You searched for:"Eduardo Tobar"
We found (5) results for your search.-
Review Articles
Cognitive stimulation and occupational therapy for delirium prevention
Rev Bras Ter Intensiva. 2017;29(2):248-252
Abstract
Review ArticlesCognitive stimulation and occupational therapy for delirium prevention
Rev Bras Ter Intensiva. 2017;29(2):248-252
DOI 10.5935/0103-507X.20170034
Views0See moreABSTRACT
Delirium is a relevant condition in critically ill patients with long-term impacts on mortality, cognitive and functional status and quality of life. Despite the progress in its diagnosis, prevention and management during the last years, its impact persists being relevant, so new preventive and therapeutic strategies need to be explored. Among non-pharmacologic preventive strategies, recent reports suggest a role for occupational therapy through a series of interventions that may impact the development of delirium. The aim of this review is to evaluate the studies evaluating the role of occupational therapy in the prevention of delirium in critically ill patient populations, and suggests perspectives to future research in this area.
-
Original Articles
Fiber optic bronchoscopy-assisted percutaneous tracheostomy: a decade of experience at a university hospital
Rev Bras Ter Intensiva. 2015;27(2):119-124
Abstract
Original ArticlesFiber optic bronchoscopy-assisted percutaneous tracheostomy: a decade of experience at a university hospital
Rev Bras Ter Intensiva. 2015;27(2):119-124
DOI 10.5935/0103-507X.20150022
Views0See moreABSTRACT
Objective:
To evaluate the efficacy and safety of percutaneous tracheostomy by means of single-step dilation with fiber optic bronchoscopy assistance in critical care patients under mechanical ventilation.
Methods:
Between the years 2004 and 2014, 512 patients with indication of tracheostomy according to clinical criteria, were prospectively and consecutively included in our study. One-third of them were high-risk patients. Demographic variables, APACHE II score, and days on mechanical ventilation prior to percutaneous tracheostomy were recorded. The efficacy of the procedure was evaluated according to an execution success rate and based on the necessity of switching to an open surgical technique. Safety was evaluated according to post-operative and operative complication rates.
Results:
The mean age of the group was 64 ± 18 years (203 women and 309 males). The mean APACHE II score was 21 ± 3. Patients remained an average of 11 ± 3 days on mechanical ventilation before percutaneous tracheostomy was performed. All procedures were successfully completed without the need to switch to an open surgical technique. Eighteen patients (3.5%) presented procedure complications. Five patients experienced transient desaturation, 4 presented low blood pressure related to sedation, and 9 presented minor bleeding, but none required a transfusion. No serious complications or deaths associated with the procedure were recorded. Eleven patients (2.1%) presented post-operative complications. Seven presented minor and transitory bleeding of the percutaneous tracheostomy stoma, 2 suffered displacement of the tracheostomy cannula, and 2 developed a superficial infection of the stoma.
Conclusion:
Percutaneous tracheostomy using the single-step dilation technique with fiber optic bronchoscopy assistance seems to be effective and safe in critically ill patients under mechanical ventilation when performed by experienced intensive care specialists using a standardized procedure.
-
Original Article
Delirium in intensive care unit patients under noninvasive ventilation: a multinational survey
Rev Bras Ter Intensiva. 2015;27(4):360-368
Abstract
Original ArticleDelirium in intensive care unit patients under noninvasive ventilation: a multinational survey
Rev Bras Ter Intensiva. 2015;27(4):360-368
DOI 10.5935/0103-507X.20150061
Views0ABSTRACT
Objective:
To conduct a multinational survey of intensive care unit professionals to determine the practices on delirium assessment and management, in addition to their perceptions and attitudes toward the evaluation and impact of delirium in patients requiring noninvasive ventilation.
Methods:
An electronic questionnaire was created to evaluate the profiles of the respondents and their related intensive care units, the systematic delirium assessment and management and the respondents’ perceptions and attitudes regarding delirium in patients requiring noninvasive ventilation. The questionnaire was distributed to the cooperative network for research of the Associação de Medicina Intensiva Brasileira (AMIB-Net) mailing list and to researchers in different centers in Latin America and Europe.
Results:
Four hundred thirty-six questionnaires were available for analysis; the majority of the questionnaires were from Brazil (61.9%), followed by Turkey (8.7%) and Italy (4.8%). Approximately 61% of the respondents reported no delirium assessment in the intensive care unit, and 31% evaluated delirium in patients under noninvasive ventilation. The Confusion Assessment Method for the intensive care unit was the most reported validated diagnostic tool (66.9%). Concerning the indication of noninvasive ventilation in patients already presenting with delirium, 16.3% of respondents never allow the use of noninvasive ventilation in this clinical context.
Conclusion:
This survey provides data that strongly reemphasizes poor efforts toward delirium assessment and management in the intensive care unit setting, especially regarding patients requiring noninvasive ventilation.
Keywords:Attitude of health personnelCritical careDeliriumDiagnostic techniques, neurologicalNoninvasive ventilationQuestionnairesSee more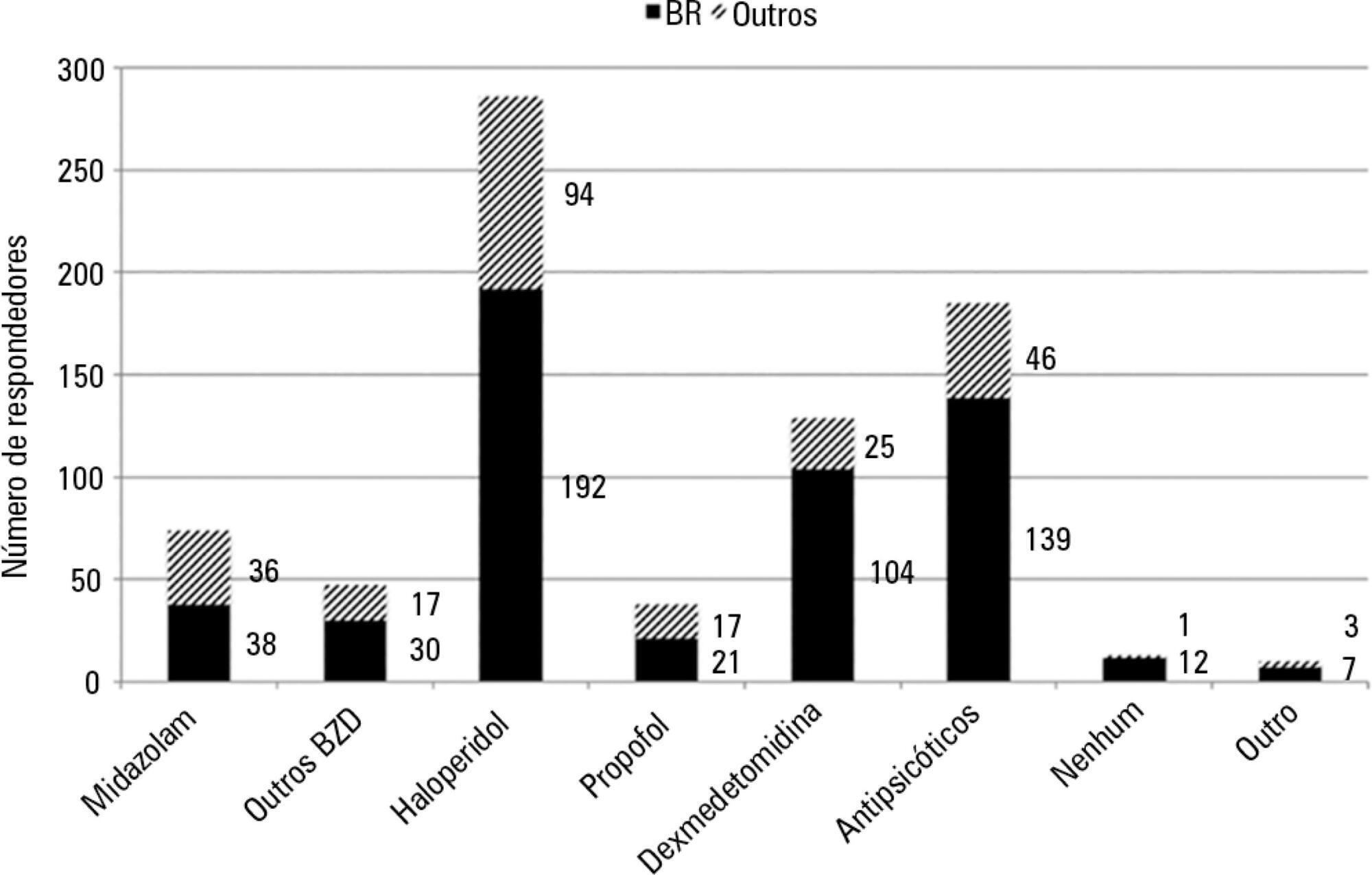
-
Original Articles
The implementation of an analgesia-based sedation protocol reduced deep sedation and proved to be safe and feasible in patients on mechanical ventilation
Rev Bras Ter Intensiva. 2013;25(3):188-196
Abstract
Original ArticlesThe implementation of an analgesia-based sedation protocol reduced deep sedation and proved to be safe and feasible in patients on mechanical ventilation
Rev Bras Ter Intensiva. 2013;25(3):188-196
DOI 10.5935/0103-507X.20130034
Views0INTRODUCTION:
Deep sedation in critically ill patients is associated with a longer duration of mechanical ventilation and a prolonged length of stay in the intensive care unit. Several protocols have been used to improve these outcomes. We implement and evaluate an analgesia-based, goal-directed, nurse-driven sedation protocol used to treat critically ill patients who receive mechanical ventilation.
METHODS:
We performed a prospective, two-phase (before-after), non-randomized multicenter study that involved 13 intensive care units in Chile. After an observational phase (observational group, n=155), we designed, implemented and evaluated an analgesia-based, goal-directed, nurse-driven sedation protocol (intervention group, n=132) to treat patients who required mechanical ventilation for more than 48 hours. The primary outcome was to achieve ventilator-free days by day 28.
RESULTS:
The proportion of patients in deep sedation or in a coma decreased from 55.2% to 44.0% in the interventional group. Agitation did not change between the periods and remained approximately 7%. Ventilator-free days to day 28, length of stay in the intensive care unit and mortality were similar in both groups. At one year, post-traumatic stress disorder symptoms in survivors were similar in both groups.
CONCLUSIONS:
We designed and implemented an analgesia-based, goal-directed, nurse-driven sedation protocol in Chile. Although there was no improvement in major outcomes, we observed that the present protocol was safe and feasible and that it resulted in decreased periods of deep sedation without increasing agitation.
Keywords:analgesiaClinical protocolsDeep sedationIntensive care unitsPatient safetyRespiration, artificialSee more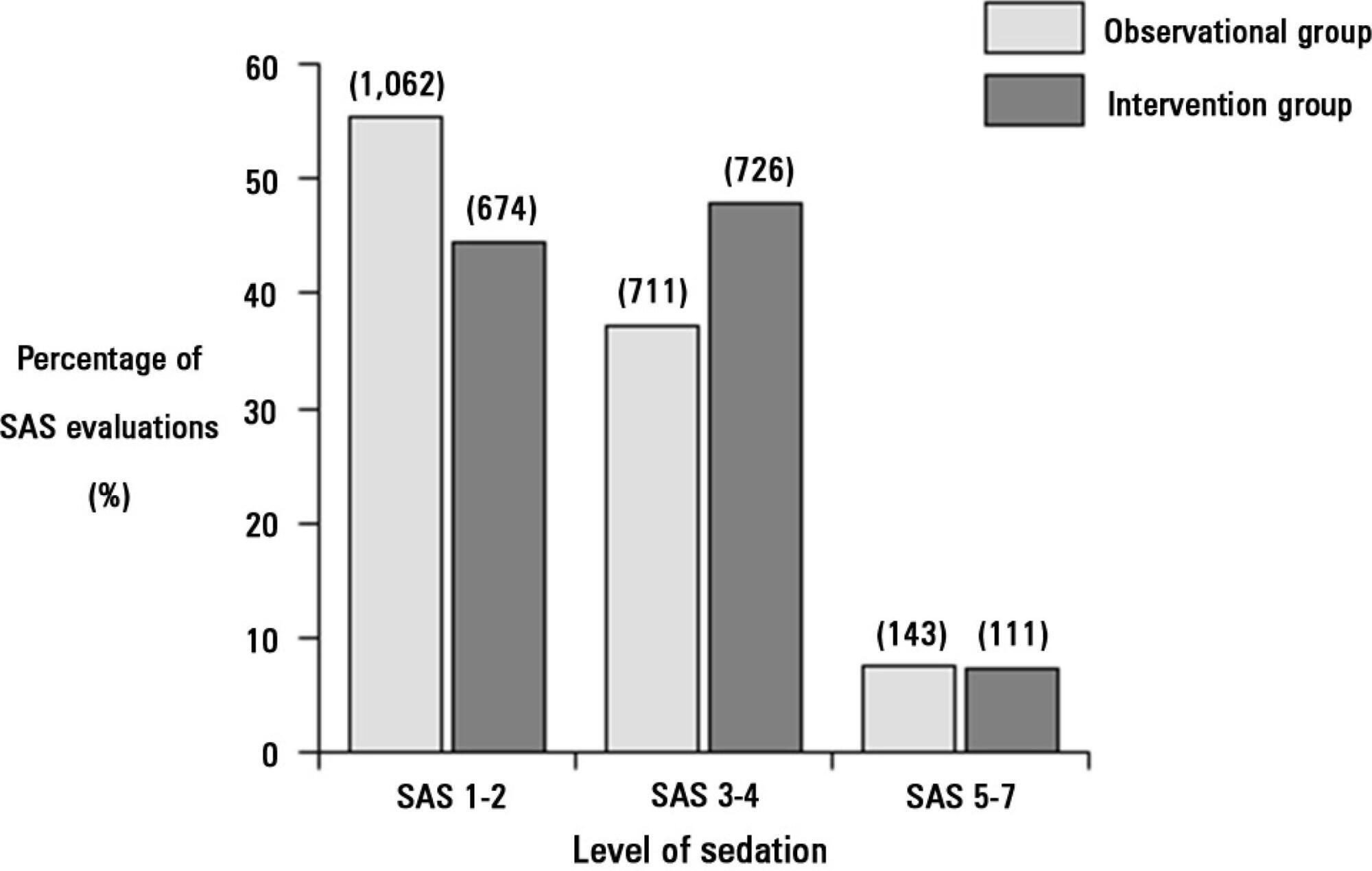
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis