Abstract
Crit Care Sci. 2024;36:e20240176en
DOI 10.62675/2965-2774.20240176-en
To systematically review the effect of the prone position on endotracheal intubation and mortality in nonintubated COVID-19 patients with acute respiratory distress syndrome.
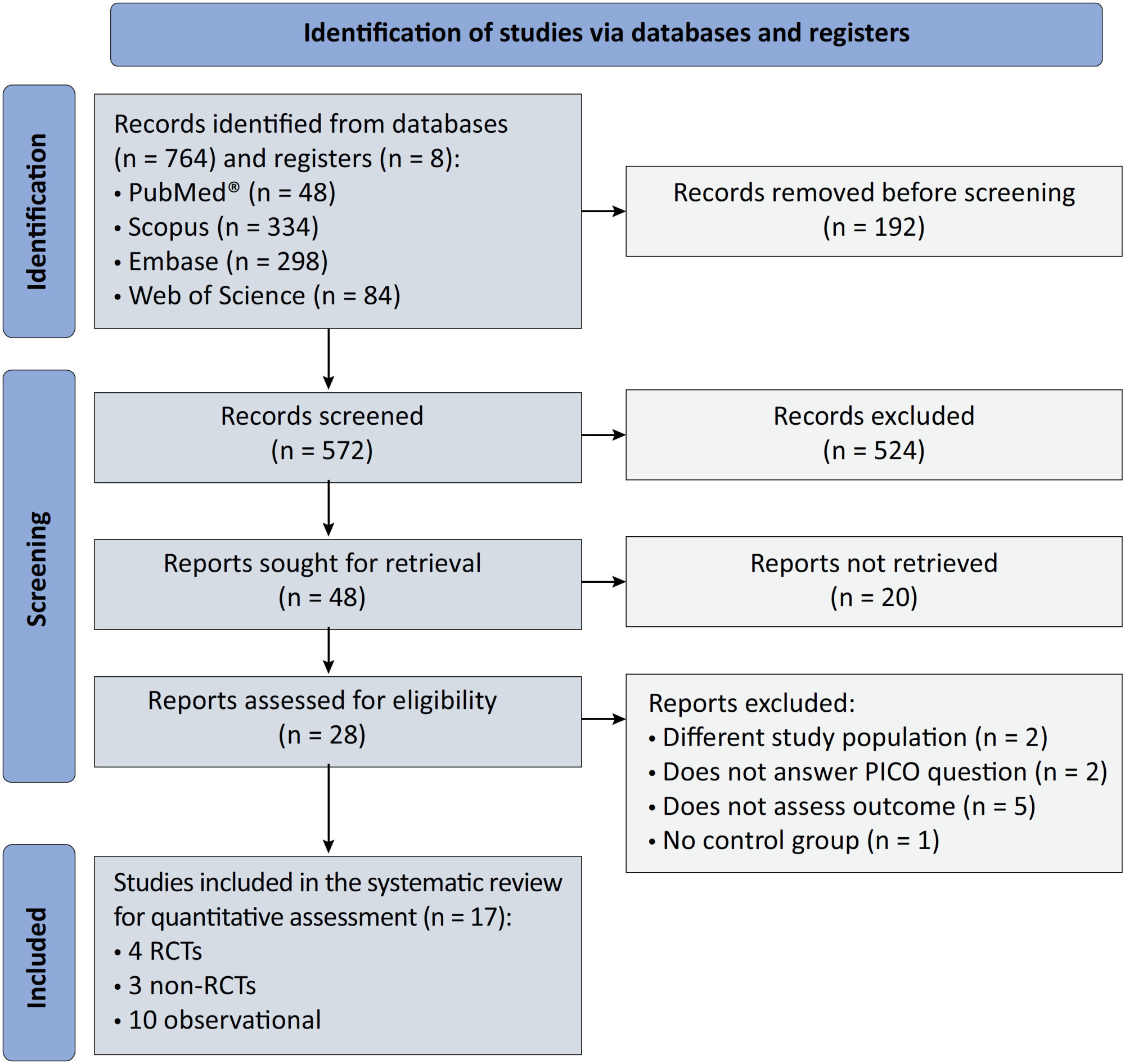
We registered the protocol (CRD42021286711) and searched for four databases and gray literature from inception to December 31, 2022. We included observational studies and clinical trials. There was no limit by date or the language of publication. We excluded case reports, case series, studies not available in full text, and those studies that included children < 18-years-old.
We included ten observational studies, eight clinical trials, 3,969 patients, 1,120 endotracheal intubation events, and 843 deaths. All of the studies had a low risk of bias (Newcastle-Ottawa Scale and Risk of Bias 2 tools). We found that the conscious prone position decreased the odds of endotracheal intubation by 44% (OR 0.56; 95%CI 0.40 - 0.78) and mortality by 43% (OR 0.57; 95%CI 0.39 - 0.84) in nonintubated COVID-19 patients with acute respiratory distress syndrome. This protective effect on endotracheal intubation and mortality was more robust in those who spent > 8 hours/day in the conscious prone position (OR 0.43; 95%CI 0.26 - 0.72 and OR 0.38; 95%CI 0.24 - 0.60, respectively). The certainty of the evidence according to the GRADE criteria was moderate.
The conscious prone position decreased the odds of endotracheal intubation and mortality, especially when patients spent over 8 hours/day in the conscious prone position and treatment in the intensive care unit. However, our results should be cautiously interpreted due to limitations in evaluating randomized clinical trials, nonrandomized clinical trials and observational studies. However, despite systematic reviews with meta-analyses of randomized clinical trials, we must keep in mind that these studies remain heterogeneous from a clinical and methodological point of view.
Abstract
Crit Care Sci. 2023;35(2):156-162
DOI 10.5935/2965-2774.20230343-pt
To identify risk factors for nonresponse to prone positioning in mechanically ventilated patients with COVID-19-associated severe acute respiratory distress syndrome and refractory hypoxemia in a tertiary care hospital in Colombia.
Observational study based on a retrospective cohort of mechanically ventilated patients with severe acute respiratory distress syndrome due to SARS-CoV-2 who underwent prone positioning due to refractory hypoxemia. The study considered an improvement ≥ 20% in the PaO2/FiO2 ratio after the first cycle of 16 hours in the prone position to be a ‘response’. Nonresponding patients were considered cases, and responding patients were controls. We controlled for clinical, laboratory, and radiological variables.
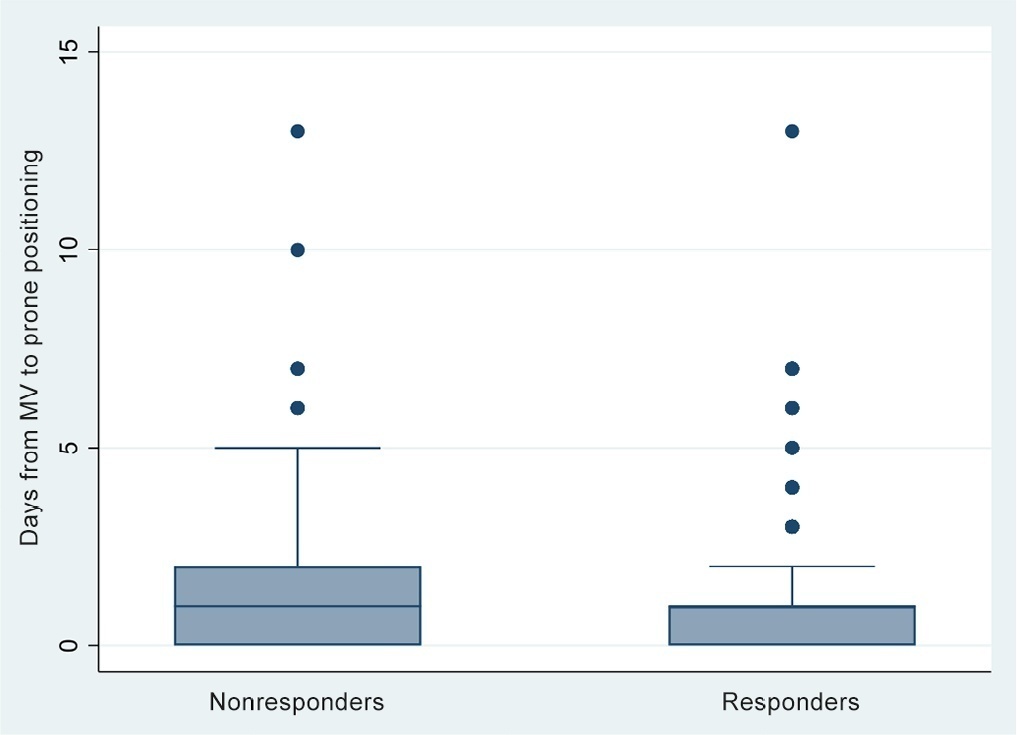
A total of 724 patients were included (58.67 ± 12.37 years, 67.7% males). Of those, 21.9% were nonresponders. Mortality was 54.1% for nonresponders and 31.3% for responders (p < 0.001). Variables associated with nonresponse were time from the start of mechanical ventilation to pronation (OR 1.23; 95%CI 1.10 - 1.41); preintubation PaO2/FiO2 ratio (OR 0.62; 95%CI 0.40 - 0.96); preprone PaO2/FiO2 ratio (OR 1.88. 95%CI 1.22 - 2.94); and radiologic multilobe consolidation (OR 2.12; 95%CI 1.33 - 3.33) or mixed pattern (OR 1.72; 95%CI 1.07 - 2.85) compared with a ground-glass pattern.
This study identified factors associated with nonresponse to prone positioning in patients with refractory hypoxemia and acute respiratory distress syndrome due to SARS-CoV-2 receiving mechanical ventilation. Recognizing such factors helps identify candidates for other rescue strategies, including more extensive prone positioning or extracorporeal membrane oxygenation. Further studies are needed to assess the consistency of these findings in populations with acute respiratory distress syndrome of other etiologies.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):133-142
DOI 10.5935/0103-507X.20200019
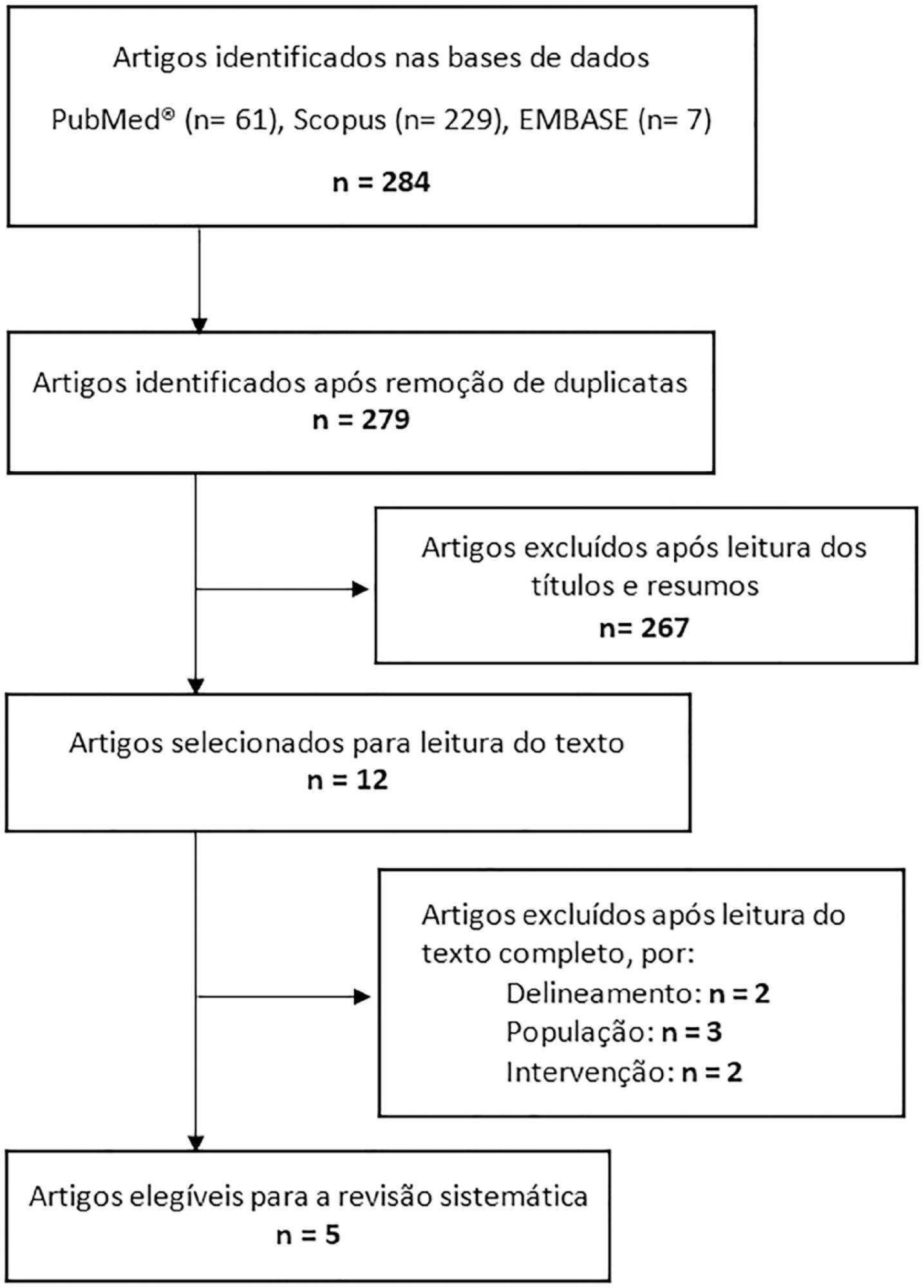
This systematic review of longitudinal studies aimed to evaluate the effect of enteral feeding of critically ill adult and pediatric patients in the prone position on gastric residual volume and other clinical outcomes. A literature search was conducted in the databases PubMed, Scopus and Embase using terms related to population and intervention. Two independent reviewers analyzed the titles and abstracts, and data collection was performed using a standardized form. Discrepancies were resolved by a third reviewer. The methodological quality of the studies was evaluated considering the potential for systematic errors, and the data were qualitatively analyzed. Four studies with adult patients and one with preterm patients were included. The gastric residual volume was evaluated as the main outcome: three studies did not show differences in the gastric residual volume between the prone and supine positions (p > 0.05), while one study showed a higher gastric residual volume during enteral feeding in the prone position (27.6mL versus 10.6mL; p < 0.05), and another group observed a greater gastric residual volume in the supine position (reduction of the gastric residual volume by 23.3% in the supine position versus 43.9% in the prone position; p < 0.01). Two studies evaluated the frequency of vomiting; one study found that it was higher in the prone position (30 versus 26 episodes; p < 0.001), while the other study found no significant difference (p > 0.05). The incidence of aspiration pneumonia and death were evaluated in one study, with no difference between groups (p > 0.05). The literature on the administration of enteral feeding in the prone position in critically ill patients is sparse and of limited quality, and the results regarding gastric residual volume are contradictory. Observational studies with appropriate sample sizes should be conducted to support conclusions on the subject.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):296-302
DOI 10.5935/0103-507X.20190054
Evaluate the physiological and autonomic nervous system responses of premature newborns to body position and noise in the neonatal intensive care unit.
A quasi-experimental study. The autonomic nervous system of newborns was evaluated based on heart rate variability when the newborns were exposed to environmental noise and placed in different positions: supine without support, supine with manual restraint and prone.
Fifty premature newborns were evaluated (gestational age: 32.6 ± 2.3 weeks; weight: 1816 ± 493g; and Brazelton sleep/awake level: 3 to 4). A positive correlation was found between environmental noise and sympathetic activity (R = 0.27, p = 0.04). The mean environmental noise was 53 ± 14dB. The heart rate was higher in the supine position than in the manual restraint and prone positions (148.7 ± 21.6, 141.9 ± 16 and 144 ± 13, respectively) (p = 0.001). Sympathetic activity, represented by a low frequency index, was higher in the supine position (p < 0.05) than in the other positions, and parasympathetic activity (high frequency, root mean square of the sum of differences between normal adjacent mean R-R interval and percentage of adjacent iRR that differed by more than 50ms) was higher in the prone position (p < 0.05) than in the other positions. The complexity of the autonomic adjustments (approximate entropy and sample entropy) was lower in the supine position than in the other positions.
The prone position and manual restraint position increased both parasympathetic activity and the complexity of autonomic adjustments in comparison to the supine position, even in the presence of higher environmental noise than the recommended level, which tends to increase sympathetic activity.

Abstract
Rev Bras Ter Intensiva. 2019;31(1):106-110
DOI 10.5935/0103-507X.20190015
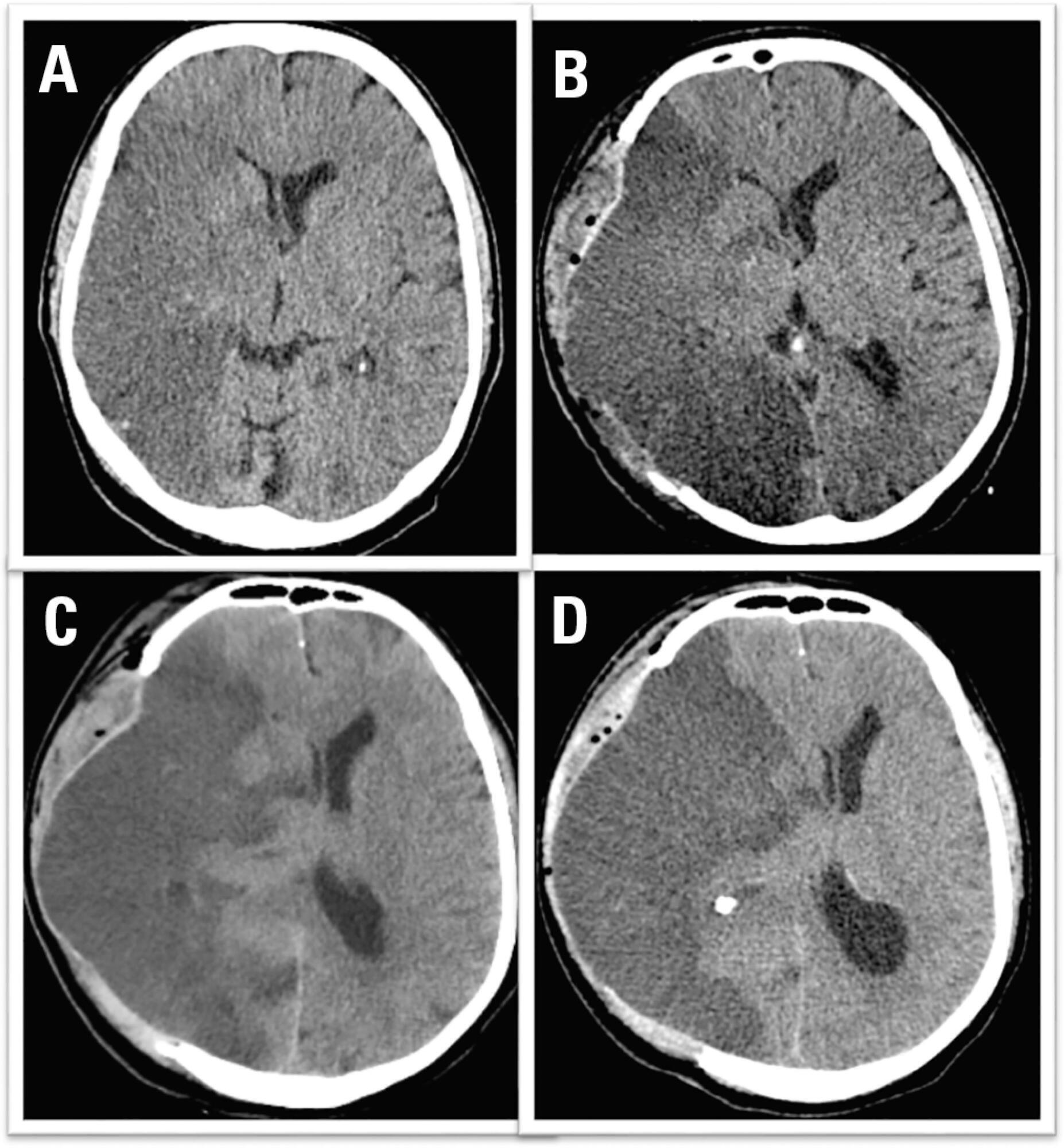
We report the case of a patient in whom brain death was suspected and associated with atelectasis and moderate to severe hypoxemia even though the patient was subjected to protective ventilation, a closed tracheal suction system, positive end-expiratory pressure, and recruitment maneuvers. Faced with the failure to obtain an adequate partial pressure of oxygen for the apnea test, we elected to place the patient in a prone position, use higher positive end-expiratory pressure, perform a new recruitment maneuver, and ventilate with a higher tidal volume (8mL/kg) without exceeding the plateau pressure of 30cmH2O. The apnea test was performed with the patient in a prone position, with continuous positive airway pressure coupled with a T-piece. The delay in diagnosis was 10 hours, and organ donation was not possible due to circulatory arrest. This report demonstrates the difficulties in obtaining higher levels of the partial pressure of oxygen for the apnea test. The delays in the diagnosis of brain death and in the organ donation process are discussed, as well as potential strategies to optimize the partial pressure of oxygen to perform the apnea test according to the current recommendations.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):452-462
DOI 10.5935/0103-507X.20160066
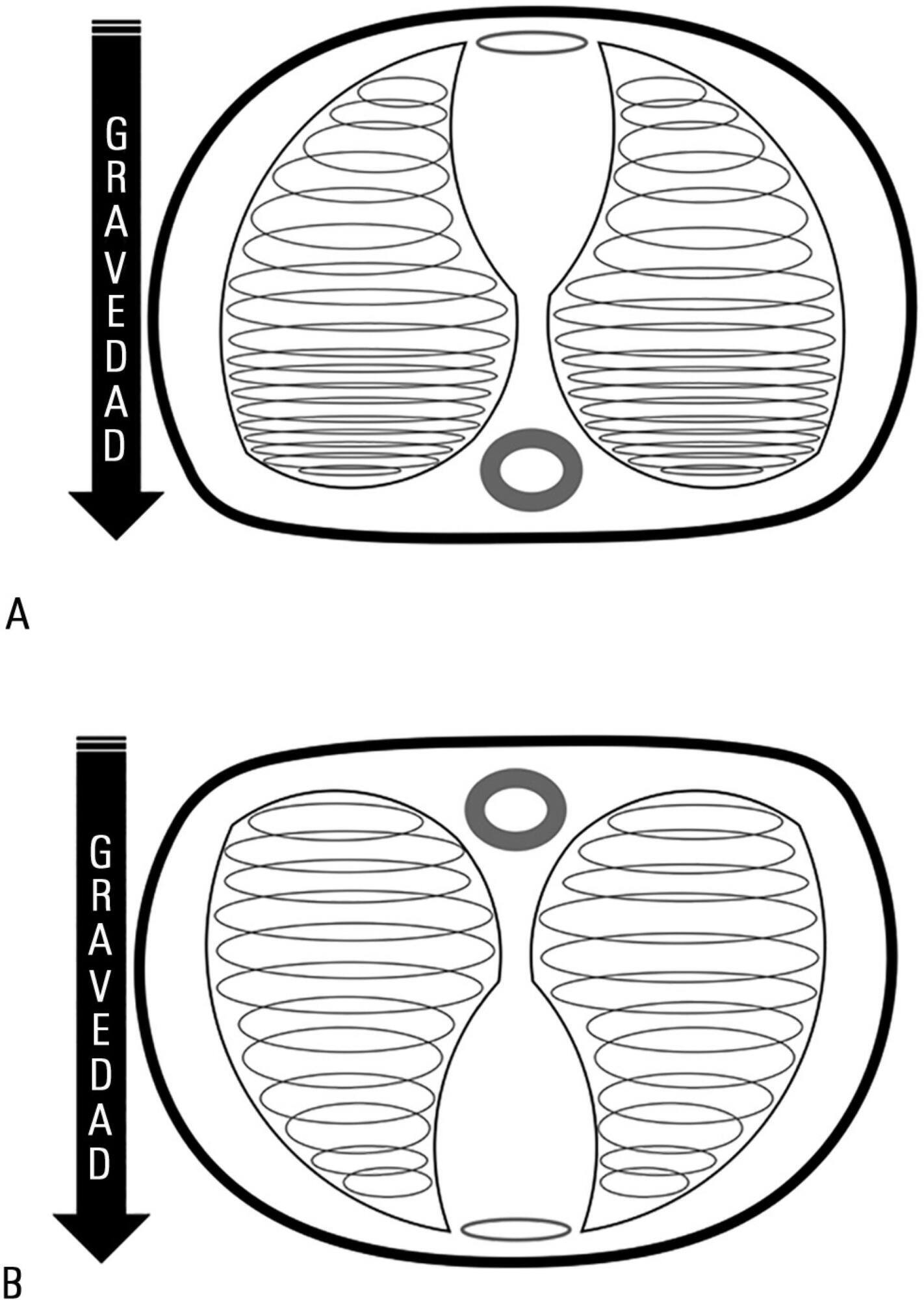
Acute respiratory distress syndrome occupies a great deal of attention in intensive care units. Despite ample knowledge of the physiopathology of this syndrome, the focus in intensive care units consists mostly of life-supporting treatment and avoidance of the side effects of invasive treatments. Although great advances in mechanical ventilation have occurred in the past 20 years, with a significant impact on mortality, the incidence continues to be high. Patients with acute respiratory distress syndrome, especially the most severe cases, often present with refractory hypoxemia due to shunt, which can require additional treatments beyond mechanical ventilation, among which is mechanical ventilation in the prone position. This method, first recommended to improve oxygenation in 1974, can be easily implemented in any intensive care unit with trained personnel.
Prone position has extremely robust bibliographic support. Various randomized clinical studies have demonstrated the effect of prone decubitus on the oxygenation of patients with acute respiratory distress syndrome measured in terms of the PaO2/FiO2 ratio, including its effects on increasing patient survival.
The members of the Respiratory Therapists Committee of the Sociedad Argentina de Terapia Intensiva performed a narrative review with the objective of discovering the available evidence related to the implementation of prone position, changes produced in the respiratory system due to the application of this maneuver, and its impact on mortality. Finally, guidelines are suggested for decision-making.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98) Septic shock (25)