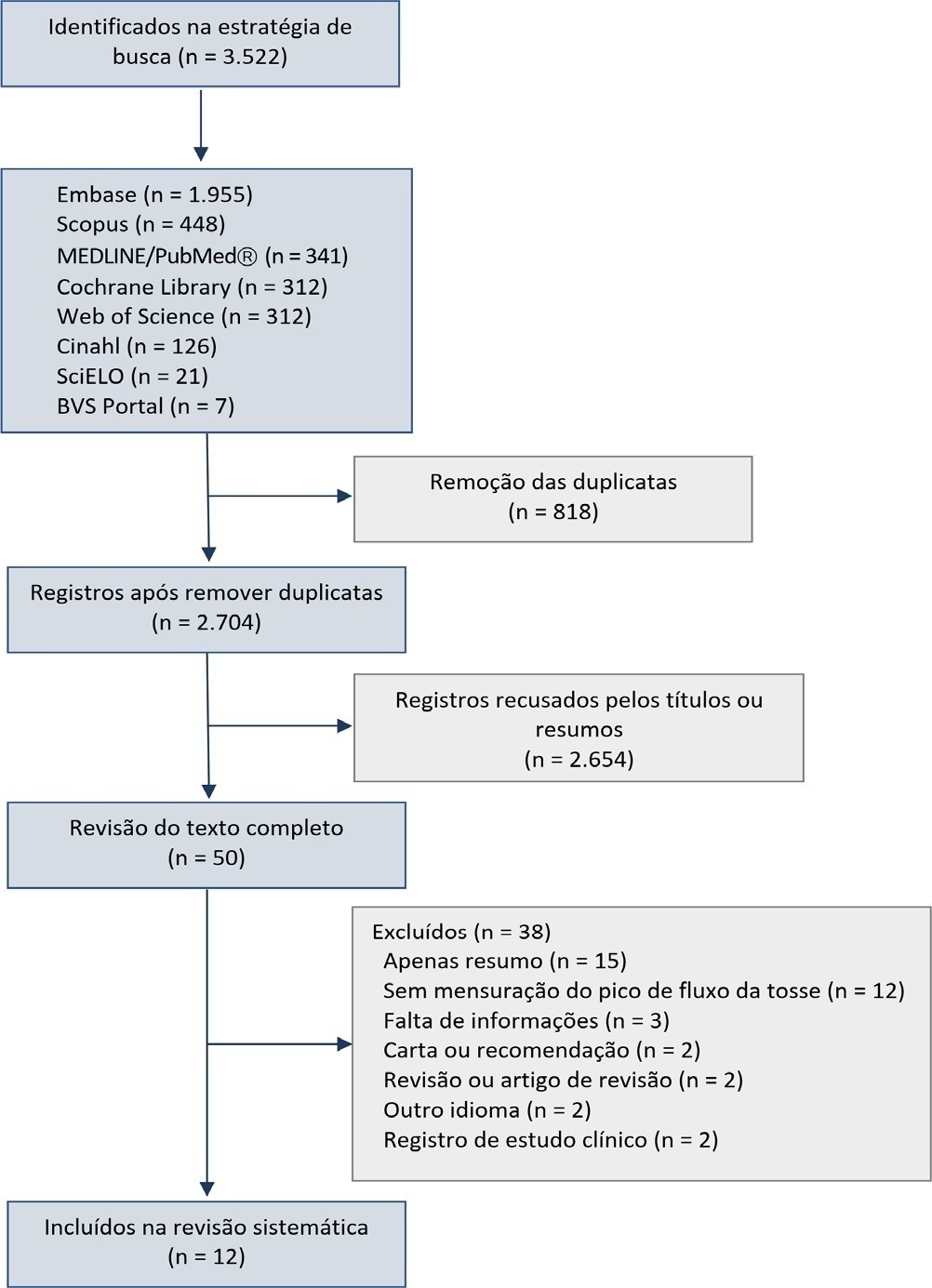
This systematic review was designed to assess the usefulness of cough peak flow to predict the extubation outcome in subjects who passed a spontaneous breathing trial.
The search covered the scientific databases MEDLINE, Lilacs, Ibecs, Cinahl, SciELO, Cochrane, Scopus, Web of Science and gray literature. The Quality Assessment of Diagnostic Accuracy Studies was used to assess the methodological quality and risk of study bias. The statistical heterogeneity of the likelihood (LR) and diagnostic odds ratios were evaluated using forest plots and Cochran’s Q statistic, and a crosshair summary Receiver Operating Characteristic plot using the multiple cutoffs model was calculated.
We initially retrieved 3,522 references from the databases; among these, 12 studies including 1,757 subjects were selected for the qualitative analysis. Many studies presented an unclear risk of bias in the “patient selection” and “flow and time” criteria. Among the 12 included studies, seven presented “high risk” and five “unclear risk” for the item “reference standard.” The diagnostic performance of the cough peak flow for the extubation outcome was low to moderate when we considered the results from all included studies, with a +LR of 1.360 (95%CI 1.240 - 1.530), -LR of 0.218 (95%CI 0.159 - 0.293) and a diagnostic odds ratio of 6.450 (95%CI 4.490 - 9.090). A subgroup analysis including only the studies with a cutoff between 55 and 65 L/minute showed a slightly better, although still moderate, performance.
A cough peak flow assessment considering a cutoff between 55 and 65L/minute may be useful as a complementary measurement prior to extubation. Additional well-designed studies are necessary to identify the best method and equipment to record the cough peak flow as well as the best cutoff.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):279-286
DOI 10.5935/0103-507X.20170038
We aimed to investigate a potential association between B-lines and weaning failure.
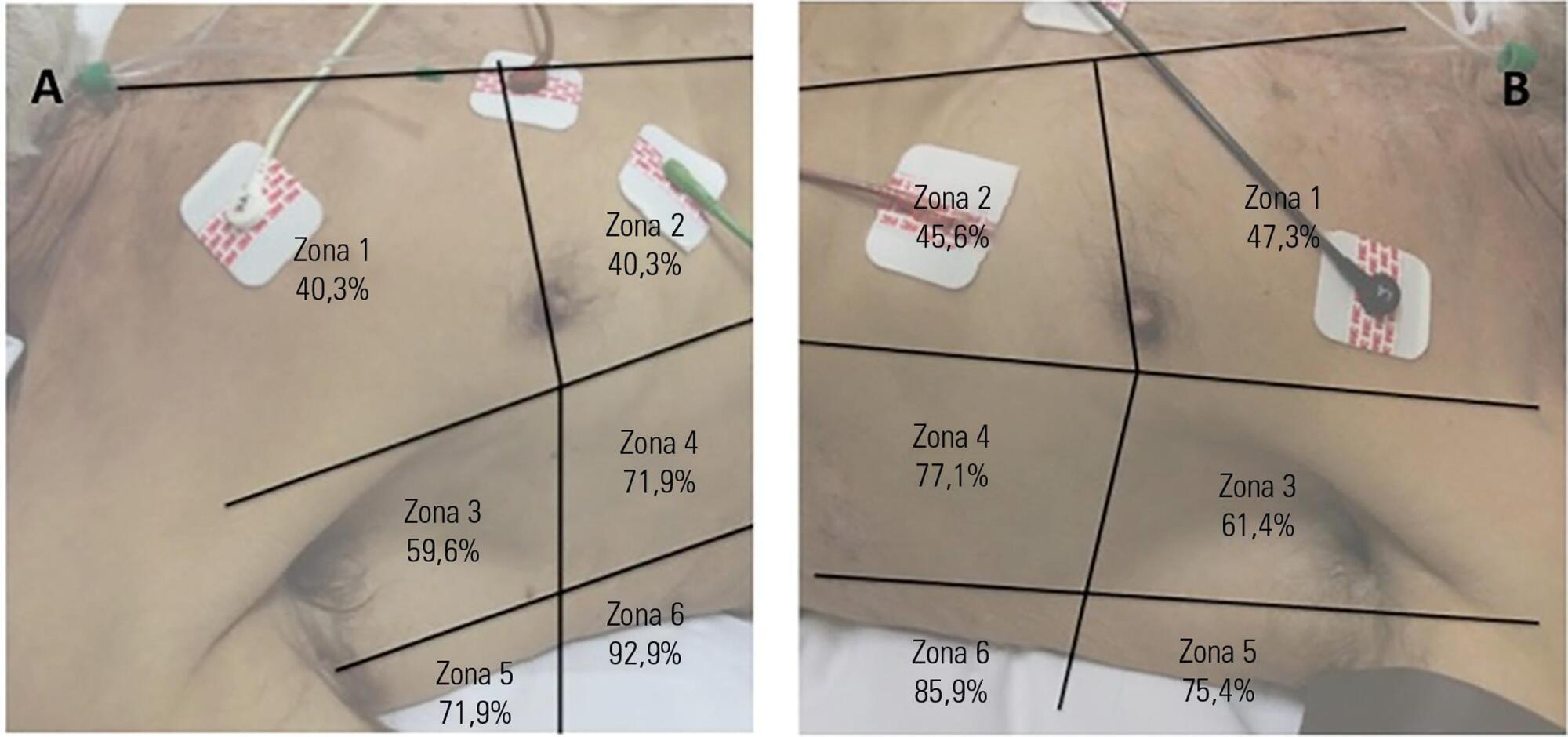
Fifty-seven subjects eligible for ventilation liberation were enrolled. Patients with tracheostomy were excluded. Lung ultrasound assessments of six thoracic zones were performed immediately before and at the exnd of the spontaneous breathing trial. B-predominance was defined as any profile with anterior bilateral B-pattern. Patients were followed up to 48 hours after extubation.
Thirty-eight individuals were successfully extubated; 11 failed the spontaneous breathing trial and 8 needed reintubation within 48 hours of extubation. At the beginning of the T-piece trial, B-pattern or consolidation was already found at the lower and posterior lung regions in more than half of the individuals and remained non-aerated at the end of the trial. A trend toward loss of lung aeration during spontaneous breathing trials was observed only in the spontaneous breathing trial-failure group (p = 0.07), and there was higher B-predominance at the end of the trial (p = 0.01).
A loss of lung aeration during the spontaneous breathing trial in non-dependent lung zones was demonstrated in subjects who failed to wean.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):213-221
DOI 10.5935/0103-507X.20170030
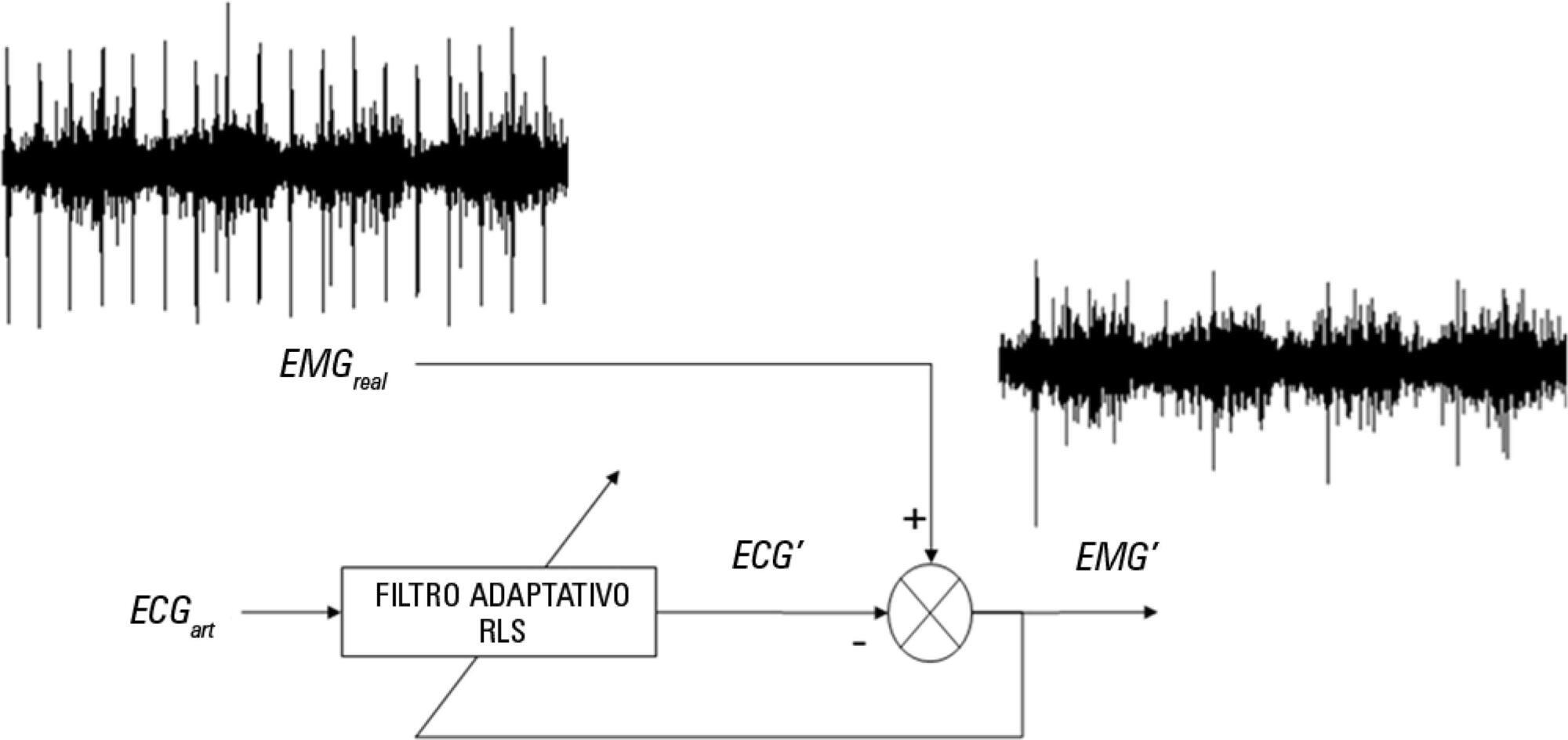
The aim of this pilot study was to evaluate the feasibility of surface electromyographic signal derived indexes for the prediction of weaning outcomes among mechanically ventilated subjects after cardiac surgery.
A sample of 10 postsurgical adult subjects who received cardiovascular surgery that did not meet the criteria for early extubation were included. Surface electromyographic signals from diaphragm and ventilatory variables were recorded during the weaning process, with the moment determined by the medical staff according to their expertise. Several indexes of respiratory muscle expenditure from surface electromyography using linear and non-linear processing techniques were evaluated. Two groups were compared: successfully and unsuccessfully weaned patients.
The obtained indexes allow estimation of the diaphragm activity of each subject, showing a correlation between high expenditure and weaning test failure.
Surface electromyography is becoming a promising procedure for assessing the state of mechanically ventilated patients, even in complex situations such as those that involve a patient after cardiovascular surgery.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98) Septic shock (25)