Abstract
Rev Bras Ter Intensiva. 2022;34(4):519-523
DOI 10.5935/0103-507X.20220314-en
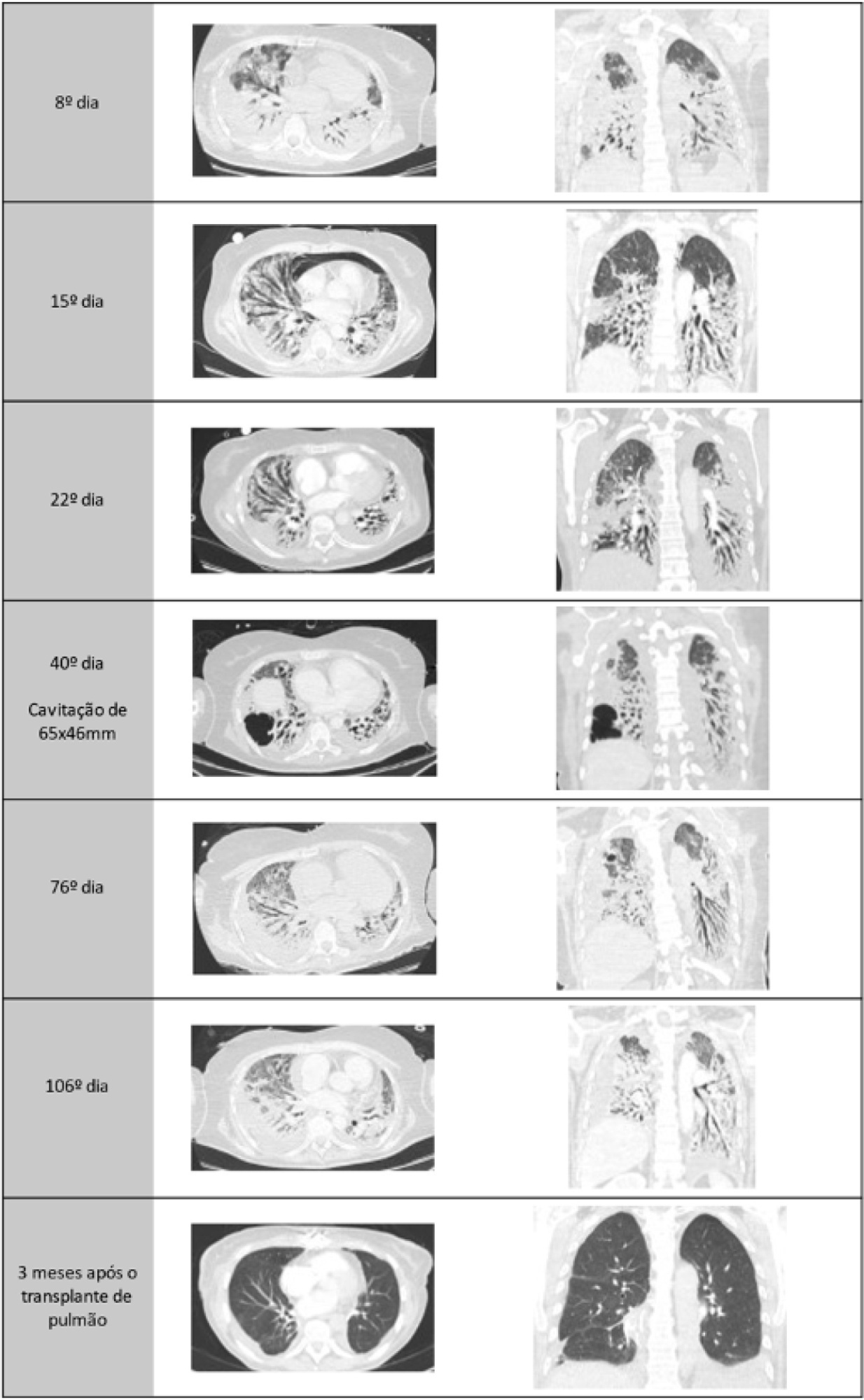
A healthy 55-year-old woman unvaccinated for SARS-CoV-2 was admitted to the hospital with a SARS-CoV-2 infection with rapid clinical deterioration. On the 17th day of disease, she was intubated, and on the 24th day, the patient was referred and admitted to our extracorporeal membrane oxygenation center. Extracorporeal membrane oxygenation support was initially used to enable lung recovery and allow the patient to rehabilitate and improve her physical condition. Despite an adequate physical condition, the lung function was not adequate to discontinue extracorporeal membrane oxygenation, and the patient was considered for lung transplantation. The intensive rehabilitation program was implemented to improve and maintain the physical status throughout all phases. The extracorporeal membrane oxygenation run had several complications that hindered successful rehabilitation: right ventricular failure that required venoarterial-venous extracorporeal membrane oxygenation for 10 days; six nosocomial infections, four with progression to septic shock; and knee hemarthrosis. To reduce the risk of infection, invasive devices (i.e., invasive mechanical ventilation, central venous catheter, and vesical catheter) were removed whenever possible, keeping only those essential for monitoring and care. After 162 days of extracorporeal membrane oxygenation support without other organ dysfunction, bilateral lobar lung transplantation was performed. Physical and respiratory rehabilitation were continued to promote independence in daily life activities. Four months after surgery, the patient was discharged.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):557-564
DOI 10.5935/0103-507X.20210072
To describe health care providers’ knowledge about lung donation and donor lung management.
A descriptive, cross-sectional study based on an anonymous survey was conducted between March and September 2018 among health care professionals registered to Sociedad Argentina de Terapia Intensiva.
Of the 736 respondents, the mean age was 40.5 years (standard deviation 8.9), and 61.3% were female. Sixty percent were physicians, 21.5% were nurses, and 17.9% were physiotherapists. Seventy-eight percent considered themselves appropriately informed about organ procurement, and 79.8% stated that they knew potential organ donor critical care management. The lung donor criteria were answered correctly by 71.3% of the respondents. However, after the donor’s brain death, 51% made no changes to ventilator parameters, 22.9% were not aware of which parameters to reprogram, and 44.5% selected tidal volume of 6 - 8mL/kg and positive end expiratory pressure of 5cmH2O. For 85% of the health care providers, the type of apnea test chosen was disconnection from the ventilator, and only 18.5% used a lung management protocol. The most frequent interventions used in the case of arterial oxygen partial pressure/fractional inspired oxygen < 300 were positive end expiratory pressure titration, closed-circuit endotracheal suctioning, and recruitment maneuvers.
Health care professionals surveyed in Argentina correctly answered most of the questions related to lung donor criteria. However, they lacked detailed knowledge about ventilatory settings, ventilatory strategies, and protocols for lung donors. Educational programs are key to optimizing multiorgan donation and should be focused on protecting the donor lungs to increase the numbers of organs available for transplantation.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):571-577
DOI 10.5935/0103-507X.20200095
To describe the results from the implementation of a respiratory care and mechanical ventilation protocol on potential lung donors who met the conditions for procurement. The secondary objective is to compare the results with historical data.
This was a retrospective, observational study. It included potential donors suitable for procurement of organs who had brain death and were hospitalized in critical care units of the Autonomous City of Buenos Aires from April 2017 to March 2018. Main variables: number of potential lung donors that reached the objective of procurement, rate of lungs procured, and rate of implanted lungs. Values of p < 0.05 were considered significant.
Thirty potential lung donors were included, and 23 (88.5%; 95%CI 69.8 - 97.6) met the oxygenation objective. Twenty potential lung donors donated organs, of whom eight donated lungs, with which four double lung transplants and eight single lung transplants were performed. Seven of 12 lungs were procured and implanted in the preprotocol period, while all 12 were under the protocol (p = 0.38). The implantation rate was 58.3% (7/12) in the historical control period and 100% (12/12) (p = 0.04) in the study period.

Abstract
Rev Bras Ter Intensiva. 2020;32(1):143-148
DOI 10.5935/0103-507X.20200020
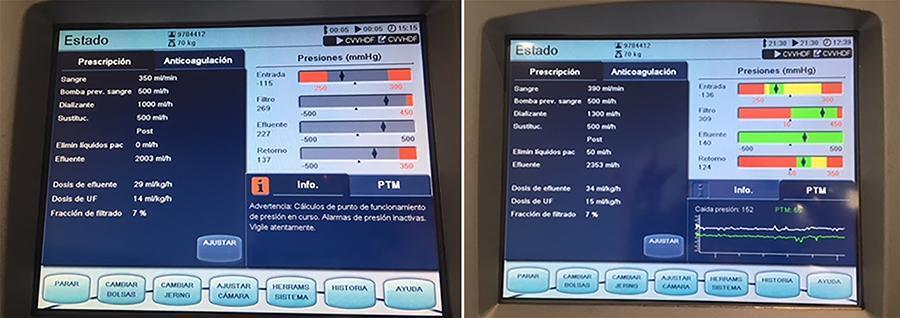
In recent years and due, in part, to technological advances, the use of extracorporeal carbon dioxide removal systems paired with the use of extracorporeal membrane oxygenation has resurfaced. However, studies are lacking that establish its indications and evidence to support its use. These systems efficiently eliminate carbon dioxide in patients with hypercapnic respiratory failure using small-bore cannula, usually double-lumen cannula with a small membrane lung surface area. Currently, we have several systems with different types of membranes and sizes. Pump-driven veno-venous systems generate fewer complications than do arteriovenous systems. Both require systemic anticoagulation. The “lung-kidney” support system, by combining a removal system with hemofiltration, simultaneously eliminates carbon dioxide and performs continuous extrarenal replacement. We describe our initial experience with a combined system for extracorporeal carbon dioxide removal-continuous extrarenal replacement in a lung transplant patients with hypercapnic respiratory failure, barotrauma and associated acute renal failure. The most important technical aspects, the effectiveness of the system for the elimination of carbon dioxide and a review of the literature are described.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):134-140
DOI 10.5935/0103-507X.20150024
The development of the extracorporeal membrane oxygenation in Latin America represents a challenge in this specialty field. The objective of this article was to describe the results of a new extracorporeal membrane oxygenation program in an intensive care unit.
This retrospective cohort study included 22 patients who required extracorporeal membrane oxygenation and were treated from January 2011 to June 2014. The baseline characteristics, indications, duration of the condition, days on mechanical ventilation, days in the intensive care unit, complications, and hospital mortality were evaluated.
Fifteen patients required extracorporeal membrane oxygenation after lung transplantation, and seven patients required oxygenation due to acute respiratory distress. All transplanted patients were weaned from extracorporeal membrane oxygenation with a median duration of 3 days (Interquartile range - IQR: 2 - 5), were on mechanical ventilation for a median of 15.5 days (IQR: 3 - 25), and had an intensive care unit stay of 31.5 days (IQR: 19 - 53) and a median hospital stay of 60 days (IQR: 36 - 89) with 20% mortality. Patients with acute respiratory distress had a median oxygenation membrane duration of 9 days (IQR: 3 - 14), median mechanical ventilation time of 25 days (IQR: 13 - 37), a 31 day stay in therapy (IQR: 11 - 38), a 32 day stay in the hospital (IQR: 11 - 41), and 57% mortality. The main complications were infections (80%), acute kidney failure (43%), bleeding at the surgical site and at the site of cannula placement (22%), plateletopenia (60%), and coagulopathy (30%).
In spite of the steep learning curve, we considered this experience to be satisfactory, with results and complications comparable to those reported in the literature.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)