Abstract
Rev Bras Ter Intensiva. 2012;24(1):86-90
DOI 10.1590/S0103-507X2012000100013
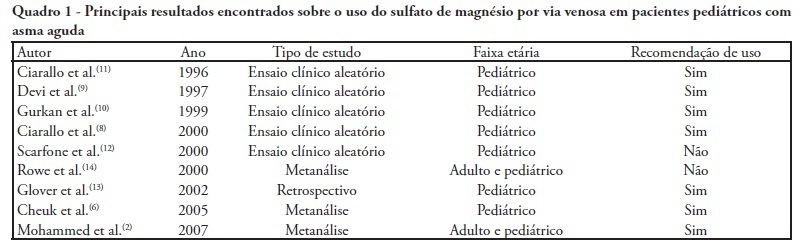
Severe acute asthma is a medical emergency that must be quickly diagnosed and treated. Initial treatment includes a bronchodilator agent and systemic corticosteroids. In severe cases with poor response to the standard treatment, intravenous magnesium sulfate is a therapeutic option. This article aimed a literature review on the use of intravenous magnesium sulfate in the emergency room treatment of children with acute asthma. The treatment parameters of effectiveness, indication, dosage, adverse effects and contraindications were assessed. A narrative review of the literature based on a search of the Medline and Lilacs databases and the Cochrane Database of Systematic Reviews for articles published between 2000 and 2010 was conducted. The keywords used included the following: asthma, children, emergency and magnesium sulfate. Eight controlled clinical trials, three meta-analyses, one retrospective study, eight review articles and one cross-sectional study were included. A total of 21 articles were analyzed. Several authors reported that intravenous magnesium was effective in the treatment of acute asthma in children. Adverse effects were rare. The use of intravenous magnesium sulfate was indicated for patients with moderate to severe acute asthma not responding to initial treatment with a bronchodilator agent and systemic corticosteroids. Few contraindications were reported but included kidney failure and atrioventricular block. Reports of adverse drug interactions with magnesium were rare. Although reported as safe, intravenous magnesium is infrequently used in children with acute asthma. Most often it is used in severe, progressed cases to prevent respiratory failure and/or admission to the intensive care unit. Intravenous magnesium was concluded to be effective and safe in children with severe acute asthma, although its use in the emergency room is still limited.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):478-483
DOI 10.1590/S0103-507X2011000400013
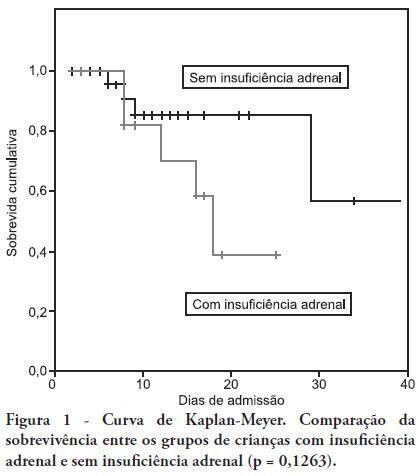
OBJECTIVE: To determine the frequency of adrenal insufficiency in children diagnosed with sepsis that were staying in pediatric intensive care units and to establish the association between adrenal function and the use of vasoactive drugs, mechanical ventilation time and mortality. METHODS: A cohort-designed study was conducted to assess the incidence of adrenal insufficiency in children aged 29 days to 12 years who were diagnosed with sepsis using the adrenocorticotropic hormone (ACTH) stimulation test. RESULTS: Thirty-nine children were included in the study. The frequency of adrenal insufficiency was 30.7% (12 patients). Children with adrenal insufficiency had an increased need for vasoactive drugs as well as longer mechanical ventilation times; however, the differences were not statistically significant. A Kaplan-Meier curve indicated lower survival rates among the adrenal insufficiency children, but the differences were not statistically significant (p = 0.1263). No differences were identified between the adrenal sufficiency and adrenal insufficiency groups in regards to mechanical ventilation time, use of vasoactive drugs, infection type and chronic disease. CONCLUSION: This study determined the frequency of adrenal insufficiency in children with sepsis and its relationship to increased mortality within the first 28 post-admission days. No statistically significant association was found between adrenal insufficiency and mechanical ventilation time or the use of vasoactive drugs.
Abstract
Rev Bras Ter Intensiva. 2008;20(1):57-62
DOI 10.1590/S0103-507X2008000100009
BACKGROUND AND OBJECTIVES: It is important to know the risk factors for extubation failure (EF) in children submitted to cardiac surgery in order to avoid inherent events due to reintubation (airways injury, usage of medications, cardiovascular changes) and because of prolonged ventilatory support (pneumonias, reduction of the ventilatory muscles strength). The objective of this study is to evaluate mechanical ventilation (MV) parameters, ventilatory mechanics [rapid shallow breathing index (RSBI), ventilatory muscles force [the maximum inspiratory pressure (MIP), the maximum expiratory pressure (MEP) and the load/force balance (LFB)] and blood gases before and after extubation in pediatric patients undergoing cardiac surgery. METHODS: Prospective (March 2004 to March 2006) observational cross sectional study, enrolling children submitted to cardiac surgery admitted to an university PICU hospital and considered able to be extubated. With the tracheal tube in situ and maintaining the children spontaneously breathing we evaluate: expiratory minute volume (V E), MIP and MEP. We calculated the RSBI [(RR/VT)/Weight)], LFB [15x [(3xMAP)/MIP] + 0.03 x RSBI-5], the mean airway pressure (MAP) [MAP={(PIP-PEEP)x[Ti/(Te+Ti)]}+PEEP] and the oxygenation index (OI) [OI=(FiO2 x MAP/PaO2)x100]. Arterial blood gas was collected one hour before extubation. If after 48 hours there was no need to reintubate the patient the extubation was considered successful (SE). RESULTS: 59 children were included. EF was observed in 19% (11/59). Median (QI25%-75%) for age, weight, MAP, OI, duration of MV after cardiac surgery (DMV) were respectively, 36 (12-82) months, 12 (8-20) kg, 8 (6-9), 2 (2-5), 1 (1-3) days. Median (QI25-75%) of EF in relation to SE for OI, LFB and DMV were respectively 5(3-8) versus 2(2-4), p = 0.005; [8(6-11) versus 5(4-6), p =0.002 and 3(2-5) versus 1(1-2) days, p = 0.026. Mean ± SD of EF in relation to SE for V E, PaO2 and MIP were respectively 1.7 ± 0.82 versus 3 ± 2.7 mL/kg/min, p = 0.003); 64 ± 34 versus 111 ± 50 mmHg, p = 0.002 and 53 ± 18 versus 78 ± 28 cmH2O; p=0.002. Concerning the risk factors for EF: OI > 2 (area under the ROC 0.74, p = 0.017) and LFB > 4 (area under the ROC 0.80, p = 0.002), achieved a sensibility of 100% and specificity of 80%; MIP < -35 cmH2O (area under the ROC 0.23; p= 0.004) achieved a sensibility of 80% and specificity of 60%. CONCLUSIONS: EF in children submitted to cardiac surgery is related to OI > 2, LFB > 4, DMV > 3 days; V E < 1.7 mL/kg/min, PaO2 < 64 mmHg and MIP < - 53 cmH2O. The kind of cardiac defect, MAP, RSBI and arterial blood gas were not related to EF.