Abstract
Rev Bras Ter Intensiva. 2016;28(2):167-178
DOI 10.5935/0103-507X.20160020
Asthma is the most common chronic illness in childhood. Although the vast majority of children with acute asthma exacerbations do not require critical care, some fail to respond to standard treatment and require escalation of support. Children with critical or near-fatal asthma require close monitoring for deterioration and may require aggressive treatment strategies. This review examines the available evidence supporting therapies for critical and near-fatal asthma and summarizes the contemporary clinical care of these children. Typical treatment includes parenteral corticosteroids and inhaled or intravenous beta-agonist drugs. For children with an inadequate response to standard therapy, inhaled ipratropium bromide, intravenous magnesium sulfate, methylxanthines, helium-oxygen mixtures, and non-invasive mechanical support can be used. Patients with progressive respiratory failure benefit from mechanical ventilation with a strategy that employs large tidal volumes and low ventilator rates to minimize dynamic hyperinflation, barotrauma, and hypotension. Sedatives, analgesics and a neuromuscular blocker are often necessary in the early phase of treatment to facilitate a state of controlled hypoventilation and permissive hypercapnia. Patients who fail to improve with mechanical ventilation may be considered for less common approaches, such as inhaled anesthetics, bronchoscopy, and extracorporeal life support. This contemporary approach has resulted in extremely low mortality rates, even in children requiring mechanical support.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):87-91
DOI 10.5935/0103-507X.20160005
Helium was discovered in 1868 by the French astronomer Pierre-Jules-César Janssen and was first used as a therapeutic treatment for airway obstruction by Barach almost 70 years later, in 1934. Heliox is characterized by its low density, which makes it more fluid under conditions of turbulence, thus minimizing airway pressure and facilitating the occurrence of laminar flow. The present article describes two clinical cases of patients with status asthmaticus subjected to mechanical ventilation and refractory to treatment in whom heliox was used, which allowed optimization of the efficacy of conventional pharmacological treatments. Although heliox is still used sporadically and its true efficacy has not been well demonstrated, the unique physical properties of helium and the theoretical improvement of the airflow in obstructed airways have produced scientific interest and stimulated research. Heliox can be used simultaneously with conventional therapies in cases of serious and refractory exacerbations of severe obstructive disease.

Abstract
Rev Bras Ter Intensiva. 2015;27(4):390-396
DOI 10.5935/0103-507X.20150065
To evaluate the quality of available evidence to establish guidelines for the use of noninvasive ventilation for the management of status asthmaticus in children unresponsive to standard treatment.
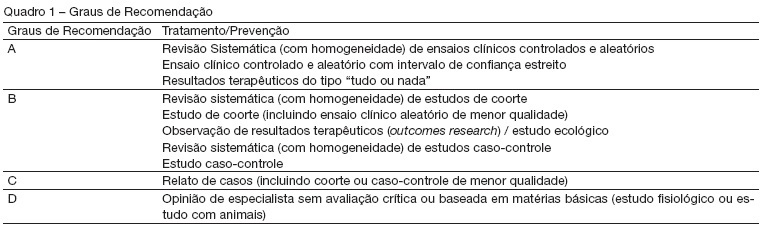
Search, selection and analysis of all original articles on asthma and noninvasive ventilation in children, published until September 1, 2014 in all languages in the electronic databases PubMed, Web of Science, Cochrane Library, Scopus and SciELO, located using the search terms: "asthma", "status asthmaticus", "noninvasive ventilation", "Bronchospasm", "continuous positive airway pressure", "child", "infant", "pediatrics", "hypercapnia", "respiratory failure" and the keywords "BIPAP", "CPAP", "Bilevel", "acute asthma" and "near fatal asthma". The articles were assessed based on the levels of evidence of the GRADE system.
Only nine original articles were located; two (22%) articles had level of evidence A, one (11%) had level of evidence B and six (67%) had level of evidence C.
The results suggest that noninvasive ventilation is applicable for the treatment of status asthmaticus in most pediatric patients unresponsive to standard treatment. However, the available evidence cannot be considered as conclusive, as further high-quality research is likely to have an impact on and change the estimate of the effect.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):86-90
DOI 10.1590/S0103-507X2012000100013
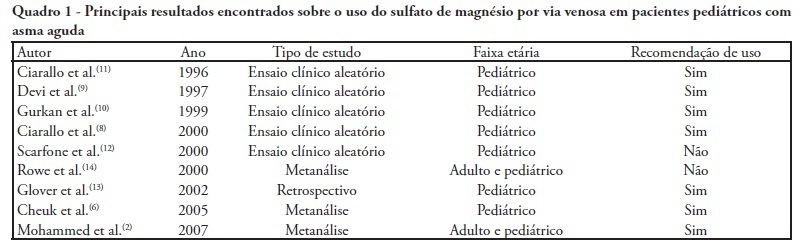
Severe acute asthma is a medical emergency that must be quickly diagnosed and treated. Initial treatment includes a bronchodilator agent and systemic corticosteroids. In severe cases with poor response to the standard treatment, intravenous magnesium sulfate is a therapeutic option. This article aimed a literature review on the use of intravenous magnesium sulfate in the emergency room treatment of children with acute asthma. The treatment parameters of effectiveness, indication, dosage, adverse effects and contraindications were assessed. A narrative review of the literature based on a search of the Medline and Lilacs databases and the Cochrane Database of Systematic Reviews for articles published between 2000 and 2010 was conducted. The keywords used included the following: asthma, children, emergency and magnesium sulfate. Eight controlled clinical trials, three meta-analyses, one retrospective study, eight review articles and one cross-sectional study were included. A total of 21 articles were analyzed. Several authors reported that intravenous magnesium was effective in the treatment of acute asthma in children. Adverse effects were rare. The use of intravenous magnesium sulfate was indicated for patients with moderate to severe acute asthma not responding to initial treatment with a bronchodilator agent and systemic corticosteroids. Few contraindications were reported but included kidney failure and atrioventricular block. Reports of adverse drug interactions with magnesium were rare. Although reported as safe, intravenous magnesium is infrequently used in children with acute asthma. Most often it is used in severe, progressed cases to prevent respiratory failure and/or admission to the intensive care unit. Intravenous magnesium was concluded to be effective and safe in children with severe acute asthma, although its use in the emergency room is still limited.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):369-373
DOI 10.1590/S0103-507X2007000300019
BACKGROUND AND OBJECTIVES: Magnesium sulfate has been shown to benefit asthmatic children and adults with poor responses to initial beta-agonist therapy and systemic corticoids in the emergency department. The aim of this study was to realize a no systematic review about the treatment of the acute asthma with intravenous and nebulized magnesium sulfate in the emergence. CONTENTS: The first investigations that demonstrate the benefit in the use of the magnesium sulfate in asthma date to 1938. The effects of magnesium sulfate may be mediated through its action as a calcium antagonist or through its function as a cofactor in enzyme systems involving ion flux across cell membranes. We realized a literature review using MedLine database of the last six years (2000 to 2006). Articles published in English were included by the crossing of keywords asthma and magnesium sulfate. CONCLUSIONS: The routine administration of intravenous and nebulized magnesium sulfate to severely ill patients with acute asthma presents in the emergence department is not recommended, however as an adjunct therapy brings some benefit.
Abstract
Rev Bras Ter Intensiva. 2007;19(2):258-263
DOI 10.1590/S0103-507X2007000200020
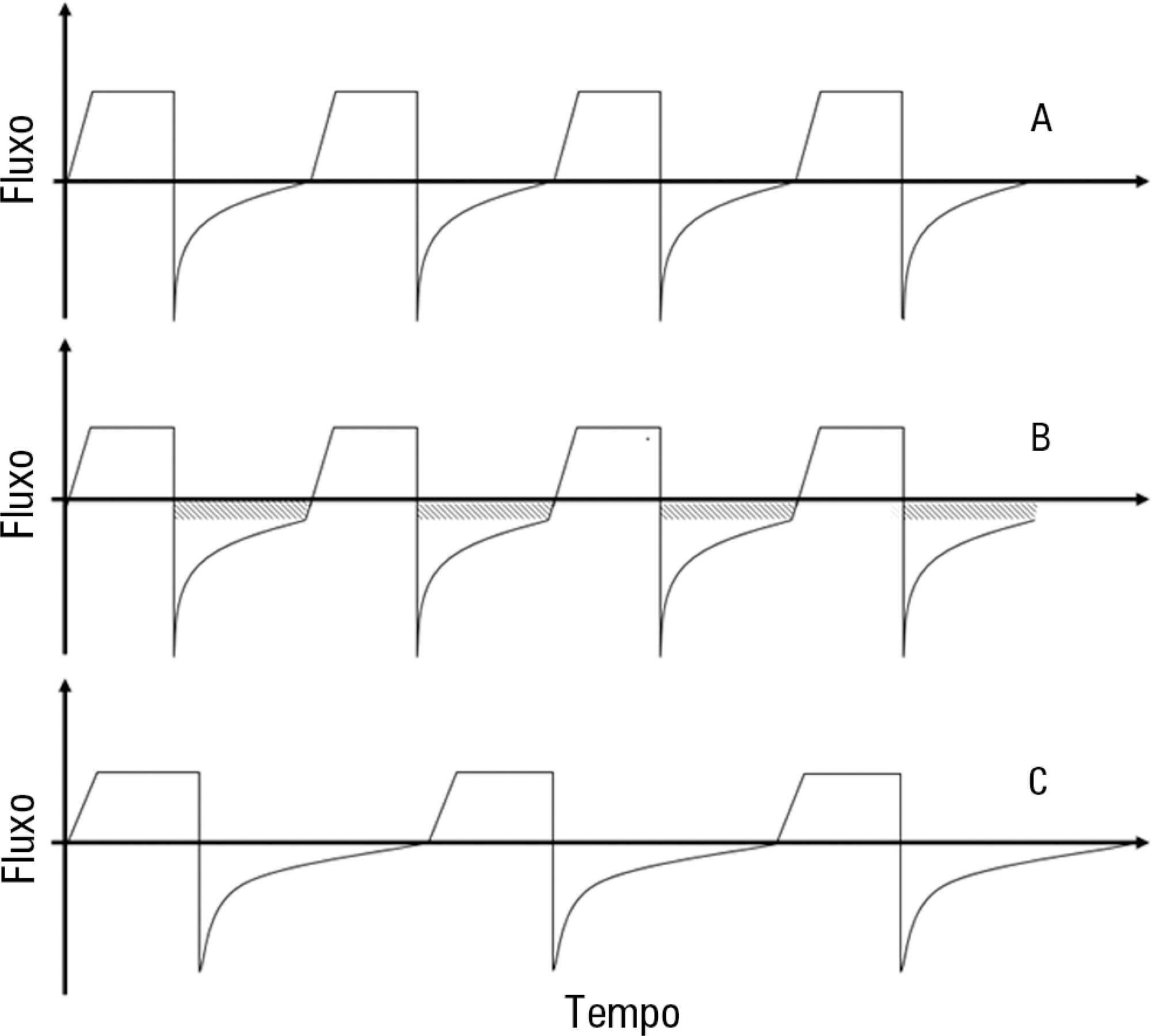
BACKGROUND AND OBJECTIVES: The II Brazilian Consensus Conference on Mechanical Ventilation was published in 2000. Knowledge on the field of mechanical ventilation evolved rapidly since then, with the publication of numerous clinical studies with potential impact on the ventilatory management of critically ill patients. Moreover, the evolving concept of evidence - based medicine determined the grading of clinical recommendations according to the methodological value of the studies on which they are based. This explicit approach has broadened the understanding and adoption of clinical recommendations. For these reasons, AMIB - Associação de Medicina Intensiva Brasileira and SBPT - Sociedade Brasileira de Pneumologia e Tisiologia - decided to update the recommendations of the II Brazilian Consensus. Mechanical ventilation in the asthma attack has been one of the updated topics. Describe the most important topics on the mechanical ventilation during the asthma attack and suggest the main therapeutic approaches. METHODS: Systematic review of the published literature and gradation of the studies in levels of evidence, using the key words "mechanical ventilation" and "asthma". RESULTS: We present recommendations on the ventilatory modes and settings to be adopted when ventilating a patient during an asthma attack, as well as the recommended monitoring. Alternative ventilation techniques are also presented. CONCLUSIONS: Protective ventilatory strategies are recommended when ventilating a patient during a severe asthma attack.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)