Abstract
Crit Care Sci. 2023;35(4):355-366
DOI 10.5935/2965-2774.20230015-pt
To compare, within a cohort of patients with acute respiratory failure, the phenotypes of patients with and without COVID-19 in the context of the pandemic and evaluate whether COVID-19 is an independent predictor of intensive care unit mortality.
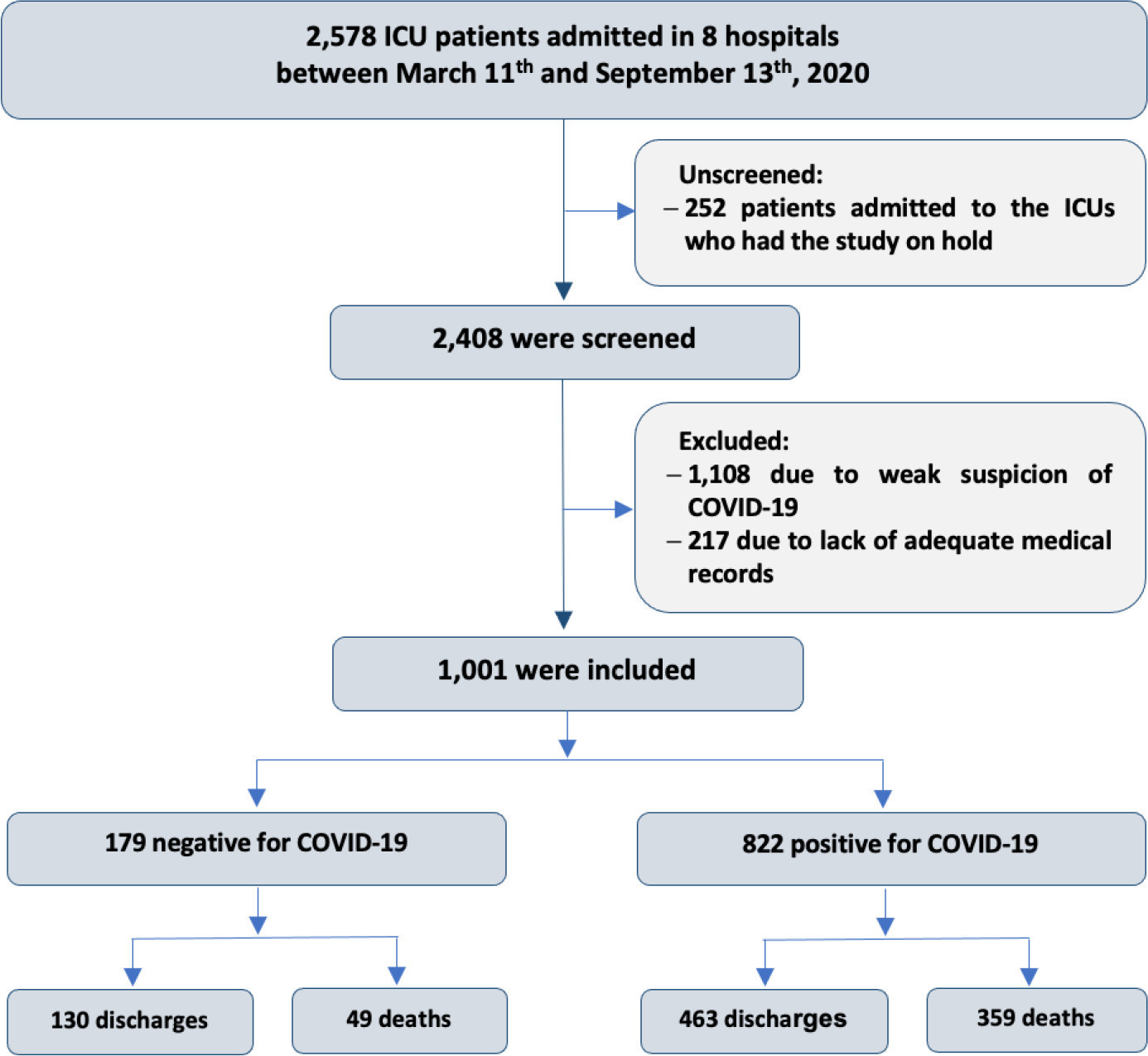
This historical cohort study evaluated 1001 acute respiratory failure patients with suspected COVID-19 admitted to the intensive care unit of 8 hospitals. Patients were classified as COVID-19 cases and non-COVID-19 cases according to real-time polymerase chain reaction results. Data on clinical and demographic characteristics were collected on intensive care unit admission, as well as daily clinical and laboratory data and intensive care unit outcomes.
Although the groups did not differ in terms of APACHE II or SOFA scores at admission, the COVID-19 group had more initial symptoms of fever, myalgia and diarrhea, had a longer duration of symptoms, and had a higher prevalence of obesity. They also had a lower PaO2/FiO2 ratio, lower platelet levels than non-COVID-19 patients, and more metabolic changes, such as higher levels of blood glucose, C-reactive protein, and lactic dehydrogenase. Patients with non-COVID-19 acute respiratory failure had a higher prevalence of chronic obstructive pulmonary disease/asthma and cardiopathy. Patients with COVID-19 stayed in the hospital longer and had more complications, such as acute kidney failure, severe acute respiratory distress syndrome and severe infection. The all-cause mortality rate was also higher in this group (43.7% in the COVID-19 group versus 27.4% in the non-COVID-19 group). The diagnosis of COVID-19 was a predictor of intensive care unit mortality (odds ratio, 2.77; 95%CI, 1.89 - 4.07; p < 0.001), regardless of age or Charlson Comorbidity Index score.
In a prospective cohort of patients admitted with acute respiratory failure, patients with COVID-19 had a clearly different phenotype and a higher mortality than non-COVID-19 patients. This may help to outline more accurate screening and appropriate and timely treatment for these patients.
Abstract
Crit Care Sci. 2023;35(3):243-255
DOI 10.5935/2965-2774.20230136-pt
To update the recommendations to support decisions regarding the pharmacological treatment of patients hospitalized with COVID-19 in Brazil.
Experts, including representatives of the Ministry of Health and methodologists, created this guideline. The method used for the rapid development of guidelines was based on the adoption and/or adaptation of existing international guidelines (GRADE ADOLOPMENT) and supported by the e-COVID-19 RecMap platform. The quality of the evidence and the preparation of the recommendations followed the GRADE method.
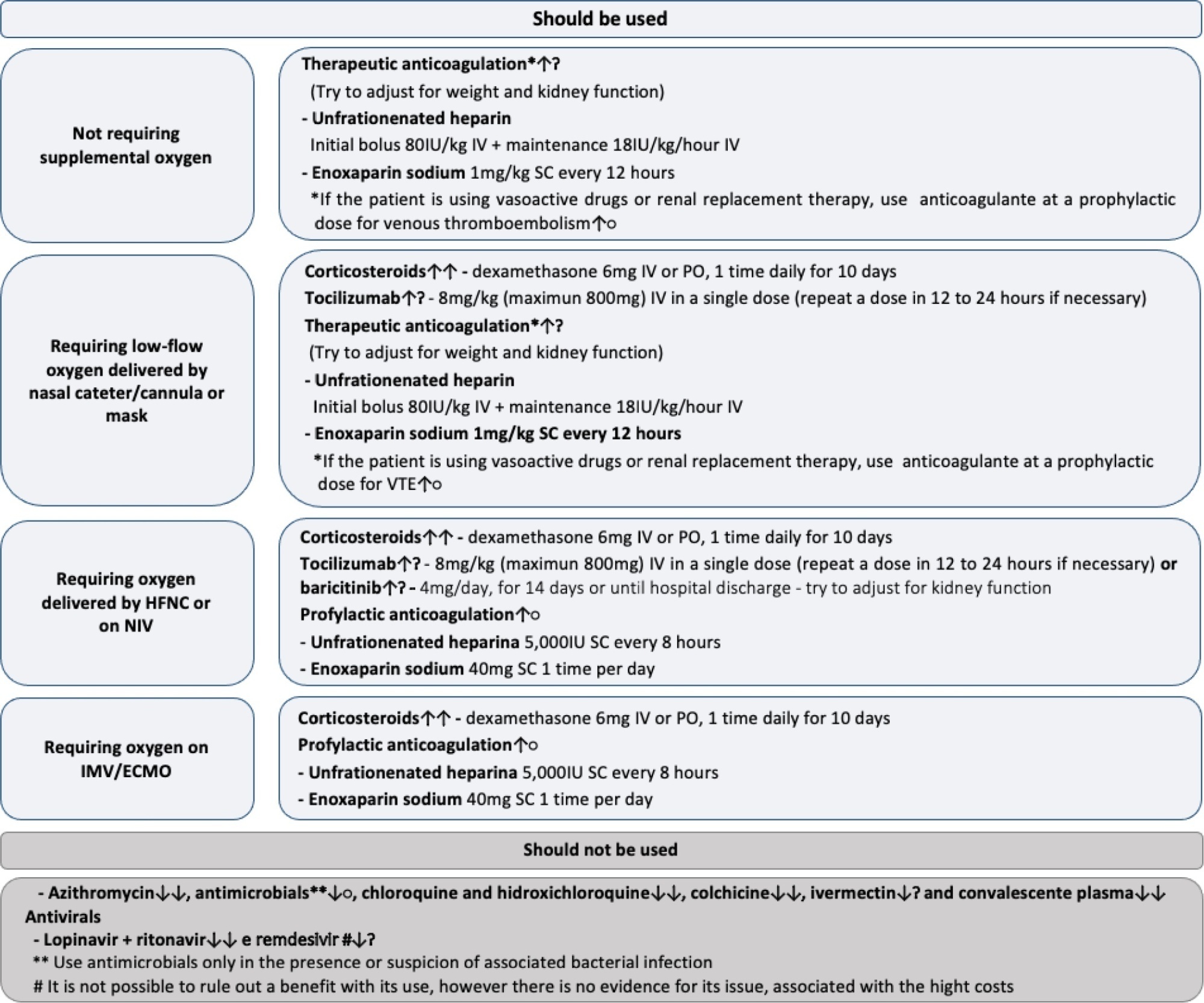
Twenty-one recommendations were generated, including strong recommendations for the use of corticosteroids in patients using supplemental oxygen and conditional recommendations for the use of tocilizumab and baricitinib for patients on supplemental oxygen or on noninvasive ventilation and anticoagulants to prevent thromboembolism. Due to suspension of use authorization, it was not possible to make recommendations regarding the use of casirivimab + imdevimab. Strong recommendations against the use of azithromycin in patients without suspected bacterial infection, hydroxychloroquine, convalescent plasma, colchicine, and lopinavir + ritonavir and conditional recommendations against the use of ivermectin and remdesivir were made.
New recommendations for the treatment of hospitalized patients with COVID-19 were generated, such as those for tocilizumab and baricitinib. Corticosteroids and prophylaxis for thromboembolism are still recommended, the latter with conditional recommendation. Several drugs were considered ineffective and should not be used to provide the best treatment according to the principles of evidence-based medicine and to promote resource economy.
Abstract
Crit Care Sci. 2023;35(3):302-310
DOI 10.5935/2965-2774.20230141-pt
To evaluate the accuracy of the persistent AKI risk index (PARI) in predicting acute kidney injury within 72 hours after admission to the intensive care unit, persistent acute kidney injury, renal replacement therapy, and death within 7 days in patients hospitalized due to acute respiratory failure.
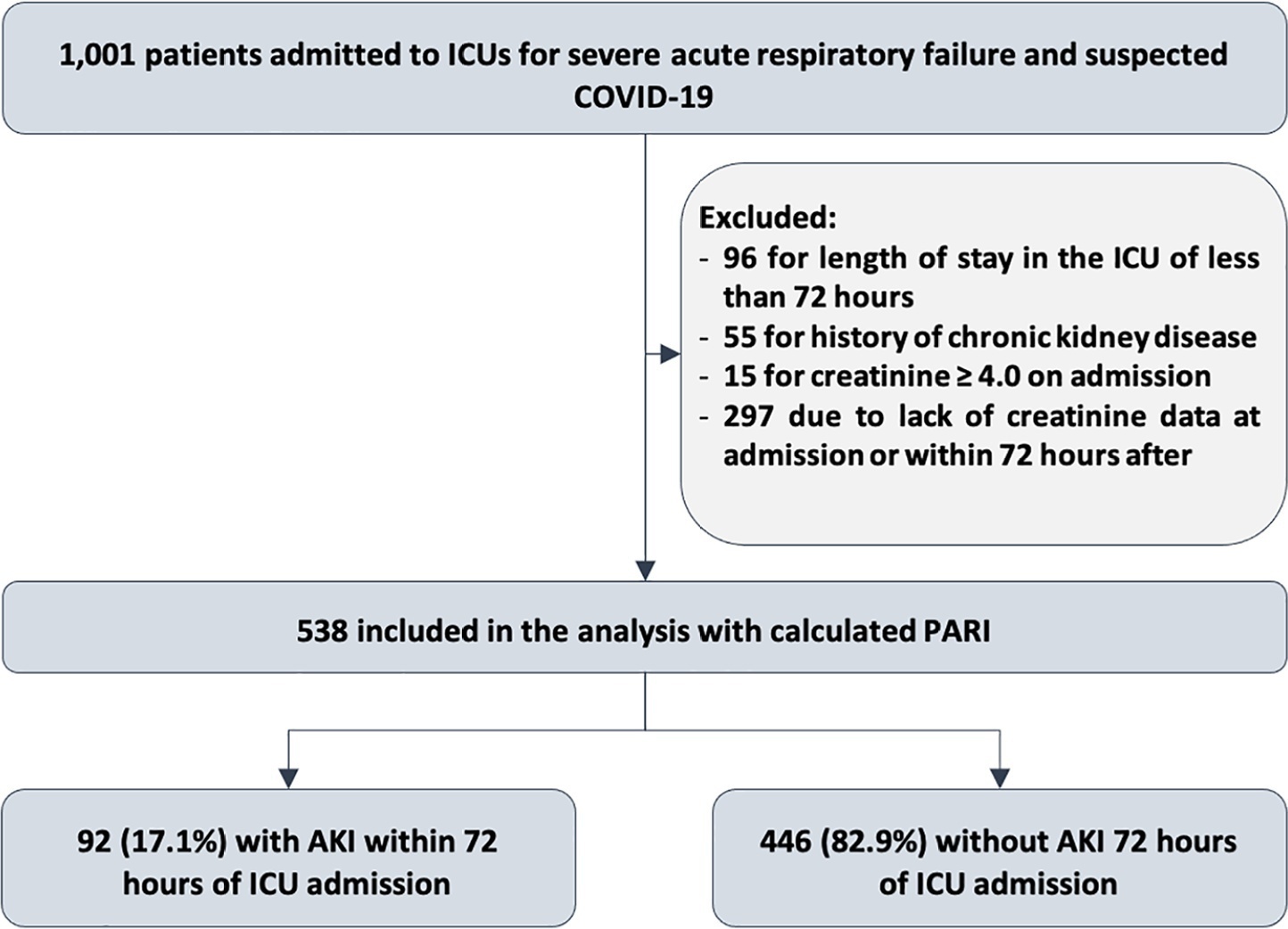
This study was done in a cohort of diagnoses of consecutive adult patients admitted to the intensive care unit of eight hospitals in Curitiba, Brazil, between March and September 2020 due to acute respiratory failure secondary to suspected COVID-19. The COVID-19 diagnosis was confirmed or refuted by RT-PCR for the detection of SARS-CoV-2. The ability of PARI to predict acute kidney injury at 72 hours, persistent acute kidney injury, renal replacement therapy, and death within 7 days was analyzed by ROC curves in comparison to delta creatinine, SOFA, and APACHE II.
Of the 1,001 patients in the cohort, 538 were included in the analysis. The mean age was 62 ± 17 years, 54.8% were men, and the median APACHE II score was 12. At admission, the median SOFA score was 3, and 83.3% had no renal dysfunction. After admission to the intensive care unit, 17.1% had acute kidney injury within 72 hours, and through 7 days, 19.5% had persistent acute kidney injury, 5% underwent renal replacement therapy, and 17.1% died. The PARI had an area under the ROC curve of 0.75 (0.696 - 0.807) for the prediction of acute kidney injury at 72 hours, 0.71 (0.613 - 0.807) for renal replacement therapy, and 0.64 (0.565 - 0.710) for death.
The PARI has acceptable accuracy in predicting acute kidney injury within 72 hours and renal replacement therapy within 7 days of admission to the intensive care unit, but it is not significantly better than the other scores.
Abstract
Crit Care Sci. 2023;35(2):156-162
DOI 10.5935/2965-2774.20230343-pt
To identify risk factors for nonresponse to prone positioning in mechanically ventilated patients with COVID-19-associated severe acute respiratory distress syndrome and refractory hypoxemia in a tertiary care hospital in Colombia.
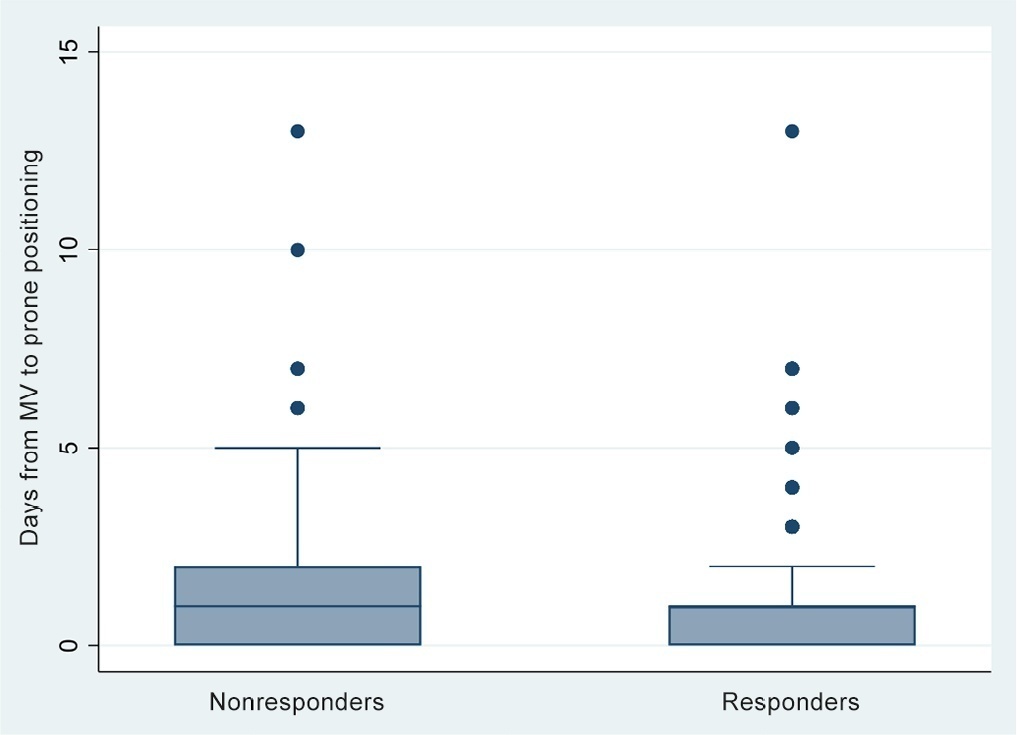
Observational study based on a retrospective cohort of mechanically ventilated patients with severe acute respiratory distress syndrome due to SARS-CoV-2 who underwent prone positioning due to refractory hypoxemia. The study considered an improvement ≥ 20% in the PaO2/FiO2 ratio after the first cycle of 16 hours in the prone position to be a ‘response’. Nonresponding patients were considered cases, and responding patients were controls. We controlled for clinical, laboratory, and radiological variables.
A total of 724 patients were included (58.67 ± 12.37 years, 67.7% males). Of those, 21.9% were nonresponders. Mortality was 54.1% for nonresponders and 31.3% for responders (p < 0.001). Variables associated with nonresponse were time from the start of mechanical ventilation to pronation (OR 1.23; 95%CI 1.10 - 1.41); preintubation PaO2/FiO2 ratio (OR 0.62; 95%CI 0.40 - 0.96); preprone PaO2/FiO2 ratio (OR 1.88. 95%CI 1.22 - 2.94); and radiologic multilobe consolidation (OR 2.12; 95%CI 1.33 - 3.33) or mixed pattern (OR 1.72; 95%CI 1.07 - 2.85) compared with a ground-glass pattern.
This study identified factors associated with nonresponse to prone positioning in patients with refractory hypoxemia and acute respiratory distress syndrome due to SARS-CoV-2 receiving mechanical ventilation. Recognizing such factors helps identify candidates for other rescue strategies, including more extensive prone positioning or extracorporeal membrane oxygenation. Further studies are needed to assess the consistency of these findings in populations with acute respiratory distress syndrome of other etiologies.
Abstract
Crit Care Sci. 2023;35(2):163-167
DOI 10.5935/2965-2774.20230009-pt
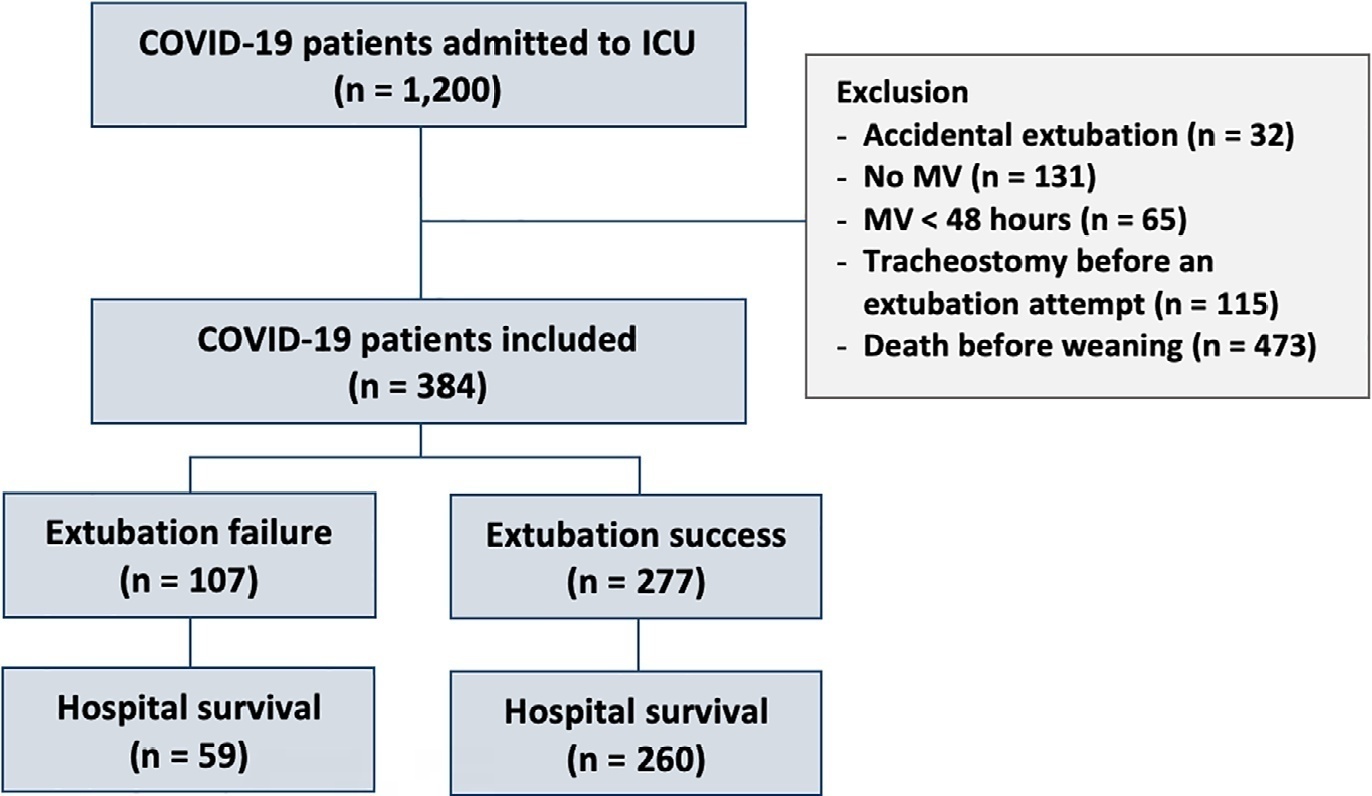
To assess the outcome of extubation in COVID-19 patients and the use of noninvasive ventilation in the weaning process.
This retrospective, observational, single-center study was conducted in COVID-19 patients aged 18 years or older who were admitted to an intensive care unit between April 2020 and December 2021, placed under mechanical ventilation for more than 48 hours and progressed to weaning. Early extubation was defined as extubation without a spontaneous breathing trial and immediate use of noninvasive ventilation after extubation. In patients who underwent a spontaneous breathing trial, noninvasive ventilation could be used as prophylactic ventilatory assistance when started immediately after extubation (prophylactic noninvasive ventilation) or as rescue therapy in cases of postextubation respiratory failure (therapeutic noninvasive ventilation). The primary outcome was extubation failure during the intensive care unit stay.
Three hundred eighty-four extubated patients were included. Extubation failure was observed in 107 (27.9%) patients. Forty-seven (12.2%) patients received prophylactic noninvasive ventilation. In 26 (6.8%) patients, early extubation was performed with immediate use of noninvasive ventilation. Noninvasive ventilation for the management of postextubation respiratory failure was administered to 64 (16.7%) patients.
We found that COVID-19 patients had a high rate of extubation failure. Despite the high risk of extubation failure, we observed low use of prophylactic noninvasive ventilation in these patients.
Abstract
Crit Care Sci. 2023;35(1):19-30
DOI 10.5935/2965-2774.20230203-pt
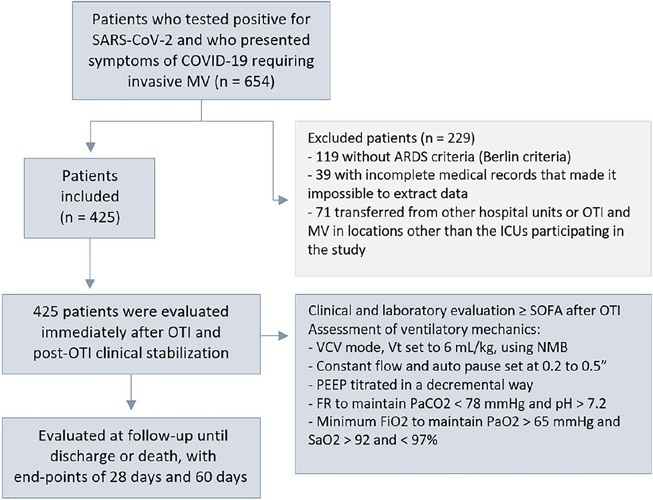
To evaluate the factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19.
This was a retrospective, multicenter cohort study that included 425 mechanically ventilated adult patients with COVID-19 admitted to 4 intensive care units. Clinical data comprising the SOFA score, laboratory data and mechanical characteristics of the respiratory system were collected in a standardized way immediately after the start of invasive mechanical ventilation. The risk factors for death were analyzed using Cox regression to estimate the risk ratios and their respective 95%CIs.
Body mass index (RR 1.17; 95%CI 1.11 - 1.20; p < 0.001), SOFA score (RR 1.39; 95%CI 1.31 - 1.49; p < 0.001) and driving pressure (RR 1.24; 95%CI 1.21 - 1.29; p < 0.001) were considered independent factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19. Respiratory system compliance (RR 0.92; 95%CI 0.90 - 0.93; p < 0.001) was associated with lower mortality. The comparative analysis of the survival curves indicated that patients with respiratory system compliance (< 30mL/cmH2O), a higher SOFA score (> 5 points) and higher driving pressure (> 14cmH2O) were more significantly associated with the outcome of death at 28 days and 60 days.
Patients with a body mass index > 32kg/m2, respiratory system compliance < 30mL/cmH2O, driving pressure > 14cmH2O and SOFA score > 5.8 immediately after the initiation of invasive ventilatory support had worse outcomes, and independent risk factors were associated with higher mortality in this population.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):443-451
DOI 10.5935/0103-507X.20220440-en
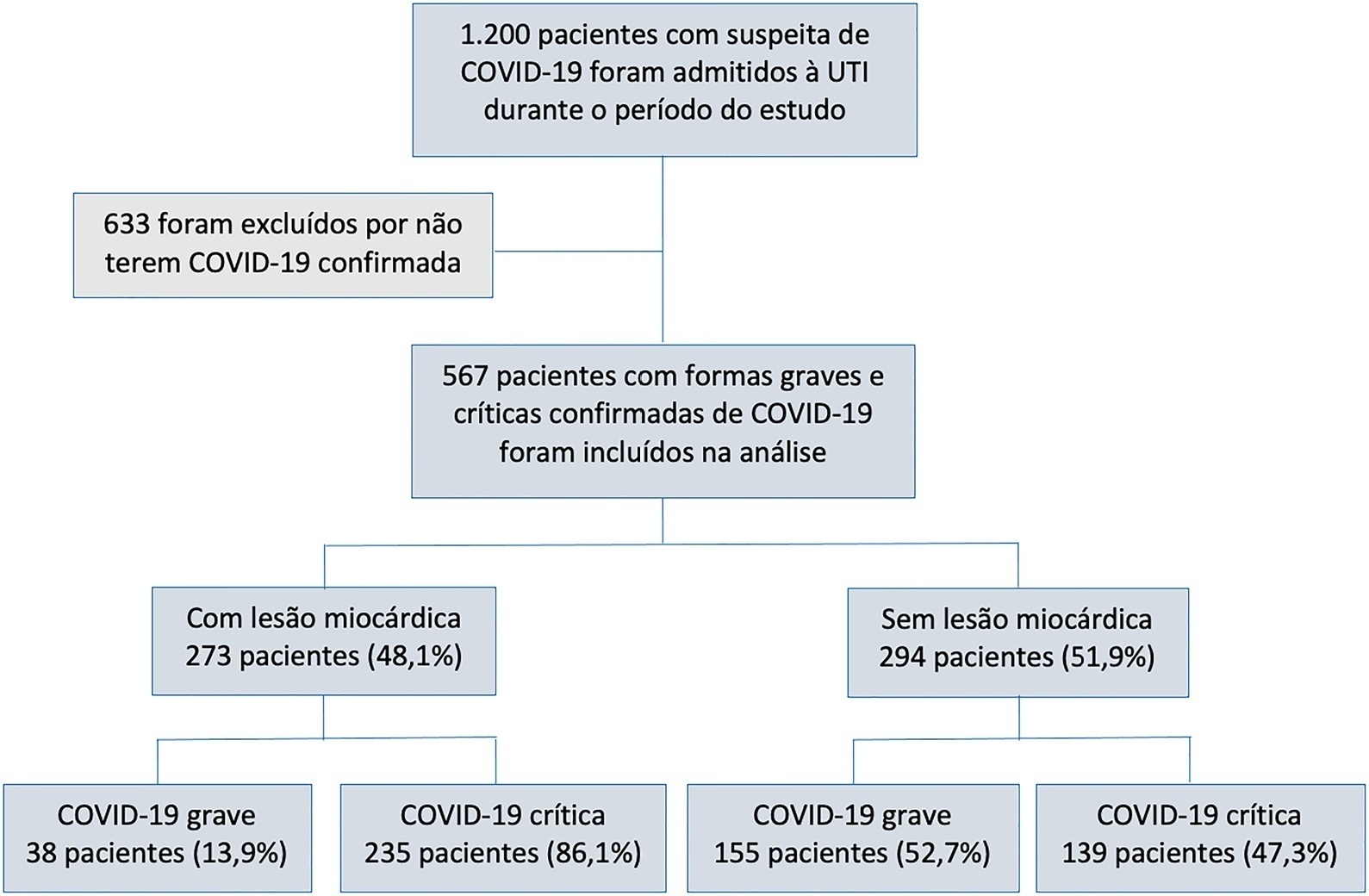
To characterize myocardial injury and cardiovascular complications and their predictors in severe and critical COVID-19 patients admitted to the intensive care unit.
This was an observational cohort study of severe and critical COVID-19 patients admitted to the intensive care unit. Myocardial injury was defined as blood levels of cardiac troponin above the 99th percentile upper reference limit. Cardiovascular events considered were the composite of deep vein thrombosis, pulmonary embolism, stroke, myocardial infarction, acute limb ischemia, mesenteric ischemia, heart failure and arrhythmia. Univariate and multivariate logistic regression or Cox proportional hazard models were used to determine predictors of myocardial injury.
Of 567 patients with severe and critical COVID-19 admitted to the intensive care unit, 273 (48.1%) had myocardial injury. Of the 374 patients with critical COVID-19, 86.1% had myocardial injury, and also showed more organ dysfunction and higher 28-day mortality (56.6% versus 27.1%, p < 0.001). Advanced age, arterial hypertension and immune modulator use were predictors of myocardial injury. Cardiovascular complications occurred in 19.9% of patients with severe and critical COVID-19 admitted to the intensive care unit, with most events occurring in patients with myocardial injury (28.2% versus 12.2%, p < 0.001). The occurrence of an early cardiovascular event during intensive care unit stay was associated with higher 28-day mortality compared with late or no events (57.1% versus 34% versus 41.8%, p = 0.01).
Myocardial injury and cardiovascular complications were commonly found in patients with severe and critical forms of COVID-19 admitted to the intensive care unit, and both were associated with increased mortality in these patients.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):519-523
DOI 10.5935/0103-507X.20220314-en
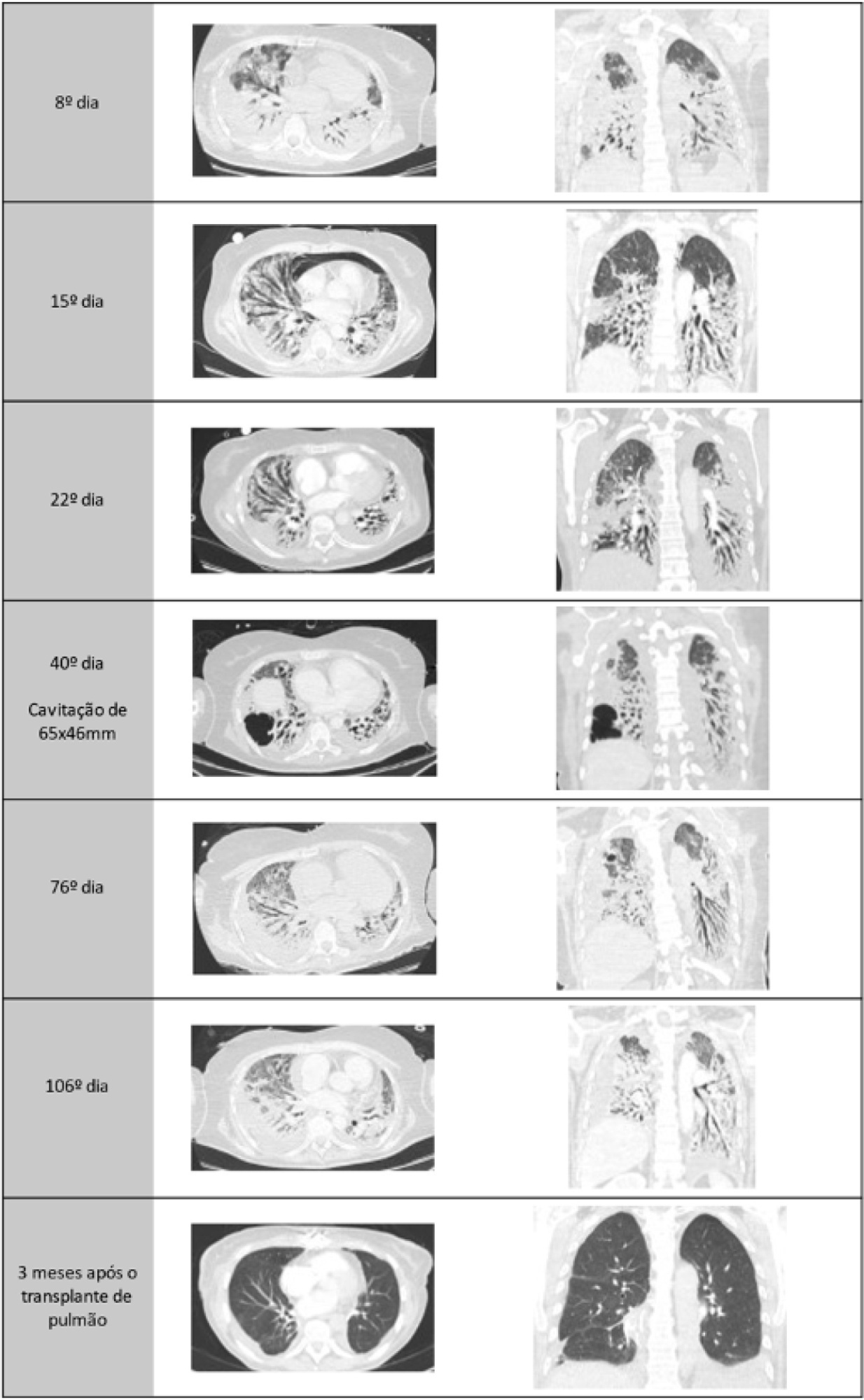
A healthy 55-year-old woman unvaccinated for SARS-CoV-2 was admitted to the hospital with a SARS-CoV-2 infection with rapid clinical deterioration. On the 17th day of disease, she was intubated, and on the 24th day, the patient was referred and admitted to our extracorporeal membrane oxygenation center. Extracorporeal membrane oxygenation support was initially used to enable lung recovery and allow the patient to rehabilitate and improve her physical condition. Despite an adequate physical condition, the lung function was not adequate to discontinue extracorporeal membrane oxygenation, and the patient was considered for lung transplantation. The intensive rehabilitation program was implemented to improve and maintain the physical status throughout all phases. The extracorporeal membrane oxygenation run had several complications that hindered successful rehabilitation: right ventricular failure that required venoarterial-venous extracorporeal membrane oxygenation for 10 days; six nosocomial infections, four with progression to septic shock; and knee hemarthrosis. To reduce the risk of infection, invasive devices (i.e., invasive mechanical ventilation, central venous catheter, and vesical catheter) were removed whenever possible, keeping only those essential for monitoring and care. After 162 days of extracorporeal membrane oxygenation support without other organ dysfunction, bilateral lobar lung transplantation was performed. Physical and respiratory rehabilitation were continued to promote independence in daily life activities. Four months after surgery, the patient was discharged.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) ICU (25) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)