Abstract
Crit Care Sci. 2023;35(2):163-167
DOI 10.5935/2965-2774.20230009-pt
To assess the outcome of extubation in COVID-19 patients and the use of noninvasive ventilation in the weaning process.
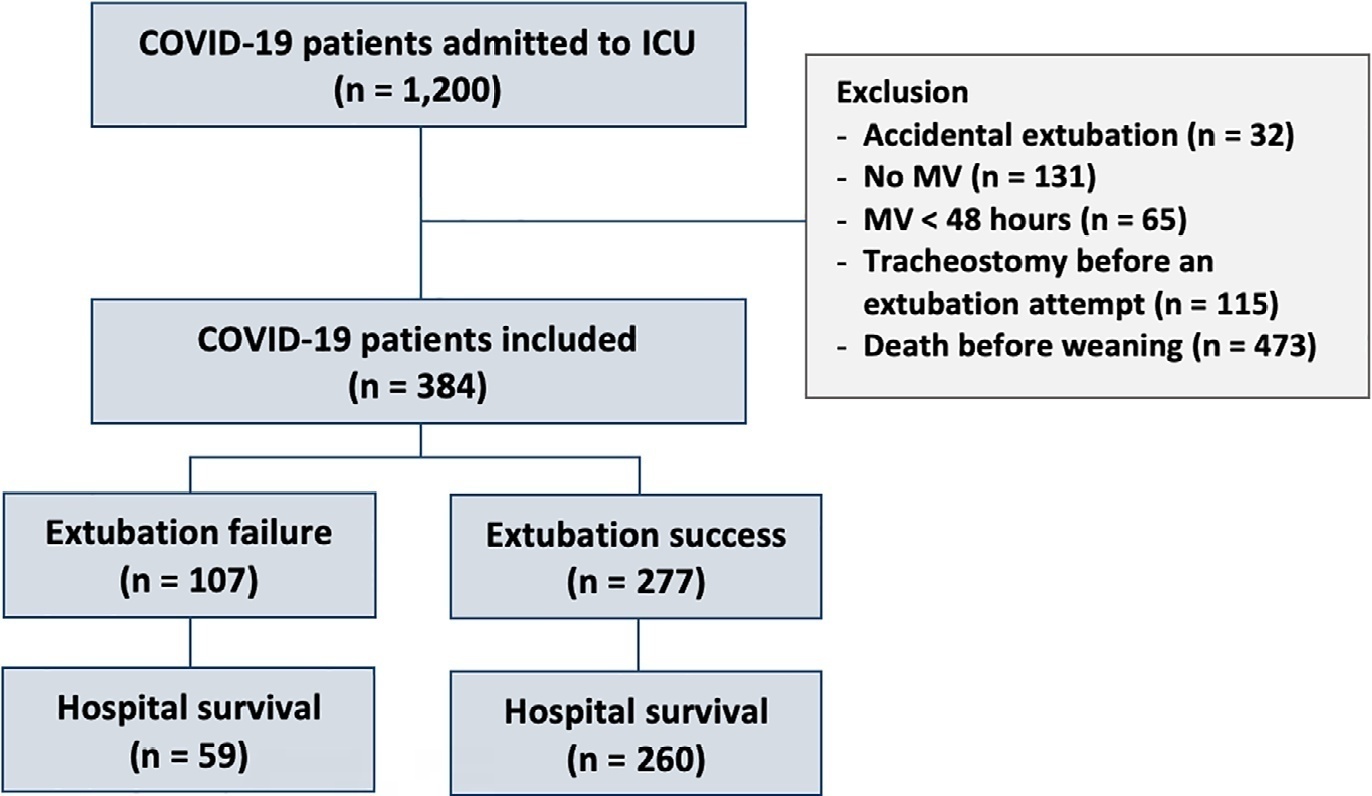
This retrospective, observational, single-center study was conducted in COVID-19 patients aged 18 years or older who were admitted to an intensive care unit between April 2020 and December 2021, placed under mechanical ventilation for more than 48 hours and progressed to weaning. Early extubation was defined as extubation without a spontaneous breathing trial and immediate use of noninvasive ventilation after extubation. In patients who underwent a spontaneous breathing trial, noninvasive ventilation could be used as prophylactic ventilatory assistance when started immediately after extubation (prophylactic noninvasive ventilation) or as rescue therapy in cases of postextubation respiratory failure (therapeutic noninvasive ventilation). The primary outcome was extubation failure during the intensive care unit stay.
Three hundred eighty-four extubated patients were included. Extubation failure was observed in 107 (27.9%) patients. Forty-seven (12.2%) patients received prophylactic noninvasive ventilation. In 26 (6.8%) patients, early extubation was performed with immediate use of noninvasive ventilation. Noninvasive ventilation for the management of postextubation respiratory failure was administered to 64 (16.7%) patients.
We found that COVID-19 patients had a high rate of extubation failure. Despite the high risk of extubation failure, we observed low use of prophylactic noninvasive ventilation in these patients.
Abstract
Rev Bras Ter Intensiva. 2022;34(2):247-254
DOI 10.5935/0103-507X.20220022-en
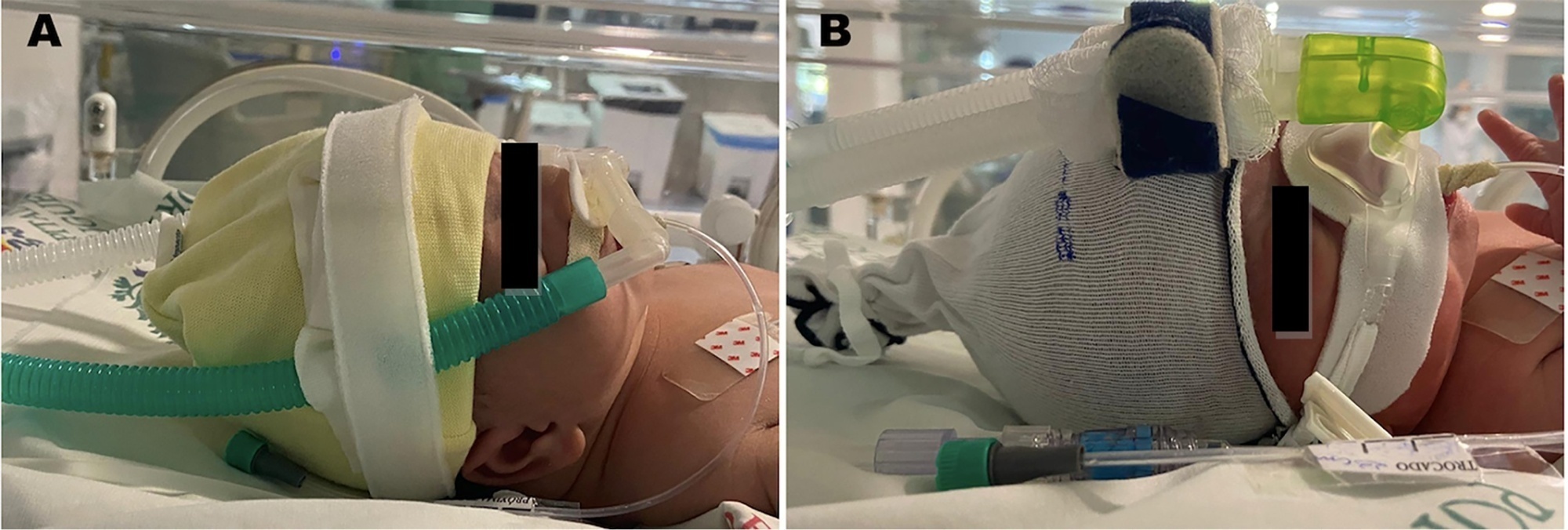
To investigate the association between noninvasive ventilation delivery devices and the incidence of nasal septum injury in preterm infants.
This retrospective singlecenter cohort study included preterm infants supported by noninvasive ventilation. The incidence of nasal injury was compared among three groups according to the noninvasive ventilation delivery device (G1 - nasal mask; G2 - binasal prongs; and G3, rotation of nasal mask with prongs). Nasal injury was classified according to the National Pressure Ulcer Advisory Panel as stages 1 - 4. Multivariate regression analyses were performed to estimate relative risks to identify possible predictors associated with medical device-related injuries.
Among the 300 infants included in the study, the incidence of medical device-related injuries in the rotating group was significantly lower than that in the continuous mask or prong groups (n = 68; 40.48%; p value < 0.01).
Rotating nasal masks with nasal prongs reduces the incidence of moderate to severe nasal injury in comparison with single devices. The addition of days using noninvasive ventilation seems to contribute to medical device-related injuries, and higher birth weight is a protective factor.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):362-373
DOI 10.5935/0103-507X.20210059
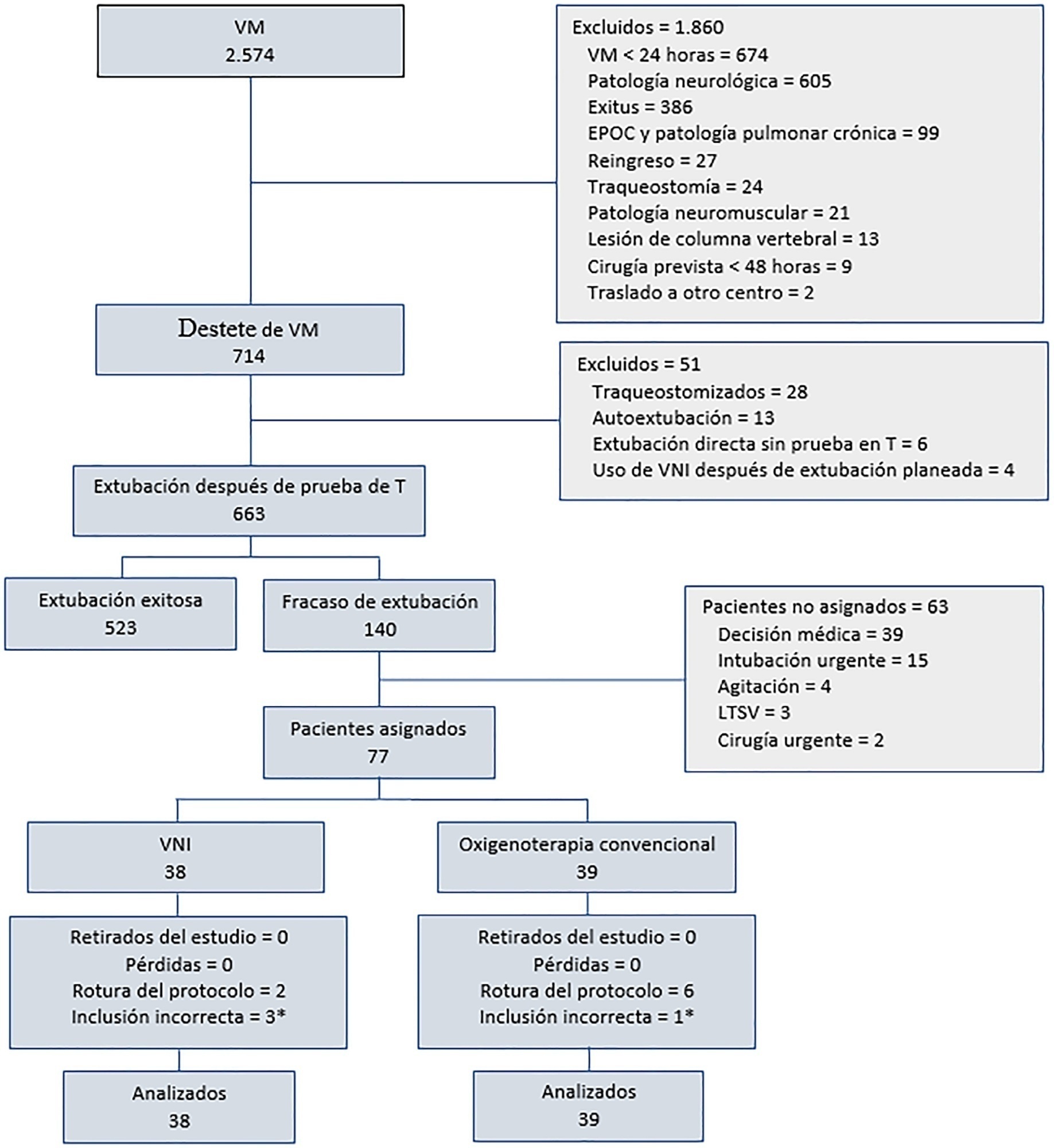
To determine the effectiveness of noninvasive ventilation versus conventional oxygen therapy in patients with acute respiratory failure after extubation failure.
A pragmatic clinical trial was conducted in an intensive care unit from March 2009 to September 2016. Patients on mechanical ventilation > 24 hours who developed acute respiratory failure after scheduled extubation were included and were assigned to noninvasive ventilation or conventional oxygen therapy. The primary objective was to reduce the reintubation rate. The secondary objectives were to improve respiratory parameters and reduce complications, the duration of mechanical ventilation, the intensive care unit stay, the hospital stay, and mortality in the intensive care unit, in the hospital, and 90 days after discharge. Factors correlated with reintubation were also analyzed.
Of a total of 2,574 patients, 77 were analyzed (38 in the noninvasive ventilation group and 39 in the conventional oxygen therapy group). Noninvasive ventilation reduced the respiratory and cardiac rates more rapidly than conventional oxygen therapy. Reintubation was less common in the noninvasive ventilation group [12 (32%) versus 22 (56%) in the conventional oxygen therapy group, relative risk 0.58 (95%CI 0.34 - 0.97), p = 0.039]. The rest of the parameters did not show significant differences. In the multivariate analysis, noninvasive ventilation protected against reintubation [OR 0.17 (95%CI 0.05 - 0.56), p = 0.004], while liver failure before extubation and the inability to maintain airway patency predisposed patients to reintubation.
The use of noninvasive ventilation in patients who failed extubation could be beneficial compared to conventional oxygen therapy.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):384-393
DOI 10.5935/0103-507X.20210055
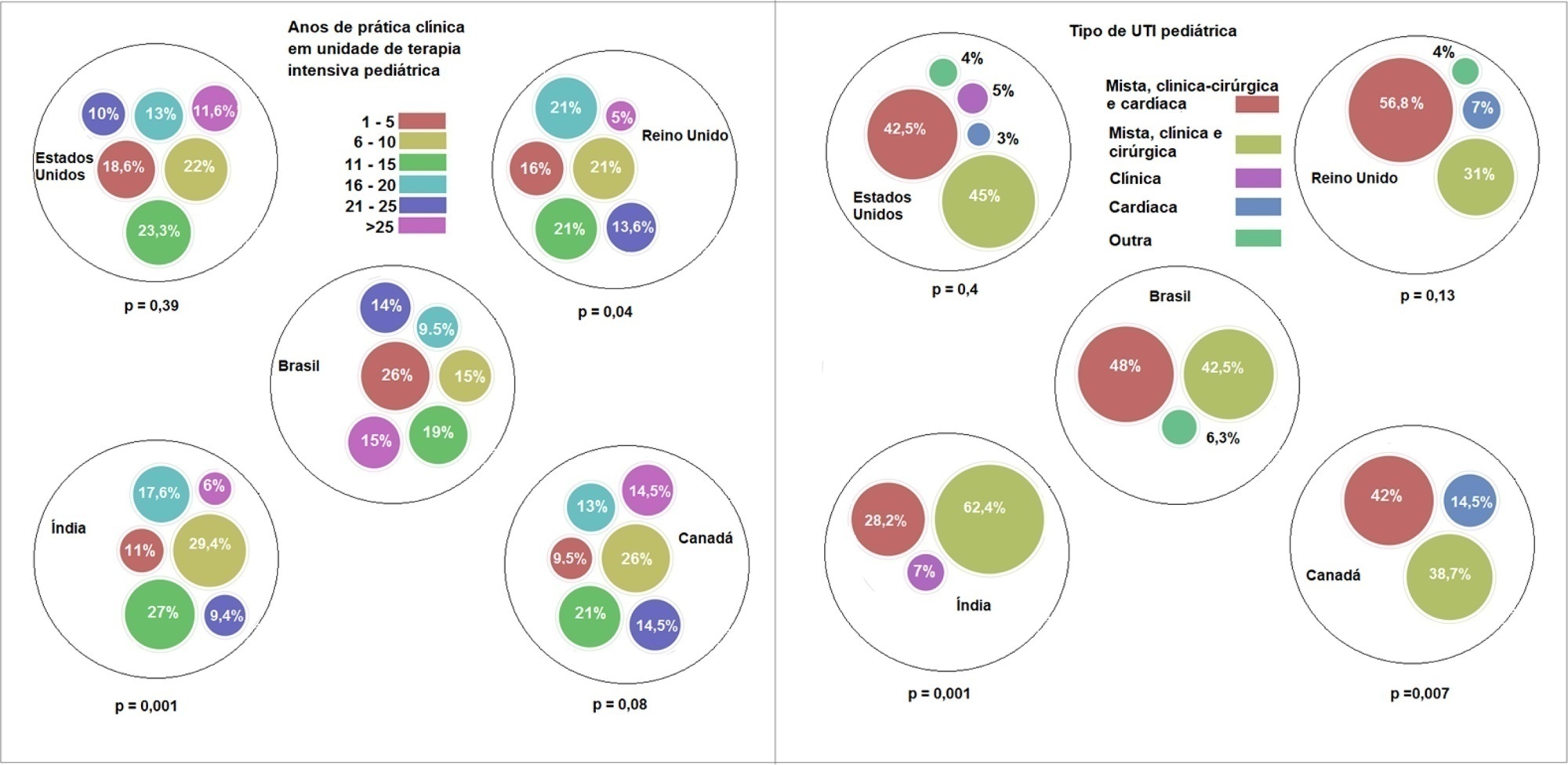
To describe current clinical practices related to the use of high-flow nasal cannula therapy by Brazilian pediatric intensivists and compare them with those in other countries.
A questionnaire was administered to pediatric intensivists in North and South America, Asia, Europe, and Australia/New Zealand for the main study. We compared the Brazilian cohort with cohorts in the United States of America, Canada, the United Kingdom, and India
Overall, 501 physicians responded, 127 of which were in Brazil. Only 63.8% of respondents in Brazil had a high-flow nasal cannula available, in contrast to 100% of respondents in the United Kingdom, Canada, and the United States. The attending physician was responsible for the decision to start a high-flow nasal cannula according to 61.2% respondents in Brazil, 95.5% in the United Kingdom, 96.6% in the United States, 96.8% in Canada, and 84.7% in India. A total of 62% of respondents in Brazil, 96.3% in the United Kingdom, 96.6% in the United States, 96.8% in Canada, and 84.7% in India reported that the attending physician was responsible for the decision to wean or modify the high-flow nasal cannula settings. When high-flow nasal cannula therapy failed due to respiratory distress/failure, 82% of respondents in Brazil would consider a trial of noninvasive ventilation before endotracheal intubation, compared to 93% in the United Kingdom, 88% in the United States, 91.5% in Canada, and 76.8% in India. More Brazilian intensivists (6.5%) than intensivists in the United Kingdom, United States, and India (1.6% for all) affirmed using sedatives frequently with high-flow nasal cannulas.
The availability of high-flow nasal cannulas in Brazil is still not widespread. There are some divergences in clinical practices between Brazilian intensivists and their colleagues abroad, mainly in processes and decision-making about starting and weaning high-flow nasal cannula therapy.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):422-427
DOI 10.5935/0103-507X.20210057
To assess whether there is an association between 48-hour postextubation fluid balance and extubation failure.
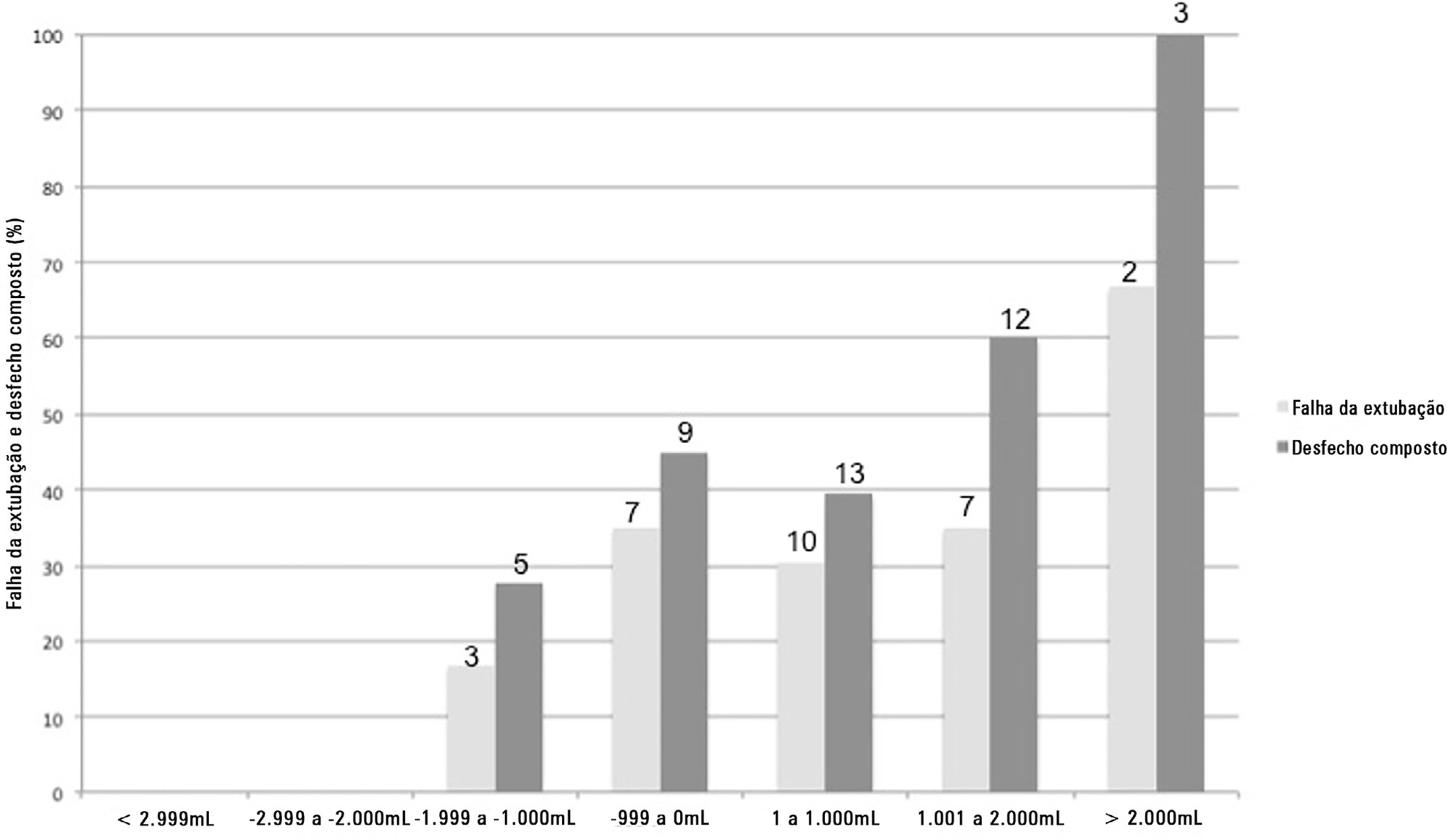
This was a prospective cohort study that included patients admitted to the intensive care unit of a tertiary hospital in southern Brazil from March 2019 to December 2019. Patients who required mechanical ventilation for at least 24 hours and who were extubated during the study period were included. The primary outcome was extubation failure, considered as the need for reintubation in the first 72 hours after extubation. The secondary outcome was a combined outcome with extubation failure or the need for therapeutic noninvasive ventilation.
A total of 101 patients were included. Extubation failure was observed in 29 (28.7%) patients. In univariate analysis, patients with a negative 48-hour postextubation fluid balance higher than one liter had a lower rate of extubation failure (12.0%) than patients with a negative 48-hour postextubation fluid balance lower than 1L (34.2%; p = 0.033). Mechanical ventilation duration and negative 48-hour postextubation fluid balance lower than one liter were associated with extubation failure when corrected for Simplified Acute Physiology Score 3 in multivariate analysis. When we evaluated the combined outcome, only negative 48-hour postextubation lower than 1L maintained an association when corrected for for Simplified Acute Physiology Score 3 and mechanical ventilation duration.
The 48-hour postextubation fluid balance is associated with extubation failure. Further studies are necessary to assess whether avoiding positive fluid balance in this period might improve weaning outcomes.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):68-74
DOI 10.5935/0103-507X.20210006
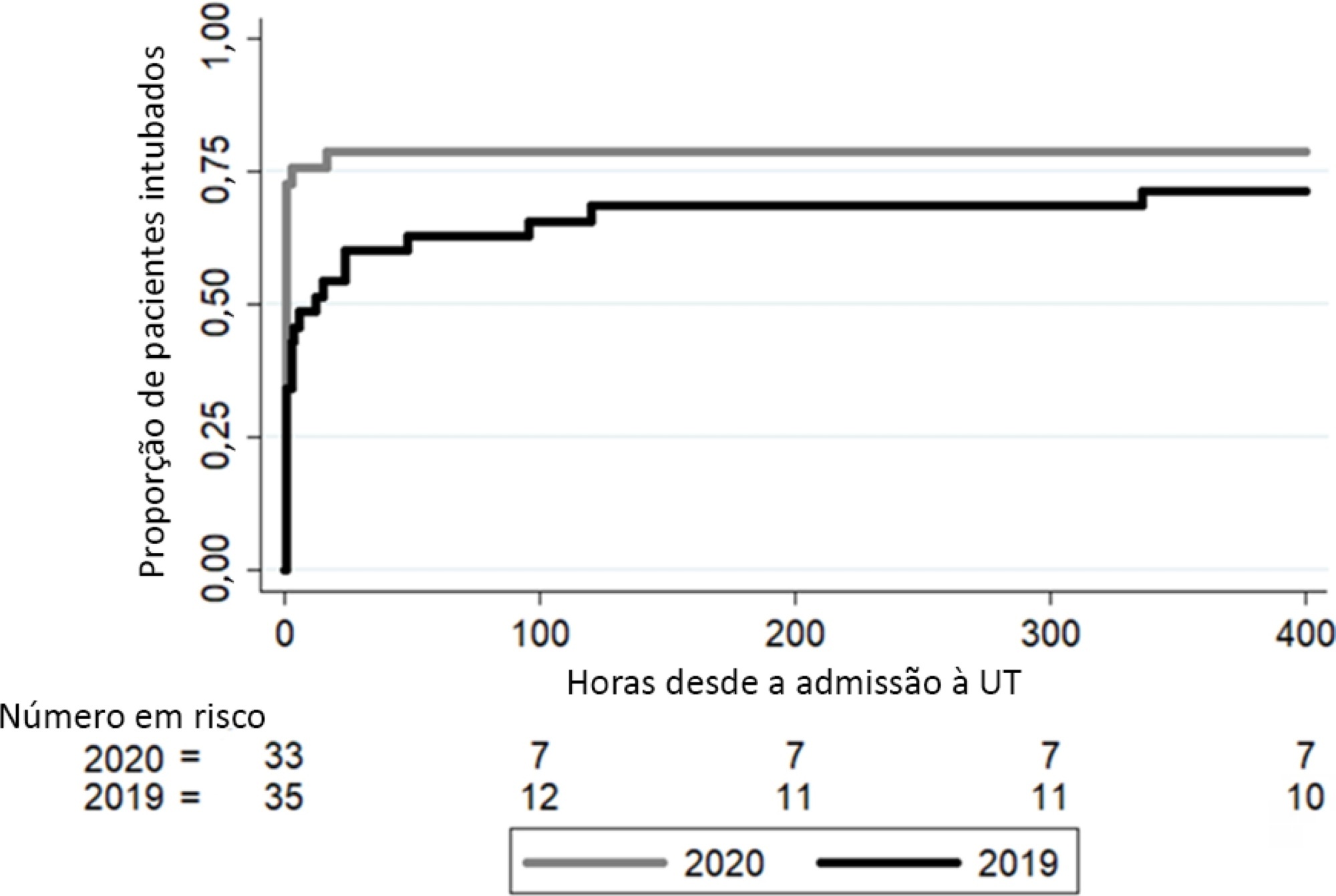
To analyze whether changes in medical care due to the application of COVID-19 protocols affected clinical outcomes in patients without COVID-19 during the pandemic.
This was a retrospective, observational cohort study carried out in a thirty-eight-bed surgical and medical intensive care unit of a high complexity private hospital. Patients with respiratory failure admitted to the intensive care unit during March and April 2020 and the same months in 2019 were selected. We compared interventions and outcomes of patients without COVID-19 during the pandemic with patients admitted in 2019. The main variables analyzed were intensive care unit respiratory management, number of chest tomography scans and bronchoalveolar lavages, intensive care unit complications, and status at hospital discharge.
In 2020, a significant reduction in the use of a high-flow nasal cannula was observed: 14 (42%) in 2019 compared to 1 (3%) in 2020. Additionally, in 2020, a significant increase was observed in the number of patients under mechanical ventilation admitted to the intensive care unit from the emergency department, 23 (69%) compared to 11 (31%) in 2019. Nevertheless, the number of patients with mechanical ventilation after 5 days of admission was similar in both years: 24 (69%) in 2019 and 26 (79%) in 2020.
Intensive care unit protocols based on international recommendations for the COVID-19 pandemic have produced a change in non-COVID-19 patient management. We observed a reduction in the use of a high-flow nasal cannula and an increased number of tracheal intubations in the emergency department. However, no changes in the percentage of intubated patients in the intensive care unit, the number of mechanical ventilation days or the length of stay in intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):333-339
DOI 10.5935/0103-507X.20190045
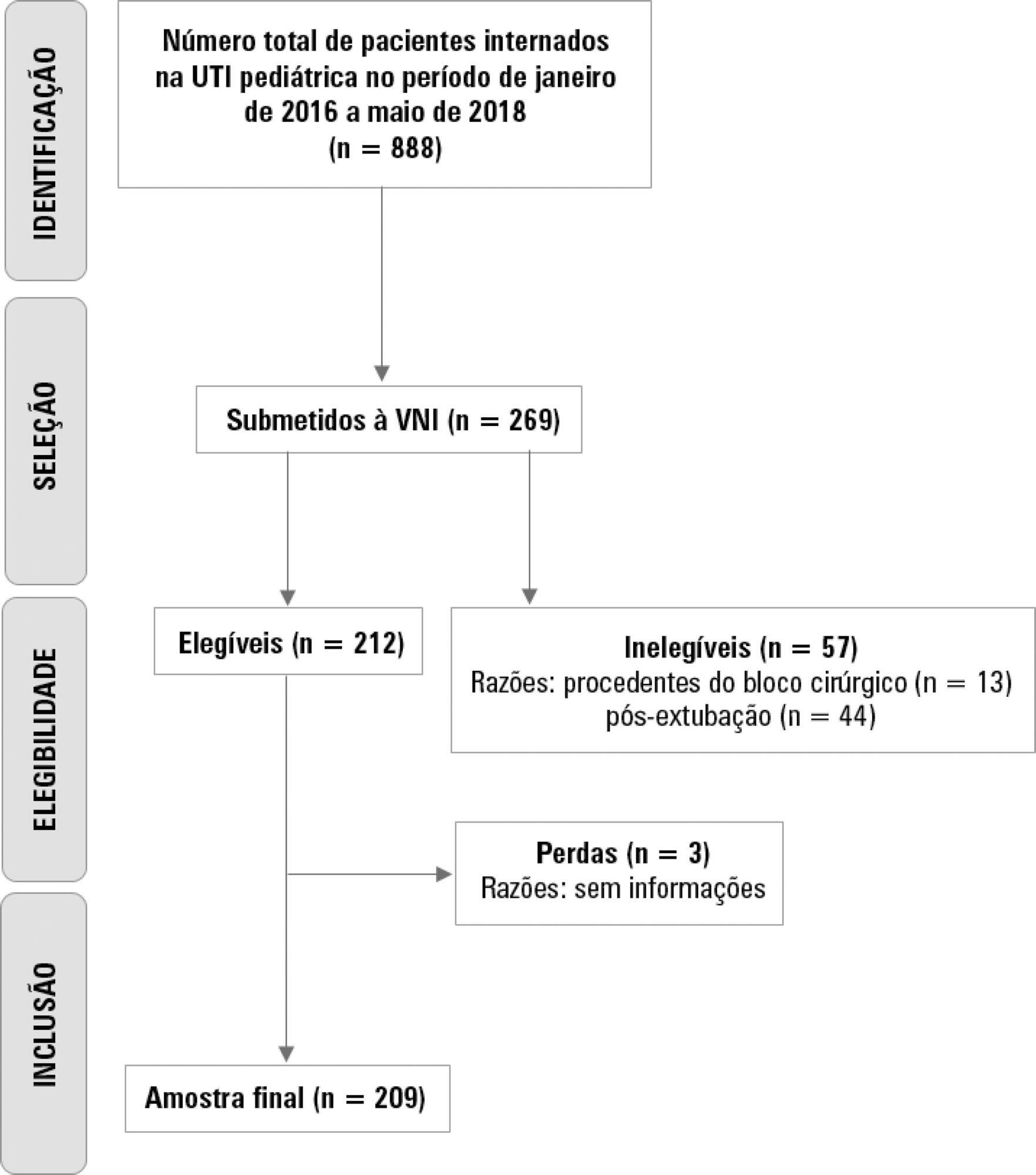
To describe the use of noninvasive ventilation to prevent tracheal intubation in children in a pediatric intensive care unit and to analyze the factors related to respiratory failure.
A retrospective cohort study was performed from January 2016 to May 2018. The study population included children aged 1 to 14 years who were subjected to noninvasive ventilation as the first therapeutic choice for acute respiratory failure. Biological, clinical and managerial data were analyzed by applying a model with the variables that obtained significance ≤ 0.20 in a bivariate analysis. Logistic regression was performed using the ENTER method. The level of significance was set at 5%.
The children had a mean age of 68.7 ± 42.3 months, 96.6% had respiratory disease as a primary diagnosis, and 15.8% had comorbidities. Of the 209 patients, noninvasive ventilation was the first option for ventilatory support in 86.6% of the patients, and the fraction of inspired oxygen was ≥ 0.40 in 47% of the cases. The lethality rate was 1.4%. The data for the use of noninvasive ventilation showed a high success rate of 95.3% (84.32 - 106). The Pediatric Risk of Mortality (PRISM) score and the length of stay in the intensive care unit were the significant clinical variables for the success or failure of noninvasive ventilation.
A high rate of effectiveness was found for the use of noninvasive ventilation for acute episodes of respiratory failure. A higher PRISM score on admission, comorbidities associated with respiratory symptoms and oxygen use ≥ 40% were independent factors related to noninvasive ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):487-495
DOI 10.5935/0103-507X.20180070
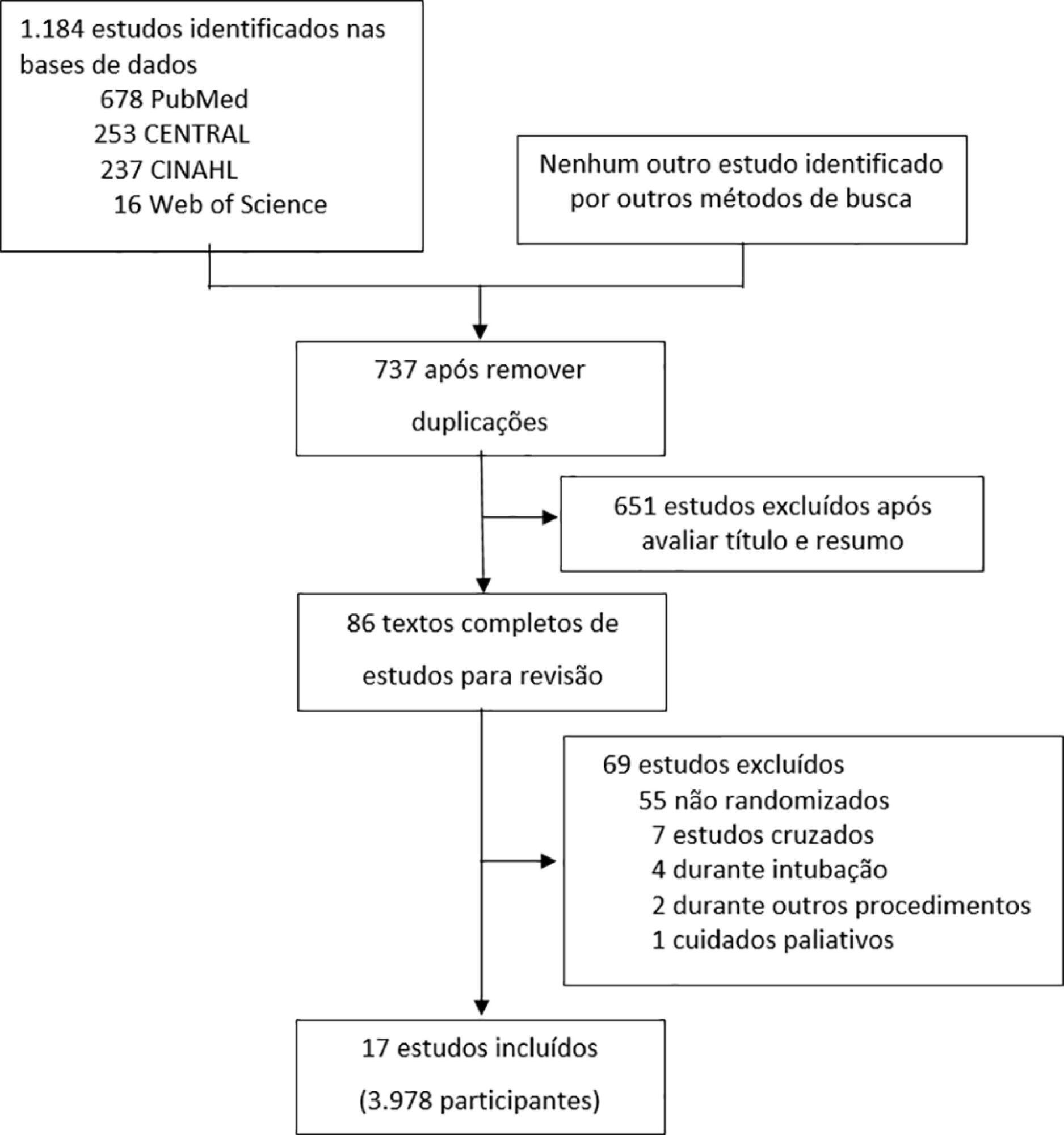
To evaluate the efficacy of high-flow nasal cannula in the prevention of intubation and re-intubation in critically ill patients compared to conventional oxygen therapy or noninvasive ventilation.
This systematic review was performed through an electronic database search of articles published from 1966 to April 2018. The primary outcome was the need for intubation or re-intubation. The secondary outcomes were therapy escalation, mortality at the longest follow-up, hospital mortality and the need for noninvasive ventilation.
Seventeen studies involving 3,978 patients were included. There was no reduction in the need for intubation or re-intubation with high-flow nasal cannula (OR 0.72; 95%CI 0.52 - 1.01; p = 0.056). There was no difference in the need for therapy escalation (OR 0.80, 95% CI 0.59 - 1.08, p = 0.144), mortality at the longest follow-up (OR 0.94; 95%CI 0.70 - 1.25; p = 0.667), hospital mortality (OR 0.84; 95%CI 0.56 - 1.26; p = 0.391) or noninvasive ventilation (OR 0.64, 95%CI 0.39 - 1.05, p = 0.075). In the trial sequential analysis, the number of events included was lower than the optimal information size with a global type I error > 0.05.
In the present study and setting, high-flow nasal cannula was not associated with a reduction of the need for intubation or re-intubation in critically ill patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)