Abstract
Crit Care Sci. 2024;36:e20240210en
DOI 10.62675/2965-2774.20240210-en
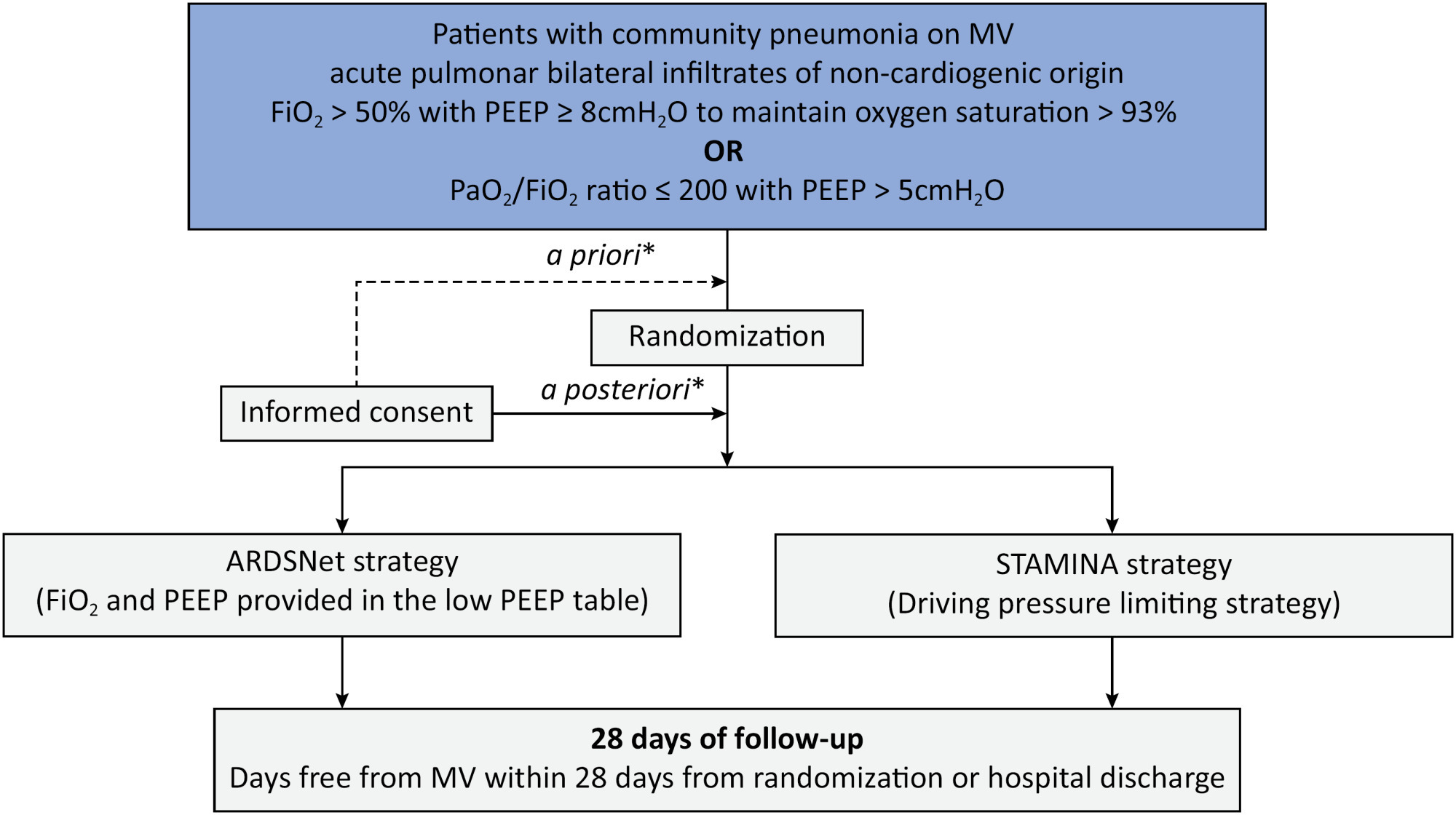
Driving pressure has been suggested to be the main driver of ventilator-induced lung injury and mortality in observational studies of acute respiratory distress syndrome. Whether a driving pressure-limiting strategy can improve clinical outcomes is unclear.
To describe the protocol and statistical analysis plan that will be used to test whether a driving pressure-limiting strategy including positive end-expiratory pressure titration according to the best respiratory compliance and reduction in tidal volume is superior to a standard strategy involving the use of the ARDSNet low-positive end-expiratory pressure table in terms of increasing the number of ventilator-free days in patients with acute respiratory distress syndrome due to community-acquired pneumonia.
The ventilator STrAtegy for coMmunIty acquired pNeumoniA (STAMINA) study is a randomized, multicenter, open-label trial that compares a driving pressure-limiting strategy to the ARDSnet low-positive end-expiratory pressure table in patients with moderate-to-severe acute respiratory distress syndrome due to community-acquired pneumonia admitted to intensive care units. We expect to recruit 500 patients from 20 Brazilian and 2 Colombian intensive care units. They will be randomized to a driving pressure-limiting strategy group or to a standard strategy using the ARDSNet low-positive end-expiratory pressure table. In the driving pressure-limiting strategy group, positive end-expiratory pressure will be titrated according to the best respiratory system compliance.
The primary outcome is the number of ventilator-free days within 28 days. The secondary outcomes are in-hospital and intensive care unit mortality and the need for rescue therapies such as extracorporeal life support, recruitment maneuvers and inhaled nitric oxide.
STAMINA is designed to provide evidence on whether a driving pressure-limiting strategy is superior to the ARDSNet low-positive end-expiratory pressure table strategy for increasing the number of ventilator-free days within 28 days in patients with moderate-to-severe acute respiratory distress syndrome. Here, we describe the rationale, design and status of the trial.
Abstract
Crit Care Sci. 2023;35(2):156-162
DOI 10.5935/2965-2774.20230343-pt
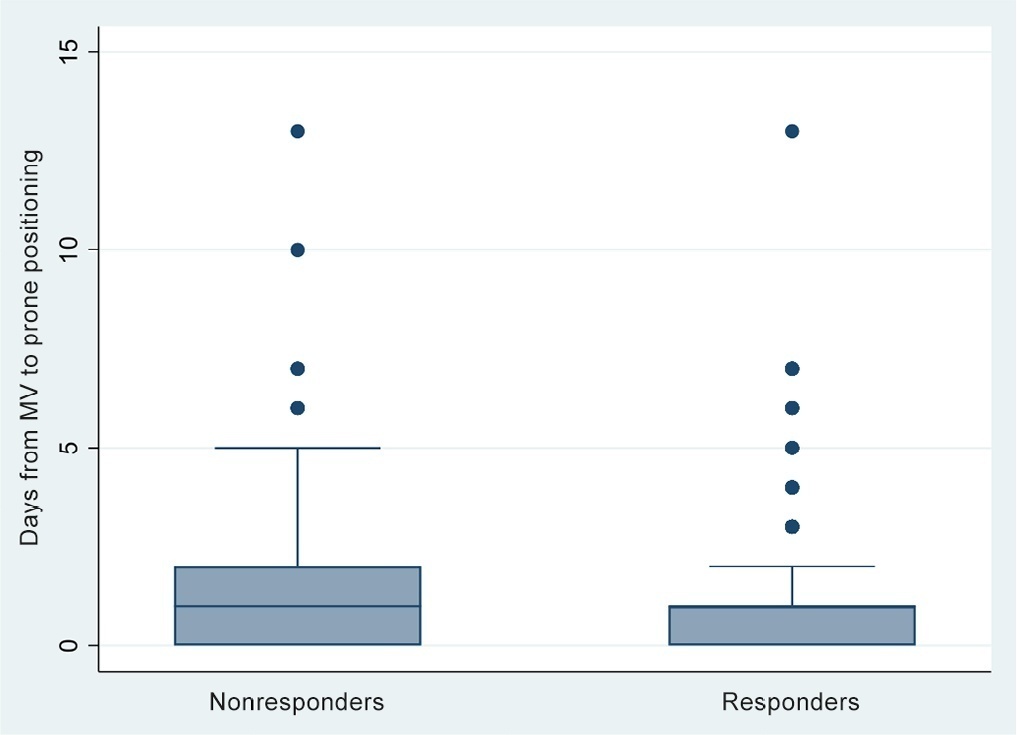
To identify risk factors for nonresponse to prone positioning in mechanically ventilated patients with COVID-19-associated severe acute respiratory distress syndrome and refractory hypoxemia in a tertiary care hospital in Colombia.
Observational study based on a retrospective cohort of mechanically ventilated patients with severe acute respiratory distress syndrome due to SARS-CoV-2 who underwent prone positioning due to refractory hypoxemia. The study considered an improvement ≥ 20% in the PaO2/FiO2 ratio after the first cycle of 16 hours in the prone position to be a ‘response’. Nonresponding patients were considered cases, and responding patients were controls. We controlled for clinical, laboratory, and radiological variables.
A total of 724 patients were included (58.67 ± 12.37 years, 67.7% males). Of those, 21.9% were nonresponders. Mortality was 54.1% for nonresponders and 31.3% for responders (p < 0.001). Variables associated with nonresponse were time from the start of mechanical ventilation to pronation (OR 1.23; 95%CI 1.10 - 1.41); preintubation PaO2/FiO2 ratio (OR 0.62; 95%CI 0.40 - 0.96); preprone PaO2/FiO2 ratio (OR 1.88. 95%CI 1.22 - 2.94); and radiologic multilobe consolidation (OR 2.12; 95%CI 1.33 - 3.33) or mixed pattern (OR 1.72; 95%CI 1.07 - 2.85) compared with a ground-glass pattern.
This study identified factors associated with nonresponse to prone positioning in patients with refractory hypoxemia and acute respiratory distress syndrome due to SARS-CoV-2 receiving mechanical ventilation. Recognizing such factors helps identify candidates for other rescue strategies, including more extensive prone positioning or extracorporeal membrane oxygenation. Further studies are needed to assess the consistency of these findings in populations with acute respiratory distress syndrome of other etiologies.
Abstract
Crit Care Sci. 2023;35(1):19-30
DOI 10.5935/2965-2774.20230203-pt
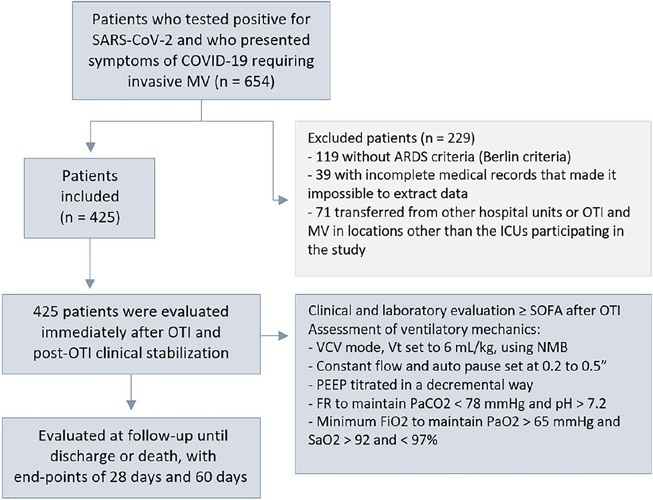
To evaluate the factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19.
This was a retrospective, multicenter cohort study that included 425 mechanically ventilated adult patients with COVID-19 admitted to 4 intensive care units. Clinical data comprising the SOFA score, laboratory data and mechanical characteristics of the respiratory system were collected in a standardized way immediately after the start of invasive mechanical ventilation. The risk factors for death were analyzed using Cox regression to estimate the risk ratios and their respective 95%CIs.
Body mass index (RR 1.17; 95%CI 1.11 - 1.20; p < 0.001), SOFA score (RR 1.39; 95%CI 1.31 - 1.49; p < 0.001) and driving pressure (RR 1.24; 95%CI 1.21 - 1.29; p < 0.001) were considered independent factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19. Respiratory system compliance (RR 0.92; 95%CI 0.90 - 0.93; p < 0.001) was associated with lower mortality. The comparative analysis of the survival curves indicated that patients with respiratory system compliance (< 30mL/cmH2O), a higher SOFA score (> 5 points) and higher driving pressure (> 14cmH2O) were more significantly associated with the outcome of death at 28 days and 60 days.
Patients with a body mass index > 32kg/m2, respiratory system compliance < 30mL/cmH2O, driving pressure > 14cmH2O and SOFA score > 5.8 immediately after the initiation of invasive ventilatory support had worse outcomes, and independent risk factors were associated with higher mortality in this population.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):519-523
DOI 10.5935/0103-507X.20220314-en
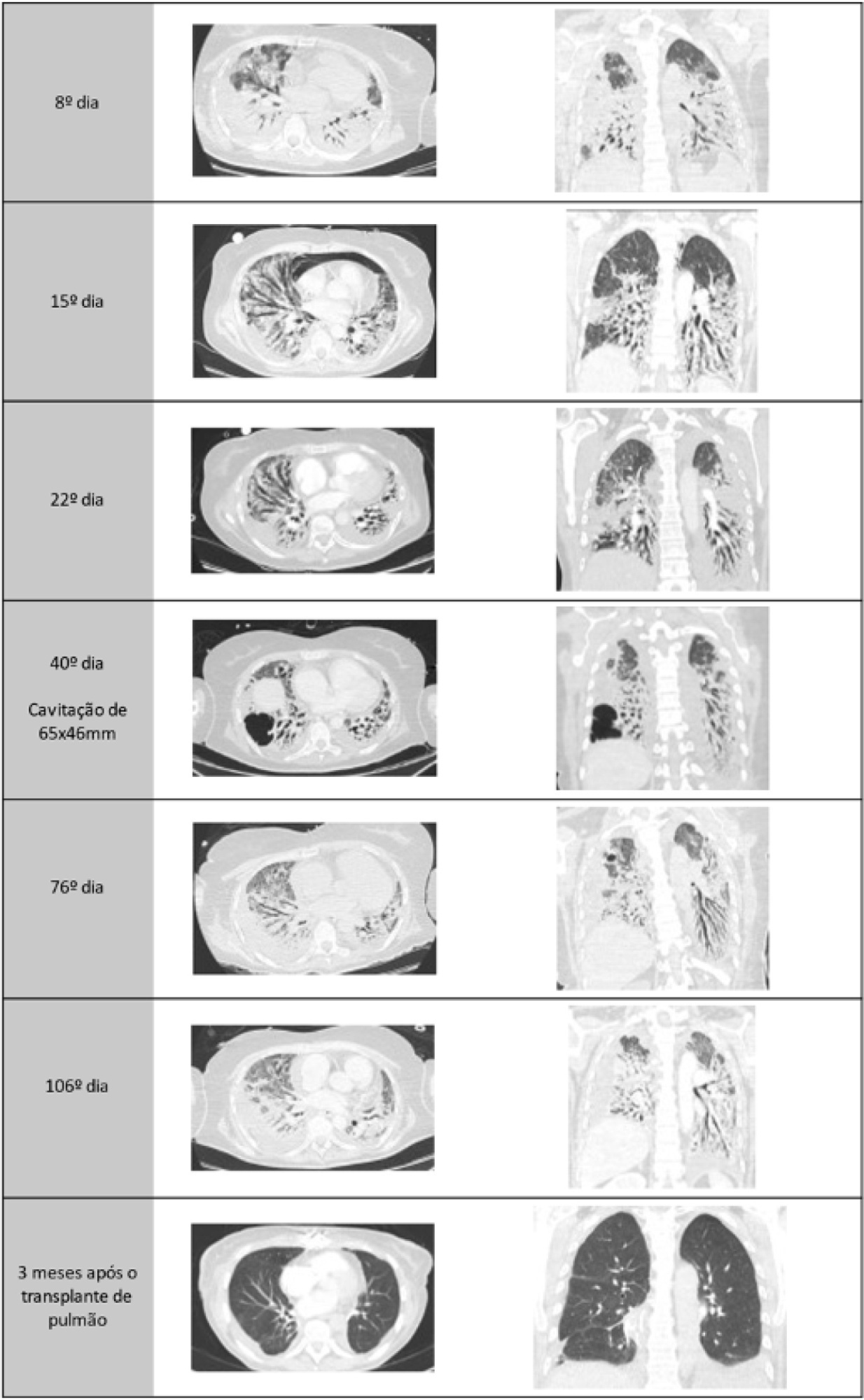
A healthy 55-year-old woman unvaccinated for SARS-CoV-2 was admitted to the hospital with a SARS-CoV-2 infection with rapid clinical deterioration. On the 17th day of disease, she was intubated, and on the 24th day, the patient was referred and admitted to our extracorporeal membrane oxygenation center. Extracorporeal membrane oxygenation support was initially used to enable lung recovery and allow the patient to rehabilitate and improve her physical condition. Despite an adequate physical condition, the lung function was not adequate to discontinue extracorporeal membrane oxygenation, and the patient was considered for lung transplantation. The intensive rehabilitation program was implemented to improve and maintain the physical status throughout all phases. The extracorporeal membrane oxygenation run had several complications that hindered successful rehabilitation: right ventricular failure that required venoarterial-venous extracorporeal membrane oxygenation for 10 days; six nosocomial infections, four with progression to septic shock; and knee hemarthrosis. To reduce the risk of infection, invasive devices (i.e., invasive mechanical ventilation, central venous catheter, and vesical catheter) were removed whenever possible, keeping only those essential for monitoring and care. After 162 days of extracorporeal membrane oxygenation support without other organ dysfunction, bilateral lobar lung transplantation was performed. Physical and respiratory rehabilitation were continued to promote independence in daily life activities. Four months after surgery, the patient was discharged.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):335-341
DOI 10.5935/0103-507X.20220040-en
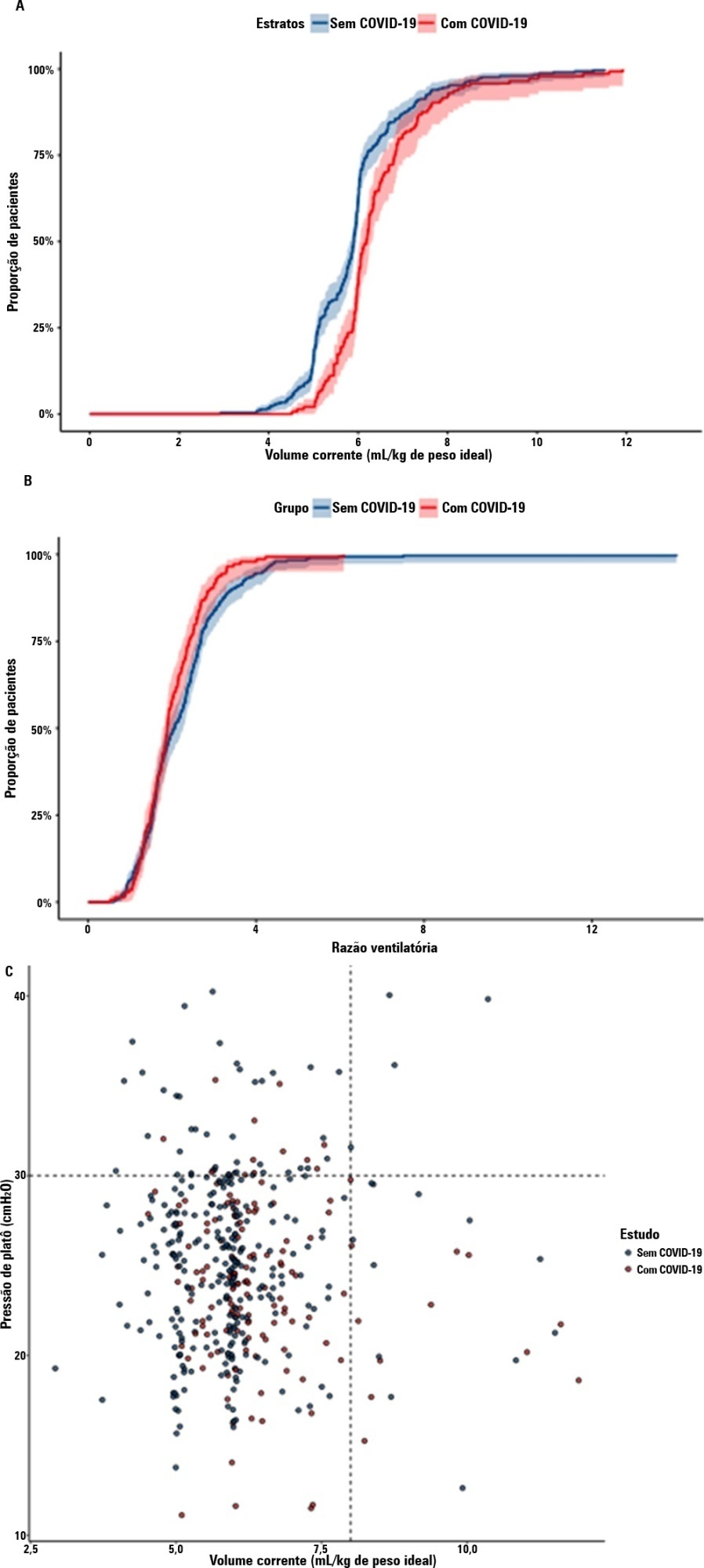
To compare the lung mechanics and outcomes between COVID-19-associated acute respiratory distress syndrome and non-COVID-19-associated acute respiratory distress syndrome.
We combined data from two randomized trials in acute respiratory distress syndrome, one including only COVID-19 patients and the other including only patients without COVID-19, to determine whether COVID-19-associated acute respiratory distress syndrome is associated with higher 28-day mortality than non-COVID-19 acute respiratory distress syndrome and to examine the differences in lung mechanics between these two types of acute respiratory distress syndrome.
A total of 299 patients with COVID-19-associated acute respiratory distress syndrome and 1,010 patients with non-COVID-19-associated acute respiratory distress syndrome were included in the main analysis. The results showed that non-COVID-19 patients used higher positive end-expiratory pressure (12.5cmH2O; SD 3.2 versus 11.7cmH2O SD 2.8; p < 0.001), were ventilated with lower tidal volumes (5.8mL/kg; SD 1.0 versus 6.5mL/kg; SD 1.2; p < 0.001) and had lower static respiratory compliance adjusted for ideal body weight (0.5mL/cmH2O/kg; SD 0.3 versus 0.6mL/cmH2O/kg; SD 0.3; p = 0.01). There was no difference between groups in 28-day mortality (52.3% versus 58.9%; p = 0.52) or mechanical ventilation duration in the first 28 days among survivors (13 [IQR 5 - 22] versus 12 [IQR 6 - 26], p = 0.46).
This analysis showed that patients with non-COVID-19-associated acute respiratory distress syndrome have different lung mechanics but similar outcomes to COVID-19-associated acute respiratory distress syndrome patients. After propensity score matching, there was no difference in lung mechanics or outcomes between groups.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):342-350
DOI 10.5935/0103-507X.20220229-en
To evaluate whether critical SARS-CoV-2 infection is more frequently associated with signs of corticospinal tract dysfunction and other neurological signs, symptoms, and syndromes, than other infectious pathogens.
This was a prospective cohort study with consecutive inclusion of patients admitted to intensive care units due to primary infectious acute respiratory distress syndrome requiring invasive mechanical ventilation > 48 hours. Eligible patients were randomly assigned to three investigators for clinical evaluation, which encompassed the examination of signs of corticospinal tract dysfunction. Clinical data, including other neurological complications and possible predictors, were independently obtained from clinical records.
We consecutively included 54 patients with acute respiratory distress syndrome, 27 due to SARS-CoV-2 and 27 due to other infectious pathogens. The groups were comparable in most characteristics. COVID-19 patients presented a significantly higher risk of neurological complications (RR = 1.98; 95%CI 1.23 - 3.26). Signs of corticospinal tract dysfunction tended to be more prevalent in COVID-19 patients (RR = 1.62; 95%CI 0.72 - 3.44).
Our study is the first comparative analysis between SARS-CoV-2 and other infectious pathogens, in an intensive care unit setting, assessing neurological dysfunction. We report a significantly higher risk of neurological dysfunction among COVID-19 patients. As such, we suggest systematic screening for neurological complications in severe COVID-19 patients.
Abstract
Rev Bras Ter Intensiva. 2022;34(1):185-196
DOI 10.5935/0103-507X.20220013-en
Although the PaO 2/FiO 2 derived from arterial blood gas analysis remains the gold standard for the diagnosis of acute respiratory failure, the SpO2/FiO2 has been investigated as a potential substitute. The current narrative review presents the state of the preclinical and clinical literature on the SpO2/FiO2 as a possible substitute for PaO2/FiO2 and for use as a diagnostic and prognostic marker; provides an overview of pulse oximetry and its limitations, and assesses the utility of SpO2/ FiO2 as a surrogate for PaO2/FiO2 in COVID-19 patients. Overall, 49 studies comparing SpO2/FiO2 and PaO2/FiO2 were found according to a minimal search strategy. Most were conducted on neonates, some were conducted on adults with acute respiratory distress syndrome, and a few were conducted in other clinical scenarios (including a very few on COVID-19 patients). There is some evidence that the SpO2/ FiO2 criteria can be a surrogate for PaO2/FiO2 in different clinical scenarios. This is reinforced by the fact that unnecessary invasive procedures should be avoided in patients with acute respiratory failure. It is undeniable that pulse oximeters are becoming increasingly widespread and can provide costless monitoring. Hence, replacing PaO2/FiO2 with SpO2/FiO2may allow resourcelimited facilities to objectively diagnose acute respiratory failure.
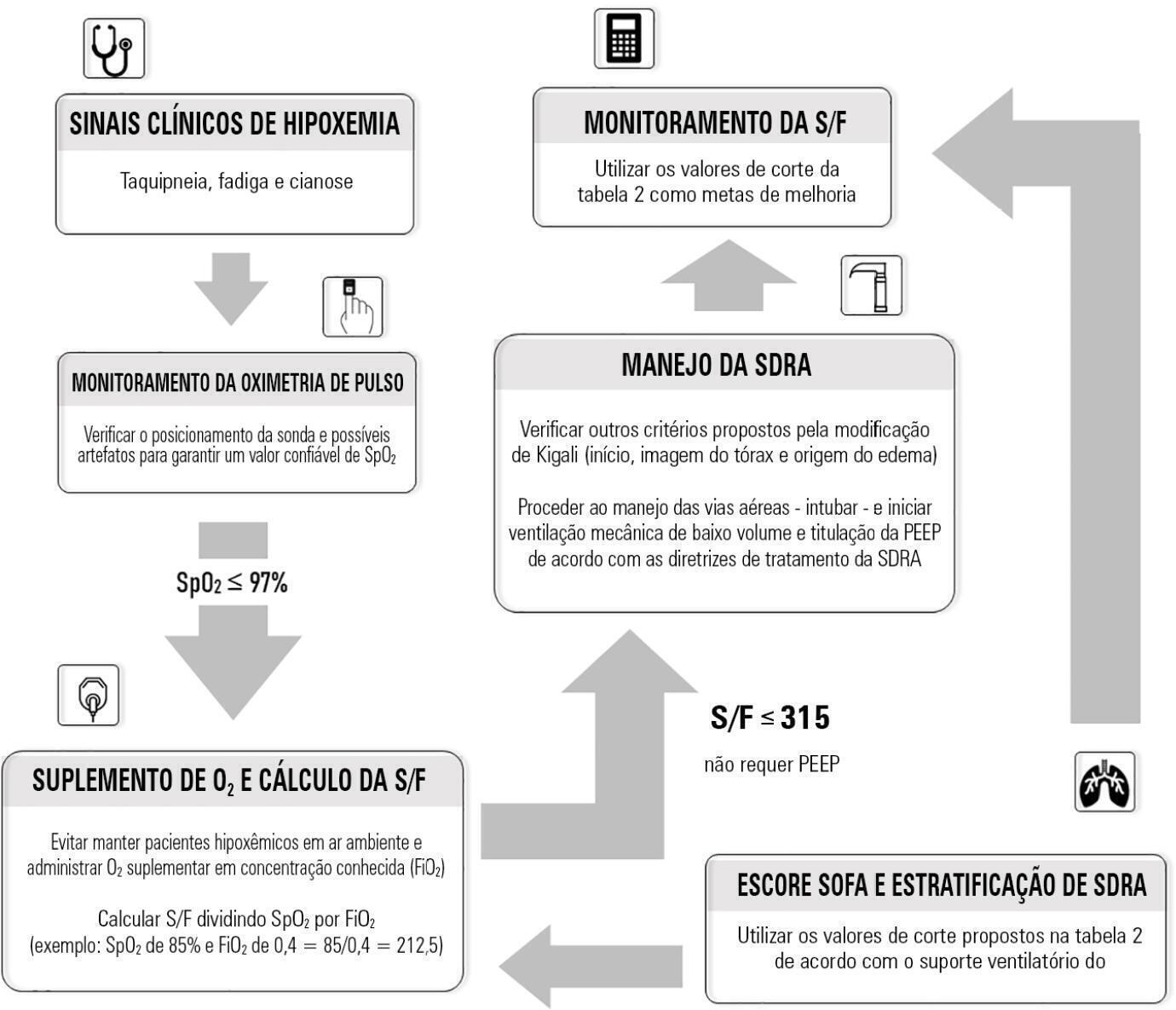
Abstract
Rev Bras Ter Intensiva. 2021;33(4):537-543
DOI 10.5935/0103-507X.20210081
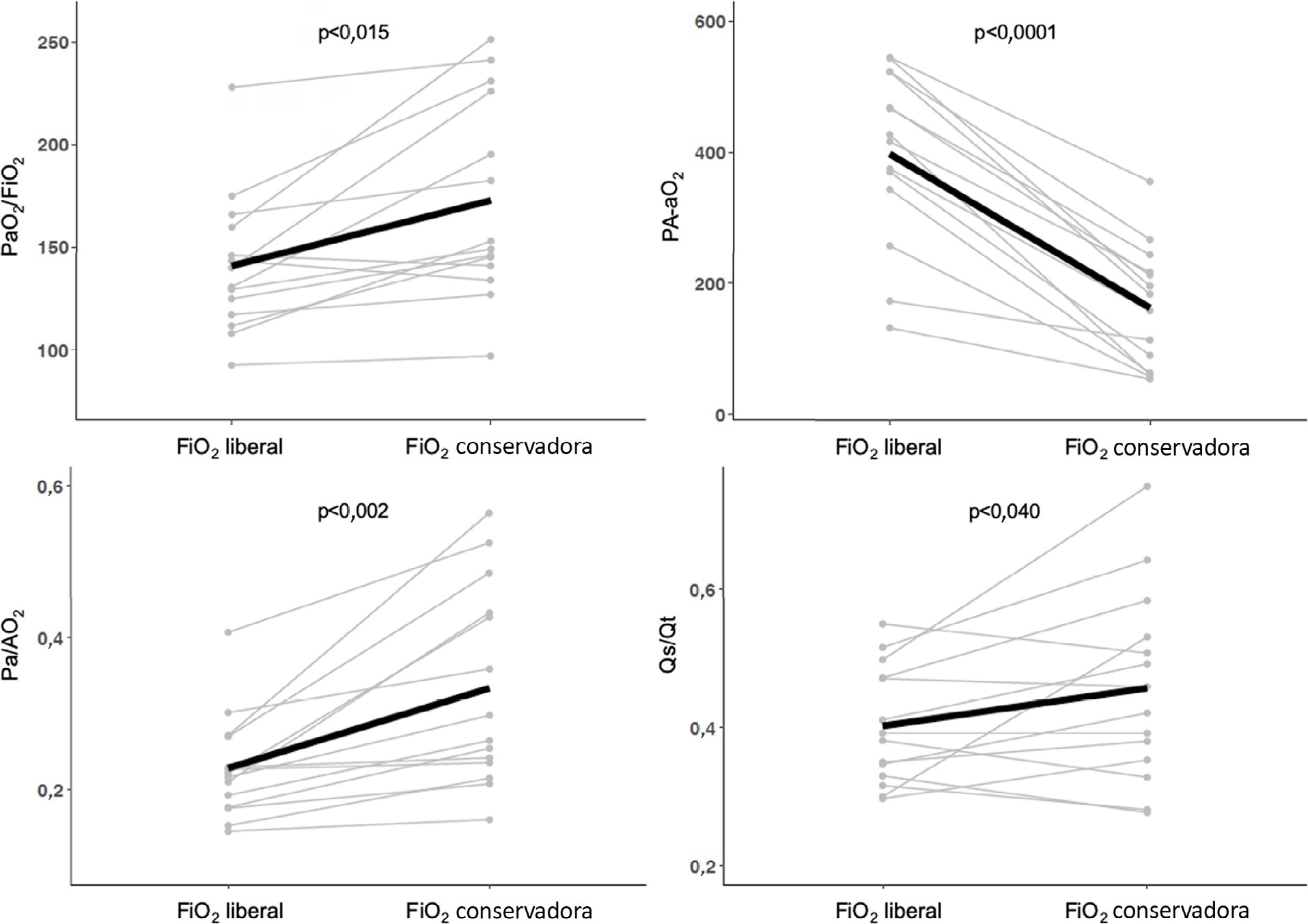
To compare gas exchange indices behavior by using liberal versus conservative oxygenation targets in patients with moderate to severe acute respiratory distress syndrome secondary to COVID-19 under invasive mechanical ventilation. We also assessed the influence of high FiO2 on respiratory system mechanics.
We prospectively included consecutive patients aged over 18 years old with a diagnosis of COVID-19 and moderate-severe acute respiratory distress syndrome. For each patient, we randomly applied two FiO2 protocols to achieve SpO2 88% - 92% or 96%. We assessed oxygenation indices and respiratory system mechanics.
We enrolled 15 patients. All the oxygenation indices were significantly affected by the FiO2 strategy (p < 0.05) selected. The PaO2/FiO2 deteriorated, PA-aO2 increased and Pa/AO2 decreased significantly when using FiO2 to achieve SpO2 96%. Conversely, the functional shunt fraction was reduced. Respiratory mechanics were not affected by the FiO2 strategy.
A strategy aimed at liberal oxygenation targets significantly deteriorated gas exchange indices, except for functional shunt, in COVID-19-related acute respiratory distress syndrome. The respiratory system mechanics were not altered by the FiO2 strategy.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)