Abstract
Rev Bras Ter Intensiva. 2017;29(2):180-187
DOI 10.5935/0103-507X.20170028
To analyze patients after cardiac surgery that needed endotracheal reintubation and identify factors associated with death and its relation with the severity scores.
Retrospective analysis of information of 1,640 patients in the postoperative period of cardiac surgery between 2007 and 2015.
The reintubation rate was 7.26%. Of those who were reintubated, 36 (30.3%) underwent coronary artery bypass surgery, 27 (22.7%) underwent valve replacement, 25 (21.0%) underwent correction of an aneurysm, and 8 (6.7%) underwent a heart transplant. Among those with comorbidities, 54 (51.9%) were hypertensive, 22 (21.2%) were diabetic, and 10 (9.6%) had lung diseases. Among those who had complications, 61 (52.6%) had pneumonia, 50 (42.4%) developed renal failure, and 49 (51.0%) had a moderate form of the transient disturbance of gas exchange. Noninvasive ventilation was performed in 53 (44.5%) patients. The death rate was 40.3%, and mortality was higher in the group that did not receive noninvasive ventilation before reintubation (53.5%). Within the reintubated patients who died, the SOFA and APACHE II values were 7.9 ± 3.0 and 16.9 ± 4.5, respectively. Most of the reintubated patients (47.5%) belonged to the high-risk group, EuroSCORE (> 6 points).
The reintubation rate was high, and it was related to worse SOFA, APACHE II and EuroSCORE scores. Mortality was higher in the group that did not receive noninvasive ventilation before reintubation.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):212-219
DOI 10.5935/0103-507X.20150034
To evaluate the clinical characteristics of patients with hematological disease admitted to the intensive care unit and the use of noninvasive mechanical ventilation in a subgroup with respiratory dysfunction.
A retrospective observational study from September 2011 to January 2014.
Overall, 157 patients were included. The mean age was 45.13 (± 17.2) years and 46.5% of the patients were female. Sixty-seven (48.4%) patients had sepsis, and 90 (57.3%) patients required vasoactive vasopressors. The main cause for admission to the intensive care unit was acute respiratory failure (94.3%). Among the 157 studied patients, 47 (29.9%) were intubated within the first 24 hours, and 38 (24.2%) underwent noninvasive mechanical ventilation. Among the 38 patients who initially received noninvasive mechanical ventilation, 26 (68.4%) were subsequently intubated, and 12 (31.6%) responded to this mode of ventilation. Patients who failed to respond to noninvasive mechanical ventilation had higher intensive care unit mortality (66.7% versus 16.7%; p = 0.004) and a longer stay in the intensive care unit (9.6 days versus 4.6 days, p = 0.02) compared with the successful cases. Baseline severity scores (SOFA and SAPS 3) and the total leukocyte count were not significantly different between these two subgroups. In a multivariate logistic regression model including the 157 patients, intubation at any time during the stay in the intensive care unit and SAPS 3 were independently associated with intensive care unit mortality, while using noninvasive mechanical ventilation was not.
In this retrospective study with severely ill hematologic patients, those who underwent noninvasive mechanical ventilation at admission and failed to respond to it presented elevated intensive care unit mortality. However, only intubation during the intensive care unit stay was independently associated with a poor outcome. Further studies are needed to define predictors of noninvasive mechanical ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):360-368
DOI 10.5935/0103-507X.20150061
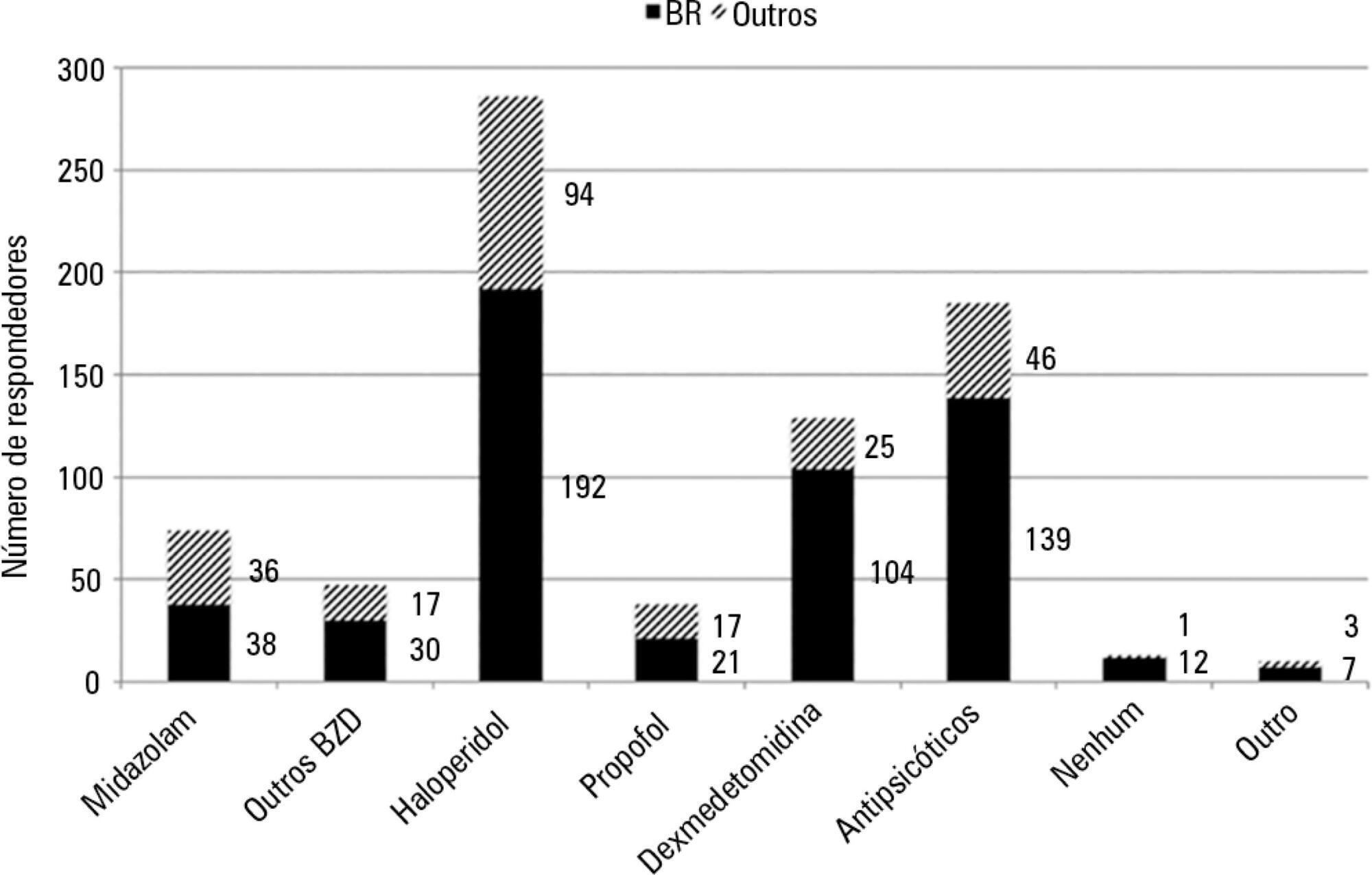
To conduct a multinational survey of intensive care unit professionals to determine the practices on delirium assessment and management, in addition to their perceptions and attitudes toward the evaluation and impact of delirium in patients requiring noninvasive ventilation.
An electronic questionnaire was created to evaluate the profiles of the respondents and their related intensive care units, the systematic delirium assessment and management and the respondents' perceptions and attitudes regarding delirium in patients requiring noninvasive ventilation. The questionnaire was distributed to the cooperative network for research of the Associação de Medicina Intensiva Brasileira (AMIB-Net) mailing list and to researchers in different centers in Latin America and Europe.
Four hundred thirty-six questionnaires were available for analysis; the majority of the questionnaires were from Brazil (61.9%), followed by Turkey (8.7%) and Italy (4.8%). Approximately 61% of the respondents reported no delirium assessment in the intensive care unit, and 31% evaluated delirium in patients under noninvasive ventilation. The Confusion Assessment Method for the intensive care unit was the most reported validated diagnostic tool (66.9%). Concerning the indication of noninvasive ventilation in patients already presenting with delirium, 16.3% of respondents never allow the use of noninvasive ventilation in this clinical context.
This survey provides data that strongly reemphasizes poor efforts toward delirium assessment and management in the intensive care unit setting, especially regarding patients requiring noninvasive ventilation.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):390-396
DOI 10.5935/0103-507X.20150065
To evaluate the quality of available evidence to establish guidelines for the use of noninvasive ventilation for the management of status asthmaticus in children unresponsive to standard treatment.
Search, selection and analysis of all original articles on asthma and noninvasive ventilation in children, published until September 1, 2014 in all languages in the electronic databases PubMed, Web of Science, Cochrane Library, Scopus and SciELO, located using the search terms: "asthma", "status asthmaticus", "noninvasive ventilation", "Bronchospasm", "continuous positive airway pressure", "child", "infant", "pediatrics", "hypercapnia", "respiratory failure" and the keywords "BIPAP", "CPAP", "Bilevel", "acute asthma" and "near fatal asthma". The articles were assessed based on the levels of evidence of the GRADE system.
Only nine original articles were located; two (22%) articles had level of evidence A, one (11%) had level of evidence B and six (67%) had level of evidence C.
The results suggest that noninvasive ventilation is applicable for the treatment of status asthmaticus in most pediatric patients unresponsive to standard treatment. However, the available evidence cannot be considered as conclusive, as further high-quality research is likely to have an impact on and change the estimate of the effect.
Abstract
Rev Bras Ter Intensiva. 2014;26(3):317-320
DOI 10.5935/0103-507X.20140045
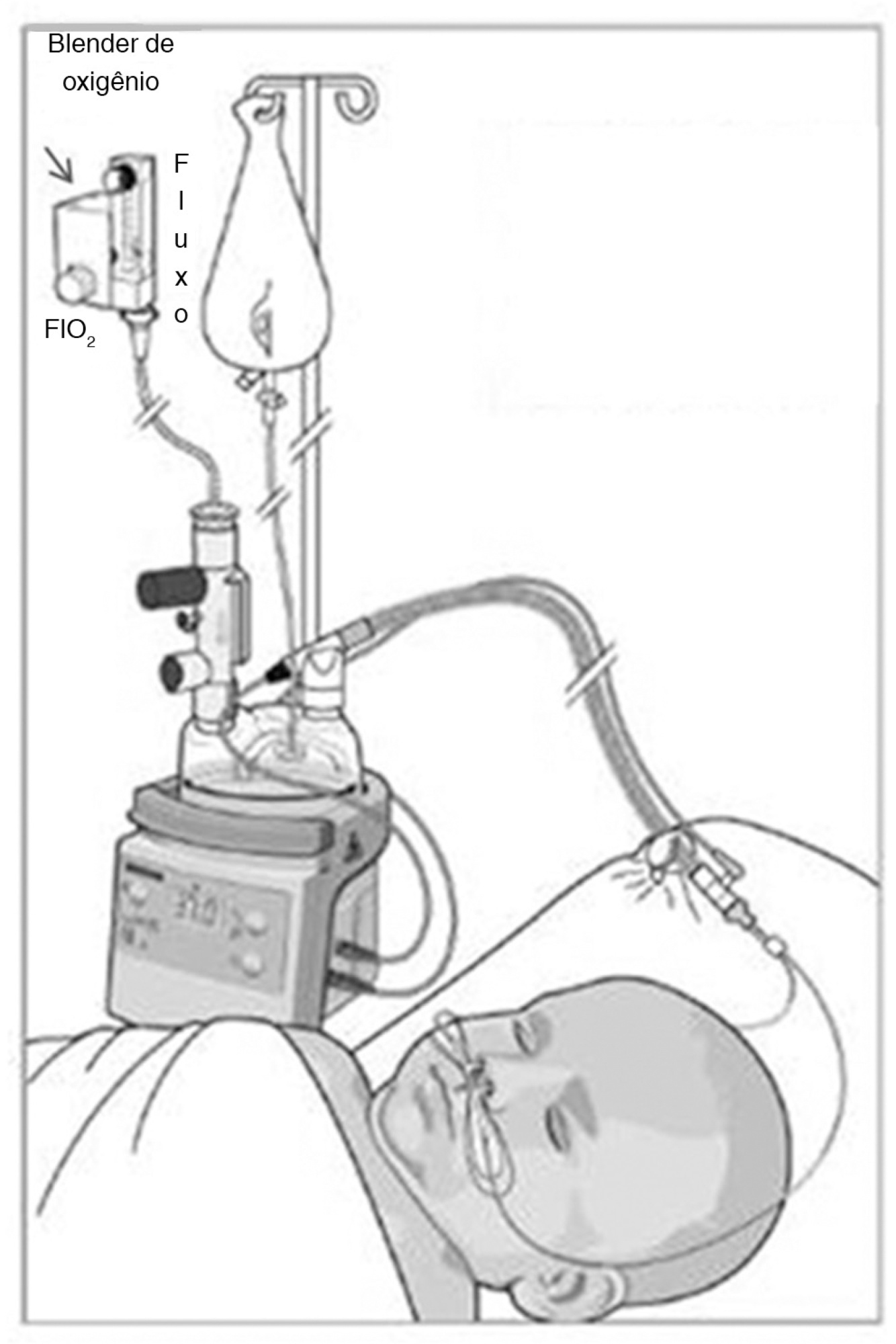
Atelectasis is a pulmonary disorder that lengthens the hospitalization time of newborns in intensive care units, resulting in increased morbidity among these infants. High-flow nasal cannulae have been used in newborns to prevent atelectasis and/or expand pulmonary regions affected by atelectasis; however, to date, no evidence-based data regarding this approach have been reported. In this paper, we report on the cases of two male newborn patients. The first and second patients described in this report were hospitalized for a neurosurgical procedure and the treatment of abdominal disease, respectively, and were subjected to invasive mechanical ventilation for 4 and 36 days, respectively. After extubation, these patients continued receiving oxygen therapy but experienced clinical and radiological worsening typical of atelectasis. In both cases, by 24 hours after the implantation of an high-flow nasal cannulae to provide noninvasive support, radiological examinations revealed the complete resolution of atelectasis. In these cases, the use of an high-flow nasal cannulae was effective in reversing atelectasis. Thus, this approach may be utilized as a supplemental noninvasive ventilatory therapy to avoid unnecessary intubation.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):210-212
DOI 10.1590/S0103-507X2008000200016
BACKGROUND AND OBJECTIVES: Pneumocystis jirovecii pneumonia has been one of the most common diseases and life-threatening infectious complications in acquired immunodeficiency syndrome patients. The objective of the case report was to present a patient with probable diagnosis of Pneumocystis jirovecii pneumonia who received noninvasive positive pressure ventilation. CASE REPORT: A female patient, 25 years old, with probable diagnosis of Pneumocystis jirovecii pneumonia received noninvasive positive pressure ventilation. CONCLUSIONS: All respiratory parameters progressively improved in the first five days. Results suggest the efficacy of this support to improve oxygenation, to revert hypoxemia and to prevent orotracheal intubation.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):399-407
DOI 10.1590/S0103-507X2007000300023
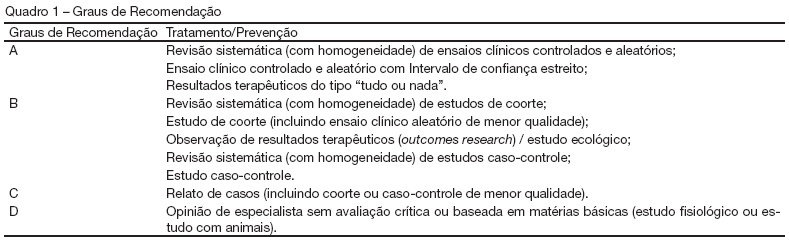
BACKGROUND AND OBJECTIVES: The II Brazilian Consensus Conference on Mechanical Ventilation was published in 2000. Knowledge on the field of mechanical ventilation evolved rapidly since then, with the publication of numerous clinical studies with potential impact on the ventilatory management of critically ill patients. Moreover, the evolving concept of evidence - based medicine determined the grading of clinical recommendations according to the methodological value of the studies on which they are based. This explicit approach has broadened the understanding and adoption of clinical recommendations. For these reasons, AMIB - Associação de Medicina Intensiva Brasileira and SBPT - Sociedade Brasileira de Pneumologia e Tisiologia - decided to update the recommendations of the II Brazilian Consensus. Physical therapy during mechanical ventilation has been one of the updated topics. This objective was described the most important topics on the physical therapy during mechanical ventilation. METHODS: Systematic review of the published literature and gradation of the studies in levels of evidence, using the key words: mechanical ventilation and physical therapy. RESULTS: Recommendations on the most important techniques applied during mechanical ventilation. CONCLUSIONS: Physical therapy has a central role at the Intensive Care environment, mainly in patients submitted to a mechanical ventilatory support invasive or non invasive.