Abstract
Crit Care Sci. 2023;35(2):168-176
DOI 10.5935/2965-2774.20230410-pt
We hypothesized that the use of mechanical insufflation-exsufflation can reduce the incidence of acute respiratory failure within the 48-hour post-extubation period in intensive care unit-acquired weakness patients.
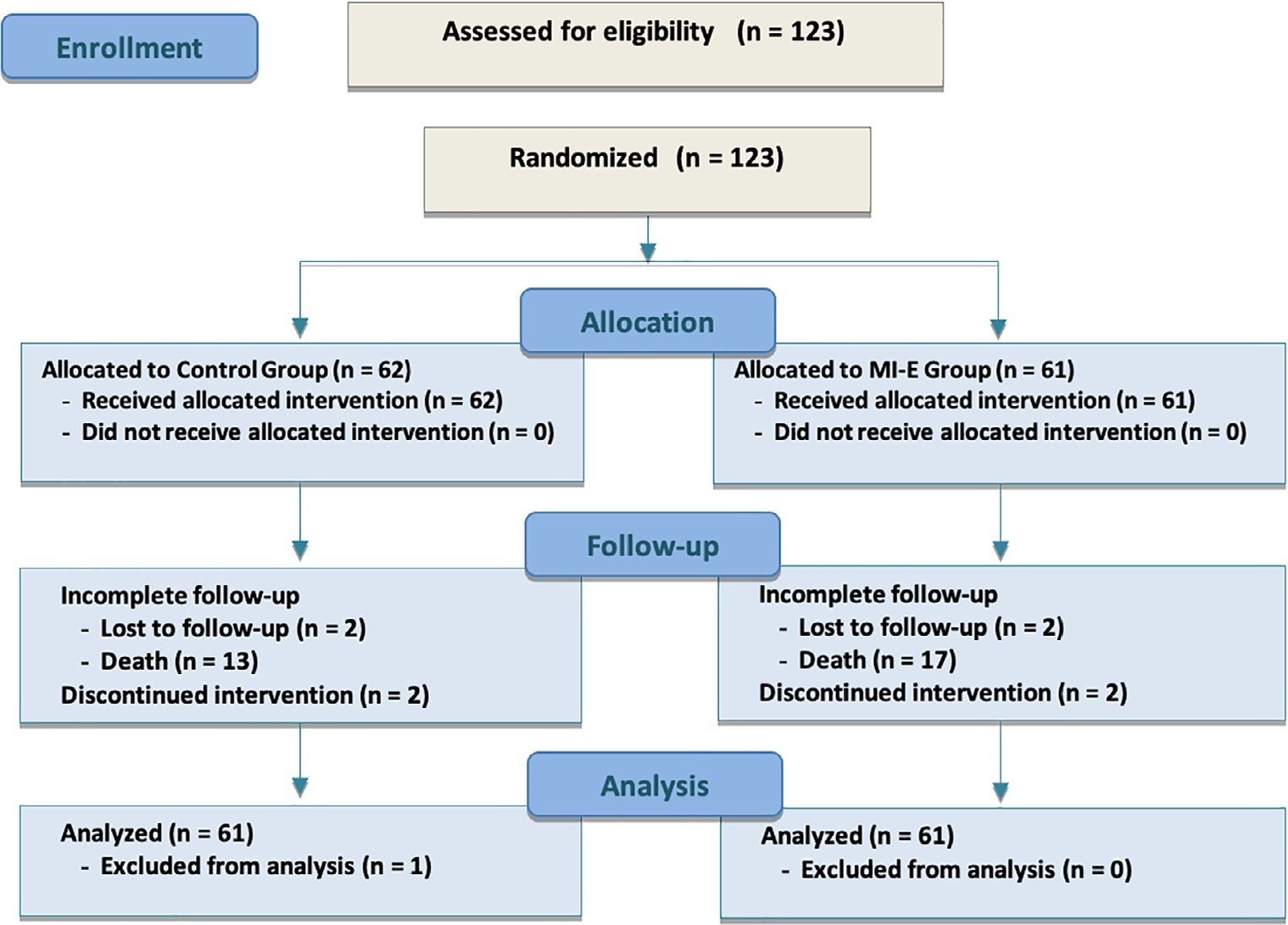
This was a prospective randomized controlled open-label trial. Patients diagnosed with intensive care unit-acquired weakness were consecutively enrolled based on a Medical Research Council score ≤ 48/60. The patients randomly received two daily sessions; in the control group, conventional chest physiotherapy was performed, while in the intervention group, chest physiotherapy was associated with mechanical insufflation-exsufflation. The incidence of acute respiratory failure within 48 hours of extubation was evaluated. Similarly, the reintubation rate, intensive care unit length of stay, mortality at 28 days, and survival probability at 90 days were assessed. The study was stopped after futility results in the interim analysis.
We included 122 consecutive patients (n = 61 per group). There was no significant difference in the incidence of acute respiratory failure between treatments (11.5% control group versus 16.4%, intervention group; p = 0.60), the need for reintubation (3.6% versus 10.7%; p = 0.27), mean length of stay (3 versus 4 days; p = 0.33), mortality at Day 28 (9.8% versus 15.0%; p = 0.42), or survival probability at Day 90 (21.3% versus 28.3%; p = 0.41).
Mechanical insufflation-exsufflation combined with chest physiotherapy seems to have no impact in preventing postextubation acute respiratory failure in intensive care unit-acquired weakness patients. Similarly, mortality and survival probability were similar in both groups. Nevertheless, given the early termination of the trial, further clinical investigation is strongly recommended.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):362-373
DOI 10.5935/0103-507X.20210059
To determine the effectiveness of noninvasive ventilation versus conventional oxygen therapy in patients with acute respiratory failure after extubation failure.
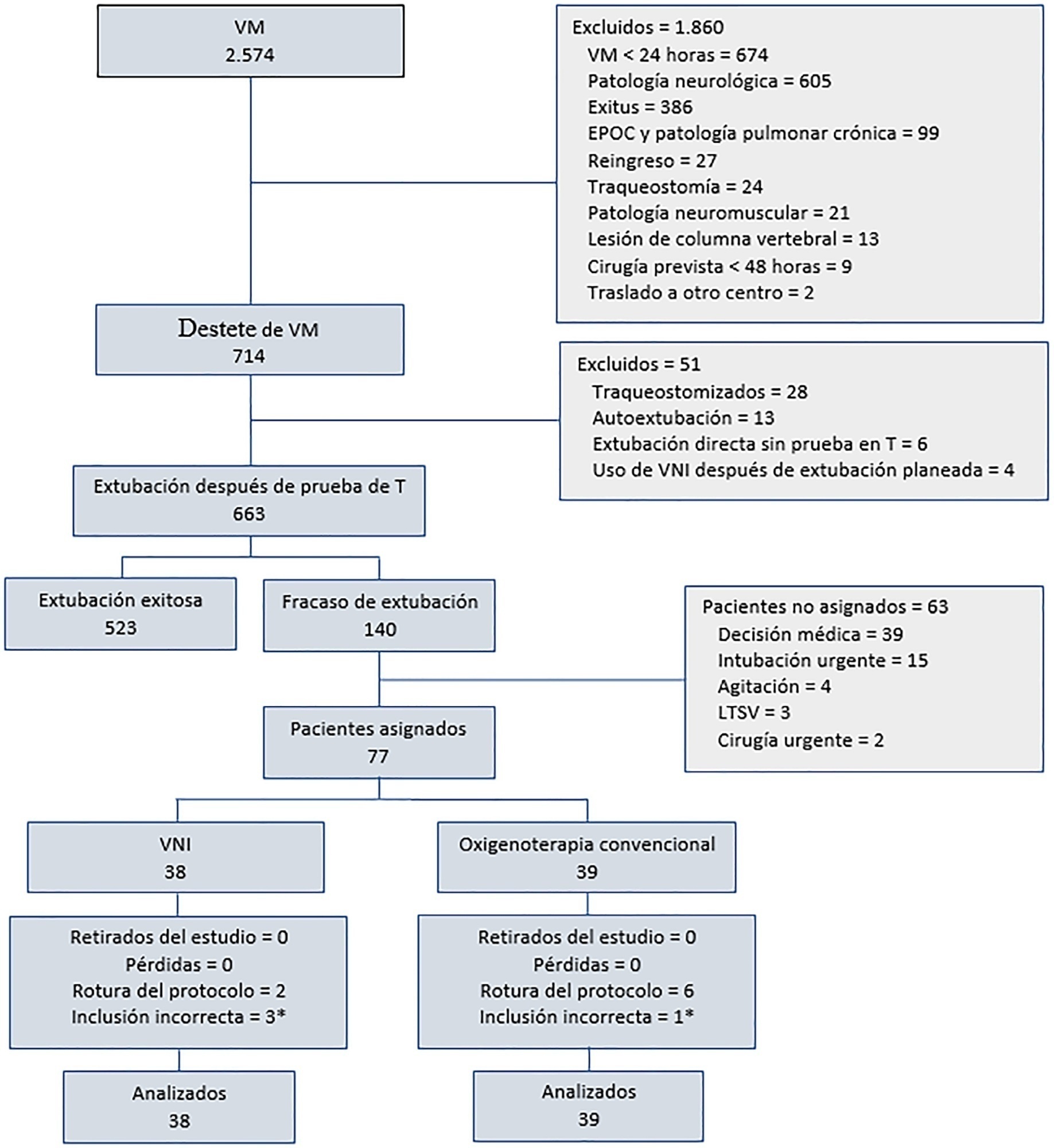
A pragmatic clinical trial was conducted in an intensive care unit from March 2009 to September 2016. Patients on mechanical ventilation > 24 hours who developed acute respiratory failure after scheduled extubation were included and were assigned to noninvasive ventilation or conventional oxygen therapy. The primary objective was to reduce the reintubation rate. The secondary objectives were to improve respiratory parameters and reduce complications, the duration of mechanical ventilation, the intensive care unit stay, the hospital stay, and mortality in the intensive care unit, in the hospital, and 90 days after discharge. Factors correlated with reintubation were also analyzed.
Of a total of 2,574 patients, 77 were analyzed (38 in the noninvasive ventilation group and 39 in the conventional oxygen therapy group). Noninvasive ventilation reduced the respiratory and cardiac rates more rapidly than conventional oxygen therapy. Reintubation was less common in the noninvasive ventilation group [12 (32%) versus 22 (56%) in the conventional oxygen therapy group, relative risk 0.58 (95%CI 0.34 - 0.97), p = 0.039]. The rest of the parameters did not show significant differences. In the multivariate analysis, noninvasive ventilation protected against reintubation [OR 0.17 (95%CI 0.05 - 0.56), p = 0.004], while liver failure before extubation and the inability to maintain airway patency predisposed patients to reintubation.
The use of noninvasive ventilation in patients who failed extubation could be beneficial compared to conventional oxygen therapy.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):422-427
DOI 10.5935/0103-507X.20210057
To assess whether there is an association between 48-hour postextubation fluid balance and extubation failure.
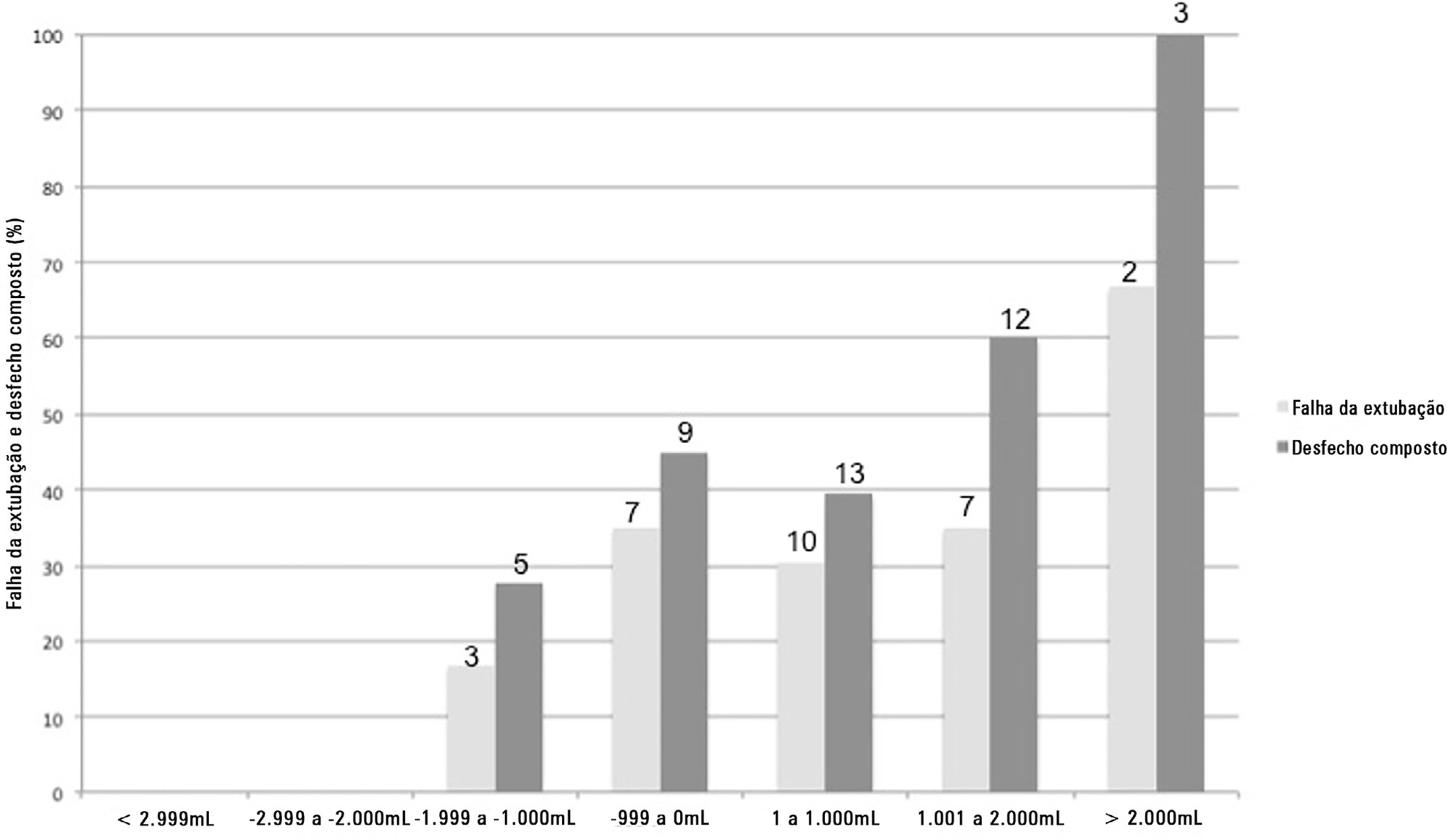
This was a prospective cohort study that included patients admitted to the intensive care unit of a tertiary hospital in southern Brazil from March 2019 to December 2019. Patients who required mechanical ventilation for at least 24 hours and who were extubated during the study period were included. The primary outcome was extubation failure, considered as the need for reintubation in the first 72 hours after extubation. The secondary outcome was a combined outcome with extubation failure or the need for therapeutic noninvasive ventilation.
A total of 101 patients were included. Extubation failure was observed in 29 (28.7%) patients. In univariate analysis, patients with a negative 48-hour postextubation fluid balance higher than one liter had a lower rate of extubation failure (12.0%) than patients with a negative 48-hour postextubation fluid balance lower than 1L (34.2%; p = 0.033). Mechanical ventilation duration and negative 48-hour postextubation fluid balance lower than one liter were associated with extubation failure when corrected for Simplified Acute Physiology Score 3 in multivariate analysis. When we evaluated the combined outcome, only negative 48-hour postextubation lower than 1L maintained an association when corrected for for Simplified Acute Physiology Score 3 and mechanical ventilation duration.
The 48-hour postextubation fluid balance is associated with extubation failure. Further studies are necessary to assess whether avoiding positive fluid balance in this period might improve weaning outcomes.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):445-456
DOI 10.5935/0103-507X.20210060
This systematic review was designed to assess the usefulness of cough peak flow to predict the extubation outcome in subjects who passed a spontaneous breathing trial.
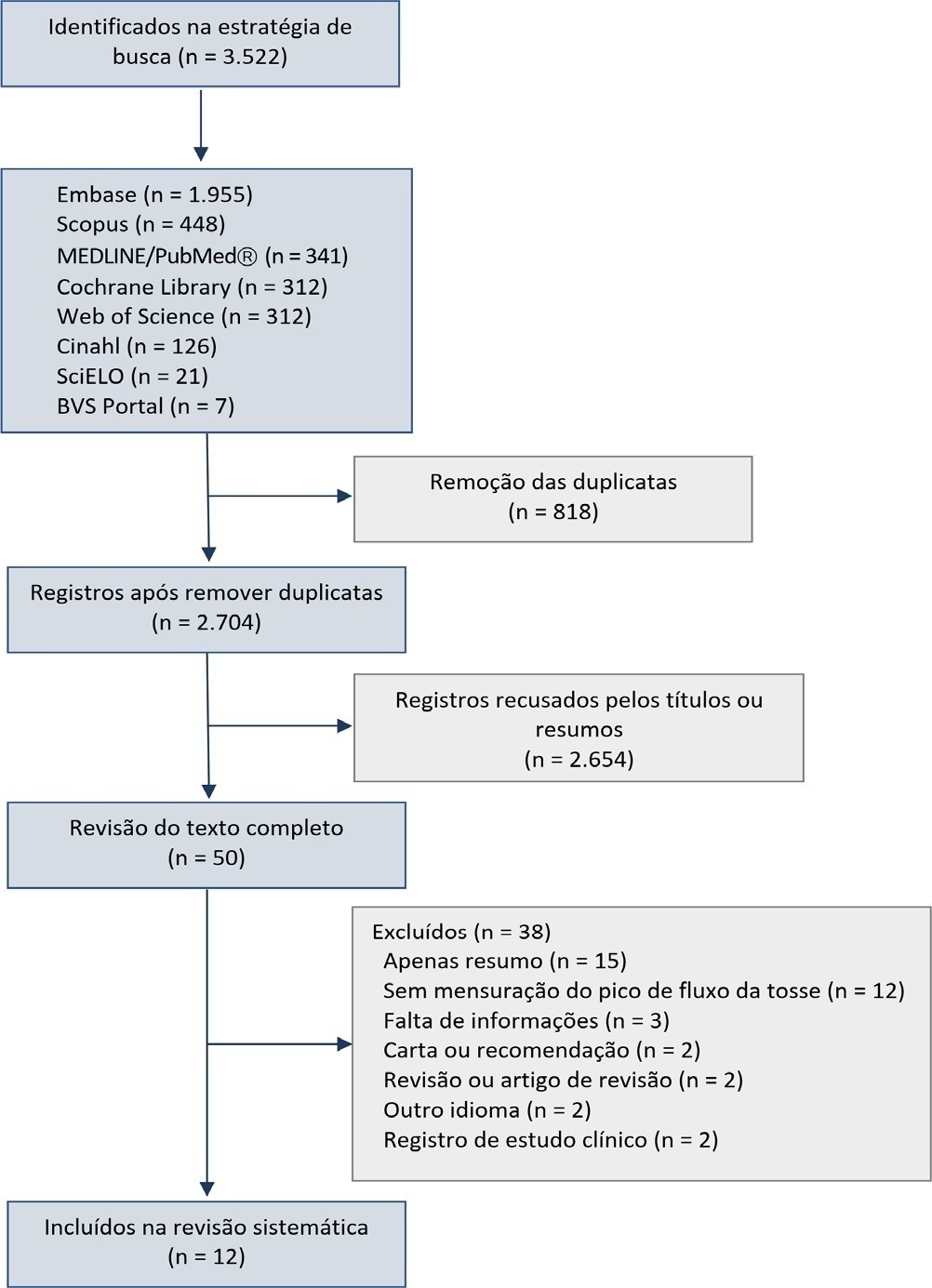
The search covered the scientific databases MEDLINE, Lilacs, Ibecs, Cinahl, SciELO, Cochrane, Scopus, Web of Science and gray literature. The Quality Assessment of Diagnostic Accuracy Studies was used to assess the methodological quality and risk of study bias. The statistical heterogeneity of the likelihood (LR) and diagnostic odds ratios were evaluated using forest plots and Cochran’s Q statistic, and a crosshair summary Receiver Operating Characteristic plot using the multiple cutoffs model was calculated.
We initially retrieved 3,522 references from the databases; among these, 12 studies including 1,757 subjects were selected for the qualitative analysis. Many studies presented an unclear risk of bias in the “patient selection” and “flow and time” criteria. Among the 12 included studies, seven presented “high risk” and five “unclear risk” for the item “reference standard.” The diagnostic performance of the cough peak flow for the extubation outcome was low to moderate when we considered the results from all included studies, with a +LR of 1.360 (95%CI 1.240 - 1.530), -LR of 0.218 (95%CI 0.159 - 0.293) and a diagnostic odds ratio of 6.450 (95%CI 4.490 - 9.090). A subgroup analysis including only the studies with a cutoff between 55 and 65 L/minute showed a slightly better, although still moderate, performance.
A cough peak flow assessment considering a cutoff between 55 and 65L/minute may be useful as a complementary measurement prior to extubation. Additional well-designed studies are necessary to identify the best method and equipment to record the cough peak flow as well as the best cutoff.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):23-33
DOI 10.5935/0103-507X.20170005
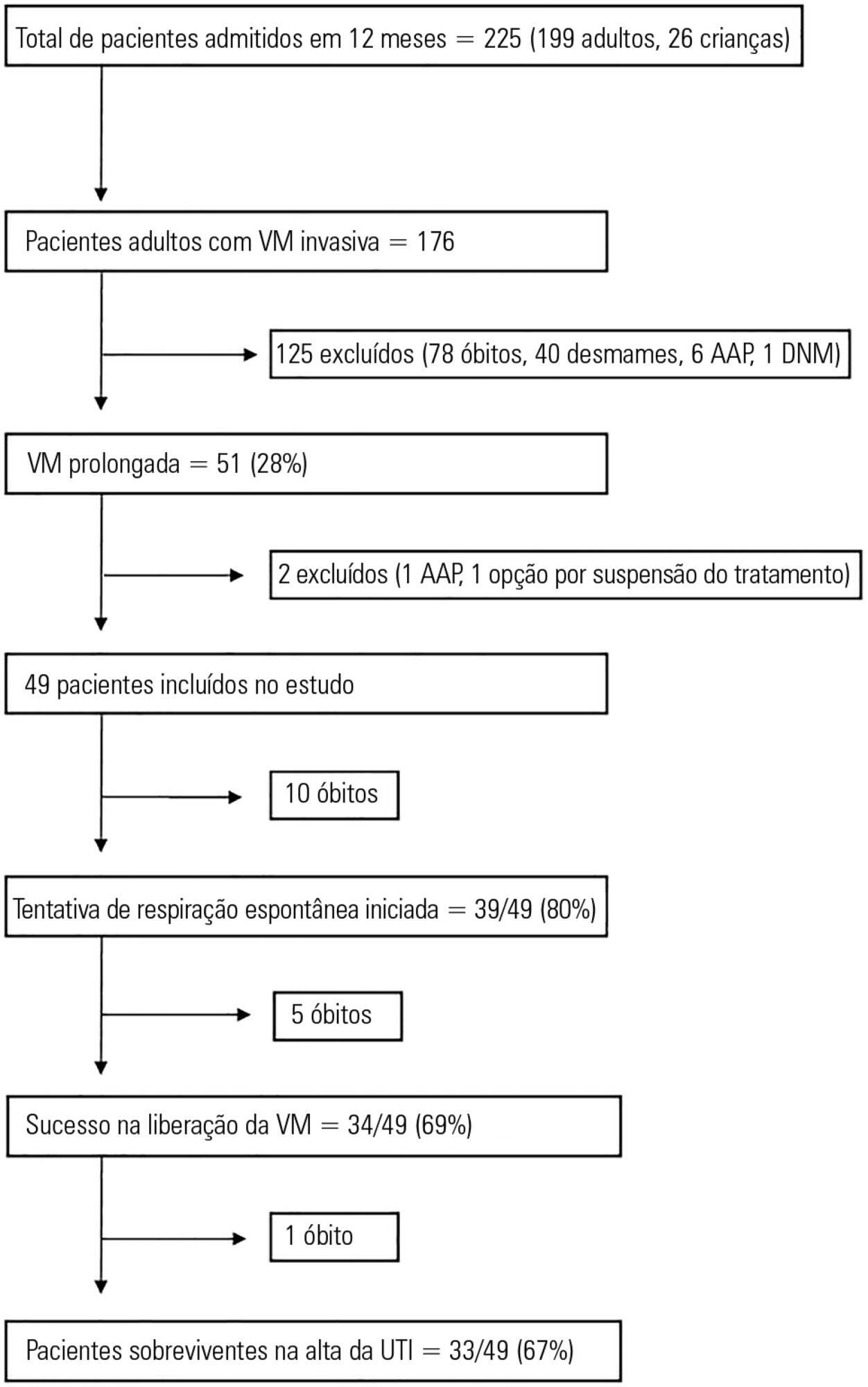
This study aimed to examine the clinical characteristics, weaning pattern, and outcome of patients requiring prolonged mechanical ventilation in acute intensive care unit settings in a resource-limited country.
This was a prospective single-center observational study in India, where all adult patients requiring prolonged ventilation were followed for weaning duration and pattern and for survival at both intensive care unit discharge and at 12 months. The definition of prolonged mechanical ventilation used was that of the National Association for Medical Direction of Respiratory Care.
During the one-year period, 49 patients with a mean age of 49.7 years had prolonged ventilation; 63% were male, and 84% had a medical illness. The median APACHE II and SOFA scores on admission were 17 and 9, respectively. The median number of ventilation days was 37. The most common reason for starting ventilation was respiratory failure secondary to sepsis (67%). Weaning was initiated in 39 (79.5%) patients, with success in 34 (87%). The median weaning duration was 14 (9.5 - 19) days, and the median length of intensive care unit stay was 39 (32 - 58.5) days. Duration of vasopressor support and need for hemodialysis were significant independent predictors of unsuccessful ventilator liberation. At the 12-month follow-up, 65% had survived.
In acute intensive care units, more than one-fourth of patients with invasive ventilation required prolonged ventilation. Successful weaning was achieved in two-thirds of patients, and most survived at the 12-month follow-up.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):137-142
DOI 10.5935/0103-507X.20140020
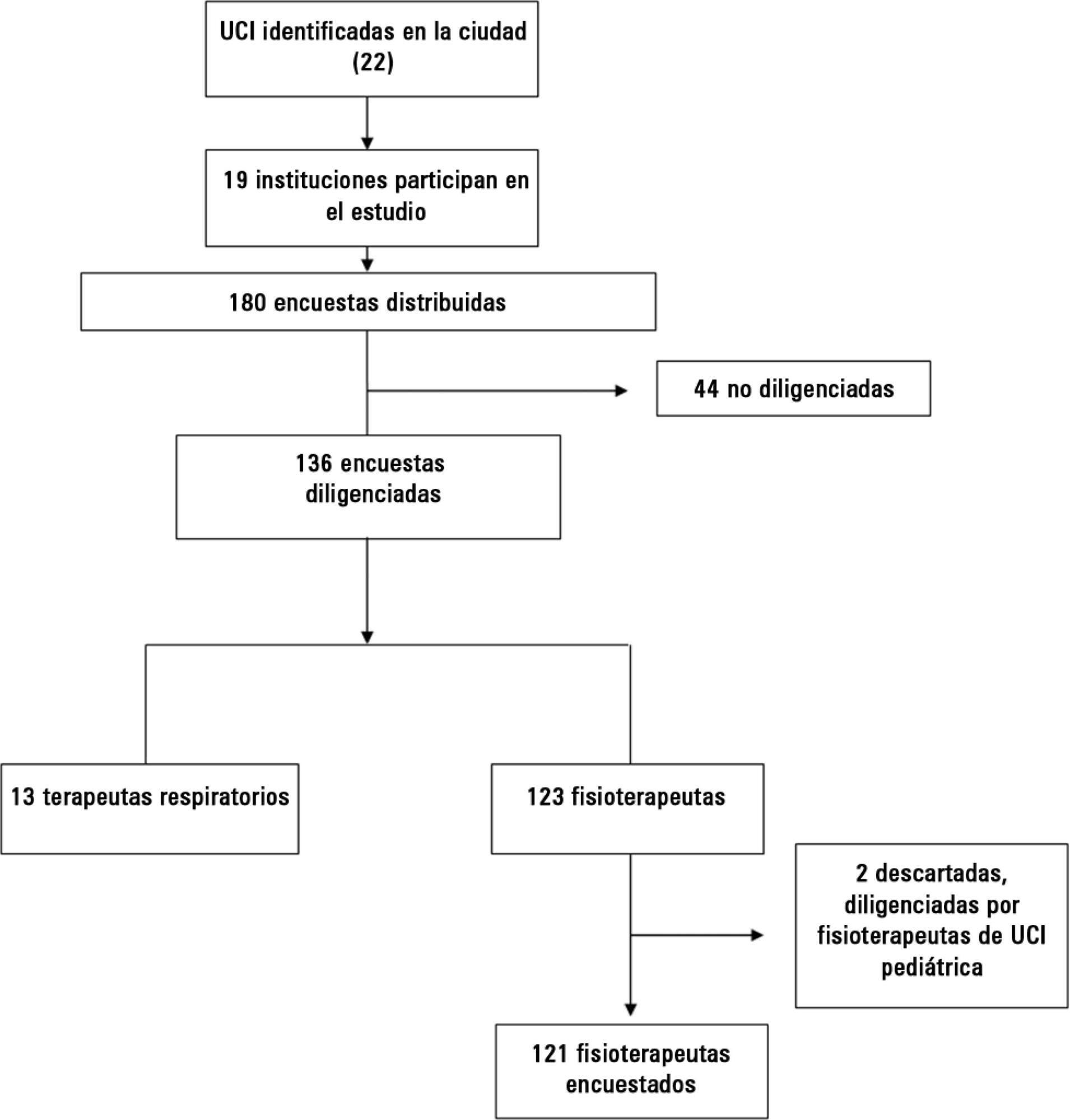
Early weaning from mechanical ventilation is one of the primary goals in managing critically ill patients. There are various techniques and measurement parameters for such weaning. The objective of this study was to describe the practices of ventilatory weaning in adult intensive care units in the city of Cali.
A survey of 32 questions (some multiple choice) evaluating weaning practices was distributed to physiotherapists and respiratory therapists working in intensive care units, to be answered anonymously.
The most common strategy for the parameter set was the combination of continuous positive airway pressure with pressure support (78%), with a large variability in pressure levels, the most common range being 6 to 8cmH2O. The most common weaning parameters were as follows: tidal volume (92.6%), respiratory rate (93.3%) and oxygen saturation (90.4%). The most common waiting time for registration of the parameters was >15 minutes (40%). The measurements were preferably obtained from the ventilator display.
The methods and measurement parameters of ventilatory weaning vary greatly. The most commonly used method was continuous positive airway pressure with more pressure support and the most commonly used weaning parameters were the measured tidal volume and respiratory rate.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):212-217
DOI 10.5935/0103-507X.20130037
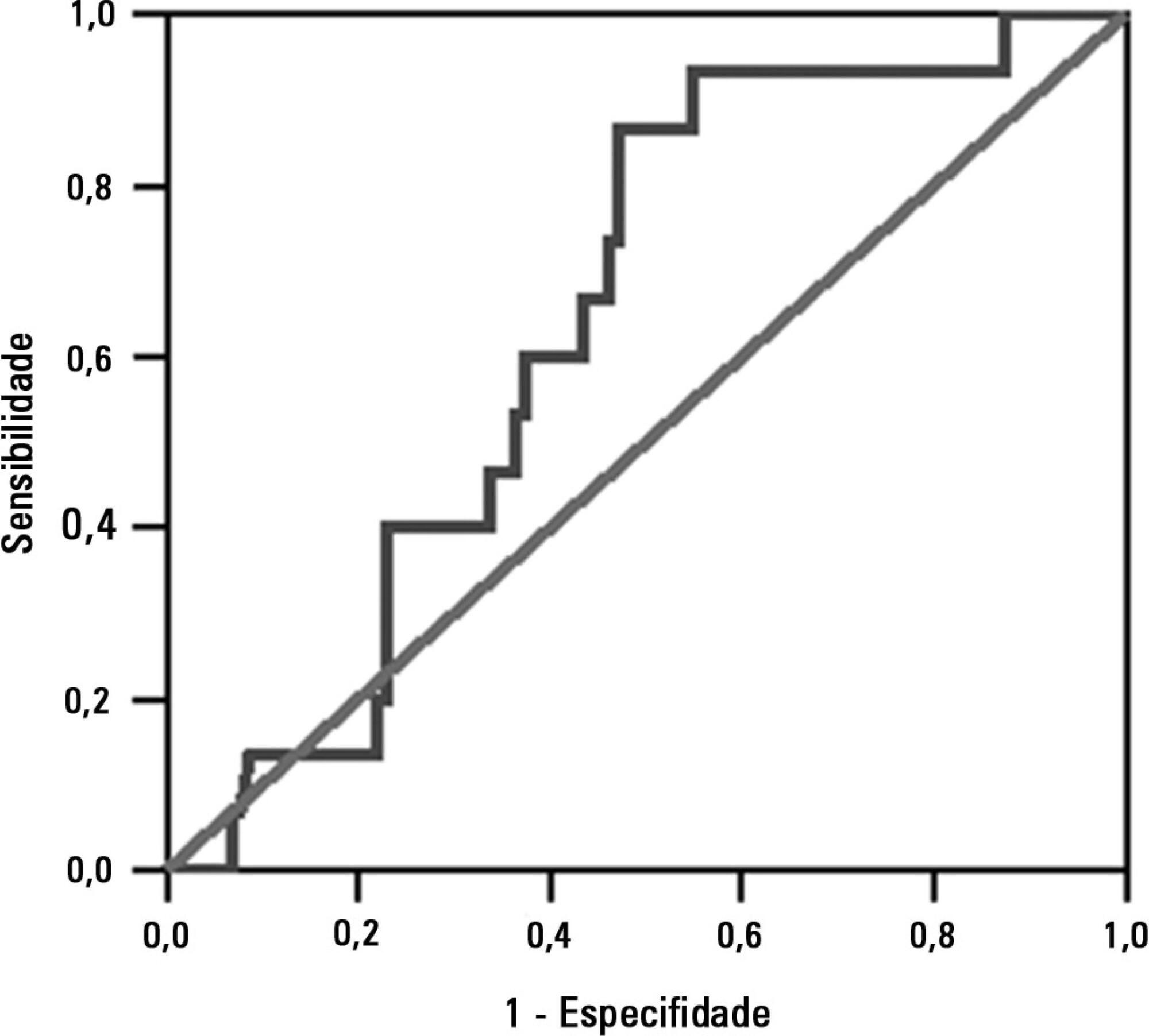
To investigate the association between the rapid shallow breathing index and successful extubation in patients with traumatic brain injury.
This study was a prospective study conducted in patients with traumatic brain injury of both genders who underwent mechanical ventilation for at least two days and who passed a spontaneous breathing trial. The minute volume and respiratory rate were measured using a ventilometer, and the data were used to calculate the rapid shallow breathing index (respiratory rate/tidal volume). The dependent variable was the extubation outcome: reintubation after up to 48 hours (extubation failure) or not (extubation success). The independent variable was the rapid shallow breathing index measured after a successful spontaneous breathing trial.
The sample comprised 119 individuals, including 111 (93.3%) males. The average age of the sample was 35.0±12.9 years old. The average duration of mechanical ventilation was 8.1±3.6 days. A total of 104 (87.4%) participants achieved successful extubation. No association was found between the rapid shallow breathing index and extubation success.
The rapid shallow breathing index was not associated with successful extubation in patients with traumatic brain injury.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):56-61
DOI 10.1590/S0103-507X2011000100010
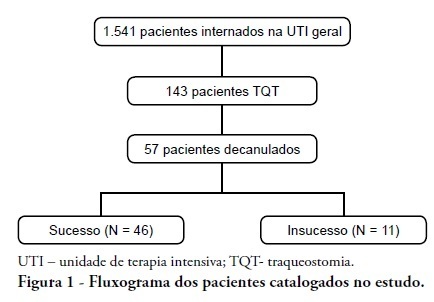
INTRODUCTION: Tracheostomy is probably the most common surgical procedure in critically ill patients and is generally performed to facilitate mechanical ventilation weaning. Evidence-based guidelines have confirmed the benefits of tracheostomy weaning protocols and of the physiotherapists engagement in this process; however, no consensus decannulation criteria are currently available. Therefore, this study aimed to evaluate the influence of peripheral muscle strength and other indicators on decannulation success. METHODS: This was an observational retrospective study that analyzed the medical records of patients admitted to the medical and surgical intensive care unit of Hospital Agamenon Magalhães between March 2007 and August 2009. Respiratory and peripheral muscle strengths were evaluated in decannulated patients. RESULTS: Overall, 1,541 patients were evaluated, 143 of which had been tracheostomized, and only 57 of which had been decannulated. Forty-six patients had a satisfactory decannulation outcome, while 11 had decannulation failure, requiring the return to an artificial airway within 2 weeks. The calculated Medical Research Council peripheral muscle strength score was significantly lower for the failure group than for the successful decannulation group (28.33 ± 15.31 vs. 41.11 ± 11.52; P = 0.04). Scores above or equal 26 had 94.4% sensitivity and 50.0% specificity for the decannulation outcome, with an area under the ROC curve of 0.7593. In addition, white blood cell counts were higher in decannulation failure group patients (14,070 ± 3,073 vs. 10,520 ± 3,402 cells/μL; P = 0.00). CONCLUSION: This study has shown that peripheral muscle strength and blood leucocyte counts evaluated on the day of decannulation may influence the tracheostomy decannulation success rate.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)