Abstract
Crit Care Sci. 2023;35(4):377-385
DOI 10.5935/2965-2774.20230215-pt
To evaluate the occurrence of adverse events in the postoperative period of cardiac surgery in a pediatric intensive care unit and to find any patient characteristics that can predict such events.
This was a historical cohort study of patients recovering in the pediatric intensive care unit for the first 7 days after cardiac surgery between April and December 2019, by reviewing the medical records. The following were reviewed: demographic, clinical, and laboratory characteristics; patient severity scores; and selected adverse events, grouped into device-related, surgical, and nonsurgical.
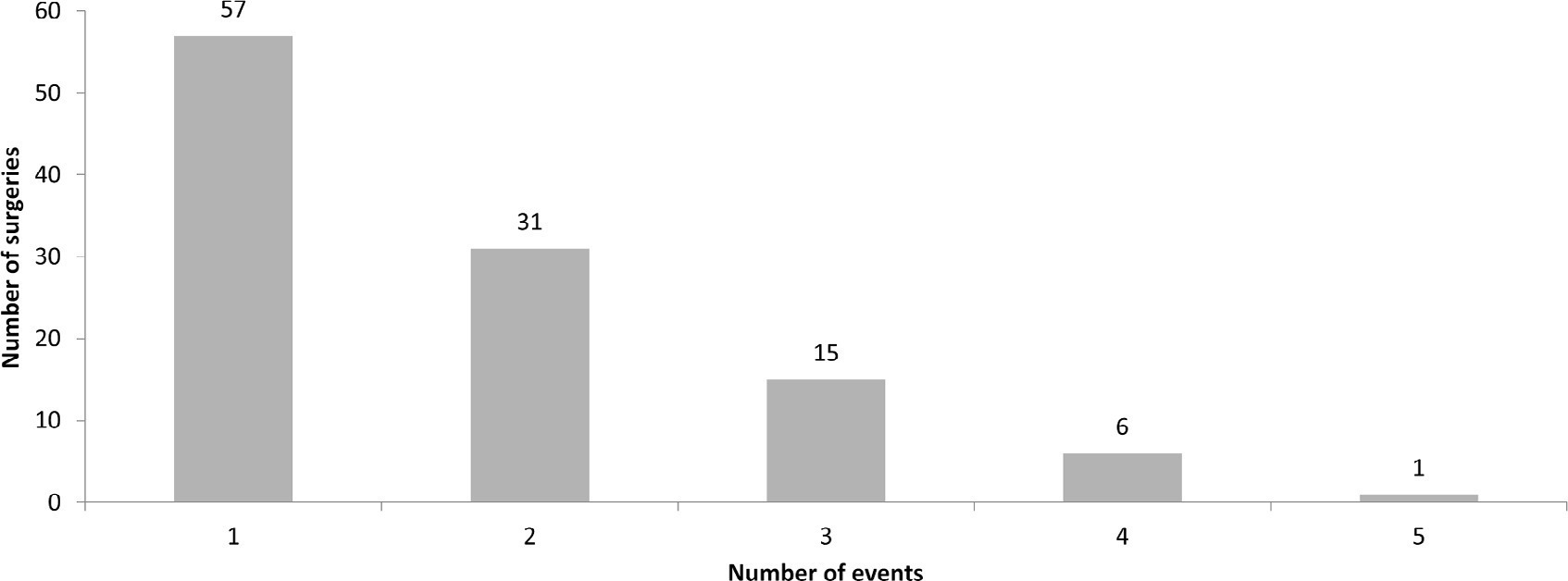
A total of 238 medical records were included. At least one adverse event occurred in 110 postoperative patients (46.2%). The total number of adverse events was 193 (81%). Vascular catheters were the most common cause, followed by cardiac arrest, bleeding, and surgical reexploration. In the univariate analysis, the vasoactive-inotropic score (VIS), Risk Adjustment in Congenital Heart Surgery (RACHS-1) score, age, Pediatric Index of Mortality (PIM-2), cardiopulmonary bypass and aortic clamping duration were significantly associated with adverse events. In the multivariate analysis, VIS ≥ 20 (OR 2.90; p = 0.004) and RACHS-1 ≥ 3 (OR 2.11; p = 0.019) were significant predictors, while age and delayed sternal closure showed only trends toward significance. To predict the occurrence of adverse events from VIS and RACHS-1, the area under the curve was 0.73 (95%CI 0.66 - 0.79).
Adverse events were quite frequent in children after cardiac surgery, especially those related to devices. The VIS and RACHS-1, used together, predicted the occurrence of adverse events well in this pediatric sample.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):386-392
DOI 10.5935/0103-507X.20220446-en
To analyze the association of patient safety culture perceived by nursing professionals with incidents recorded during nursing shifts in intensive care units.
This was a cross-sectional study that investigated patient safety culture measured by the Hospital Survey on Patient Safety Culture instrument. Descriptive statistics, chi-square tests, Student’s t-test and multiple linear regression models were analyzed considering a significance level of 5%.
The study reported a mean of 3.1 (standard deviation of 0.4) for the culture of patient safety in the perception of nursing professionals and 480 incidents with and without damage recorded during the nursing shifts. The variables patient safety culture with a difference between means of 0.543 (95%CI 0.022 - 1.065; p < 0.05) and nursing assistants with a difference between means of -0.133 (95%CI -0.192 - -0.074; p < 0.05) were associated with the incidents recorded during the nursing shifts. Further, nursing assistants had a lower tendency to record incidents than did the nurses.
The strengthening of the patient safety culture and the aspects tangential to the nursing professionals represent a possible target for interventions to encourage the recording of incidents during the nursing shift shifts and improve patient safety.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):327-334
DOI 10.5935/0103-507X.20220070-en
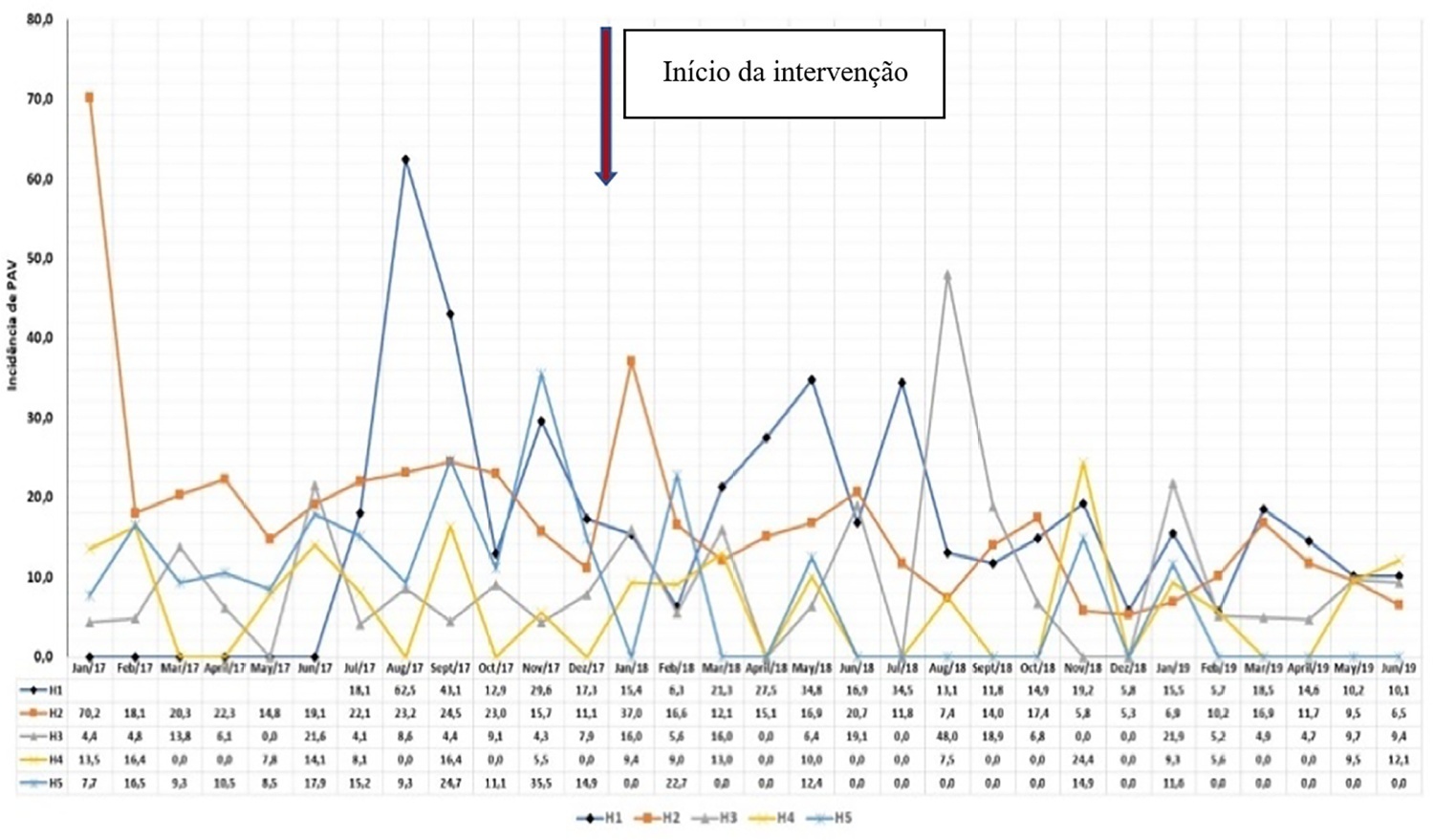
To describe the implementation and results of the collaborative PROADI-SUS project by the Brazilian Ministry of Health to reduce healthcare-associated infections: ventilator-associated pneumonia, primary central line-associated bloodstream infection and catheter-associated urinary tract infections.
This was a prospective observational study that investigated the implementation stages and outcomes during 18 months in five intensive care units in the city of Recife. Reductions in healthcare-associated infections in each unit were calculated using previous medians compared to those of the study period.
The goal of reducing the three healthcare-associated infections, i.e., 30% in 18 months, was achieved in at least one of the healthcare-associated infections and was also achieved for two healthcare-associated infections in two hospitals and three healthcare-associated infections in just one hospital; the latter reached the target of 36 months. Implementing the bundles and monitoring the results by the professionals were considered essential actions by the local management teams. In addition, the acquisition of supplies and their availability alongside the beds, signage, checklists, staff awareness, adaptation, team building, training and celebration of achievements were assessed as being relevant for reducing healthcare-associated infections.
The collaborative approach reduced healthcare-associated infections, despite partial adherence to the bundles. The hypothesis is that success is related to the project methodology and motivated multidisciplinary teams, especially nursing teams.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):434-443
DOI 10.5935/0103-507X.20190084
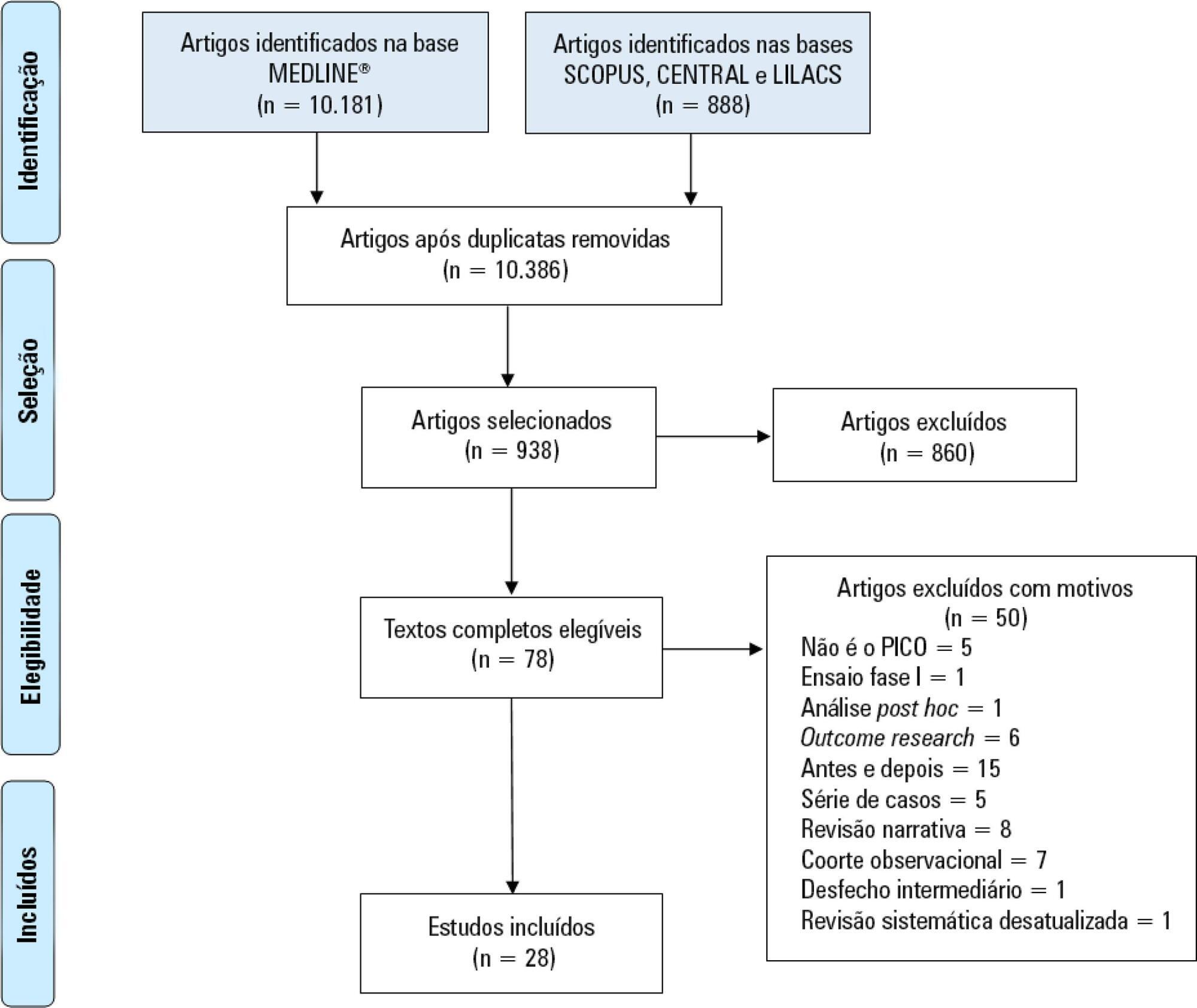
Immobility can cause several complications, including skeletal muscle atrophy and weakness, that influence the recovery of critically ill patients. This effect can be mitigated by early mobilization. Six key questions guided this research: Is early mobilization safe? Which patients are candidates for early mobilization? What are the contraindications? What is the appropriate dose, and how should it be defined? What results are obtained? What are the prognostic indicators for the use of early mobilization? The objective of this guideline was to produce a document that would provide evidence-based recommendations and suggestions regarding the early mobilization of critically ill adult patients, with the aim of improving understanding of the topic and making a positive impact on patient care. This guideline was based on a systematic review of articles conducted using the PICO search strategy, as recommended by the Guidelines Project of the Associação Médica Brasileira. Randomized clinical trials, prognostic cohort studies, and systematic reviews with or without meta-analysis were selected, and the evidence was classified according to the Oxford Center for Evidence-based Medicine Levels of Evidence. For all the questions addressed, enough evidence was found to support safe and well-defined early mobilization, with prognostic indicators that support and recommend the technique. Early mobilization is associated with better functional outcomes and should be performed whenever indicated. Early mobilization is safe and should be the goal of the entire multidisciplinary team.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):131-141
DOI 10.5935/0103-507X.20170023
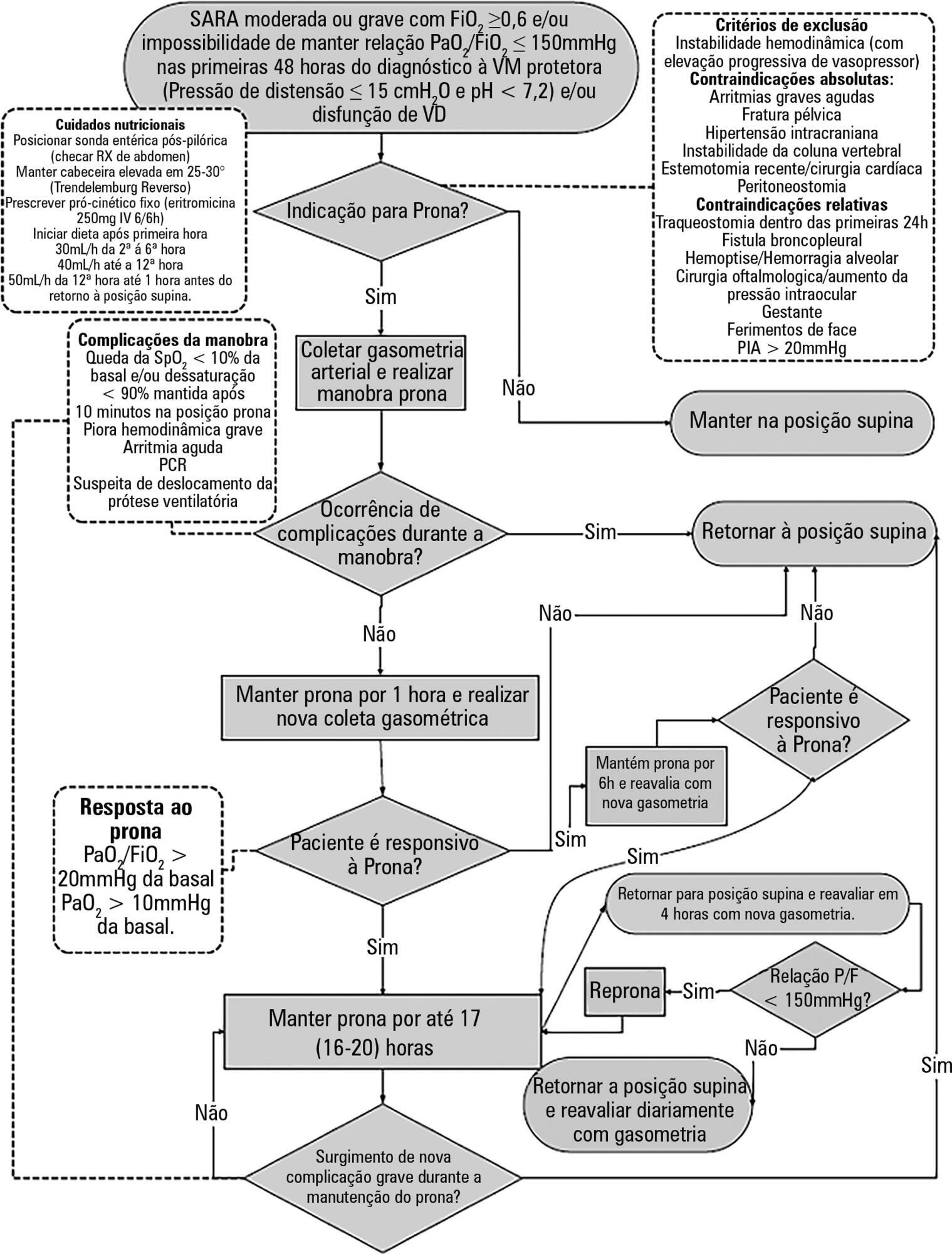
To construct and implement an instrument (checklist) to improve safety when performing the prone maneuver.
This was an applied, qualitative and descriptive study. The instrument was developed based on a broad review of the literature pertaining to the construction of a care protocol using the main electronic databases (MEDLINE, LILACS and Cochrane).
We describe the construction of a patient safety tool with numerous modifications and adaptations based on the observations of the multidisciplinary team regarding its use in daily practice.
The use of the checklist when performing the prone maneuver increased the safety and reliability of the procedure. The team's understanding of the tool's importance to patient safety and training in its use are necessary for its success.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):509-519
DOI 10.5935/0103-507X.20170076
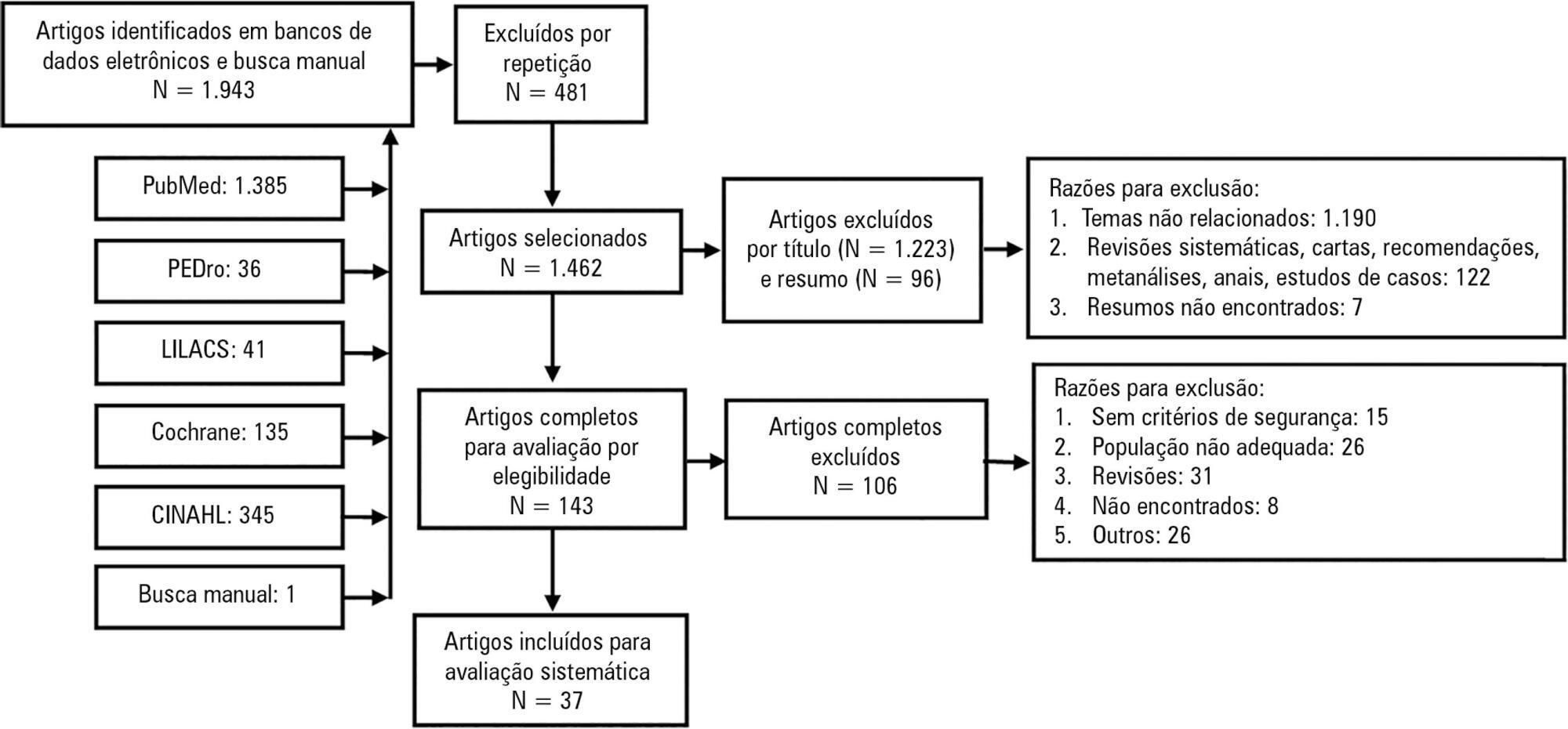
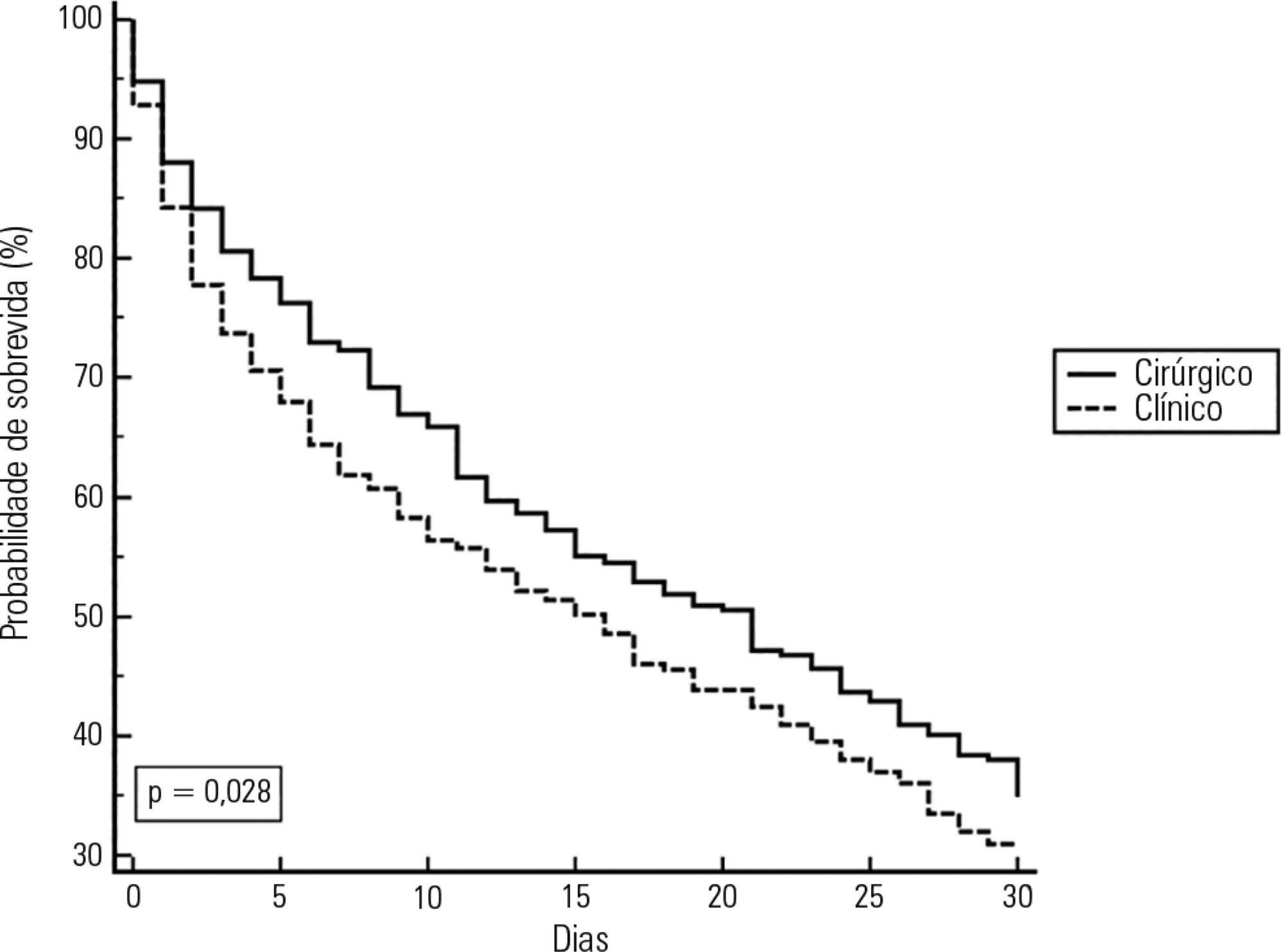
Mobilization of critically ill patients admitted to intensive care units should be performed based on safety criteria. The aim of the present review was to establish which safety criteria are most often used to start early mobilization for patients under mechanical ventilation admitted to intensive care units. Articles were searched in the PubMed, PEDro, LILACS, Cochrane and CINAHL databases; randomized and quasi-randomized clinical trials, cohort studies, comparative studies with or without simultaneous controls, case series with 10 or more consecutive cases and descriptive studies were included. The same was performed regarding prospective, retrospective or cross-sectional studies where safety criteria to start early mobilization should be described in the Methods section. Two reviewers independently selected potentially eligible studies according to the established inclusion criteria, extracted data and assessed the studies' methodological quality. Narrative description was employed in data analysis to summarize the characteristics and results of the included studies; safety criteria were categorized as follows: cardiovascular, respiratory, neurological, orthopedic and other. A total of 37 articles were considered eligible. Cardiovascular safety criteria exhibited the largest number of variables. However, respiratory safety criteria exhibited higher concordance among studies. There was greater divergence among the authors regarding neurological criteria. There is a need to reinforce the recognition of the safety criteria used to start early mobilization for critically ill patients; the parameters and variables found might contribute to inclusion into service routines so as to start, make progress and guide clinical practice.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):278-284
DOI 10.5935/0103-507X.20160045
To evaluate the implementation of a multidisciplinary rapid response team led by an intensive care physician at a university hospital.
This retrospective cohort study analyzed assessment forms that were completed during the assessments made by the rapid response team of a university hospital between March 2009 and February 2014.
Data were collected from 1,628 assessments performed by the rapid response team for 1,024 patients and included 1,423 code yellow events and 205 code blue events. The number of assessments was higher in the first year of operation of the rapid response team. The multivariate analysis indicated that age (OR 1.02; 95%CI 1.02 - 1.03; p < 0.001), being male (OR 1.48; 95%CI 1.09 - 2.01; p = 0.01), having more than one assessment (OR 3.31; 95%CI, 2.32 - 4.71; p < 0.001), hospitalization for clinical care (OR 1.77; 95%CI 1.29 - 2.42; p < 0.001), the request of admission to the intensive care unit after the code event (OR 4.75; 95%CI 3.43 - 6.59; p < 0.001), and admission to the intensive care unit before the code event (OR 2.13; 95%CI 1.41 - 3.21; p = 0.001) were risk factors for hospital mortality in patients who were seen for code yellow events.
The hospital mortality rates were higher than those found in previous studies. The number of assessments was higher in the first year of operation of the rapid response team. Moreover, hospital mortality was higher among patients admitted for clinical care.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):130-136
DOI 10.5935/0103-507X.20140019
To assess the performance of central venous oxygen saturation, lactate, base deficit, and C-reactive protein levels and SOFA and SWIFT scores on the day of discharge from the intensive care unit as predictors of patient readmission to the intensive care unit.
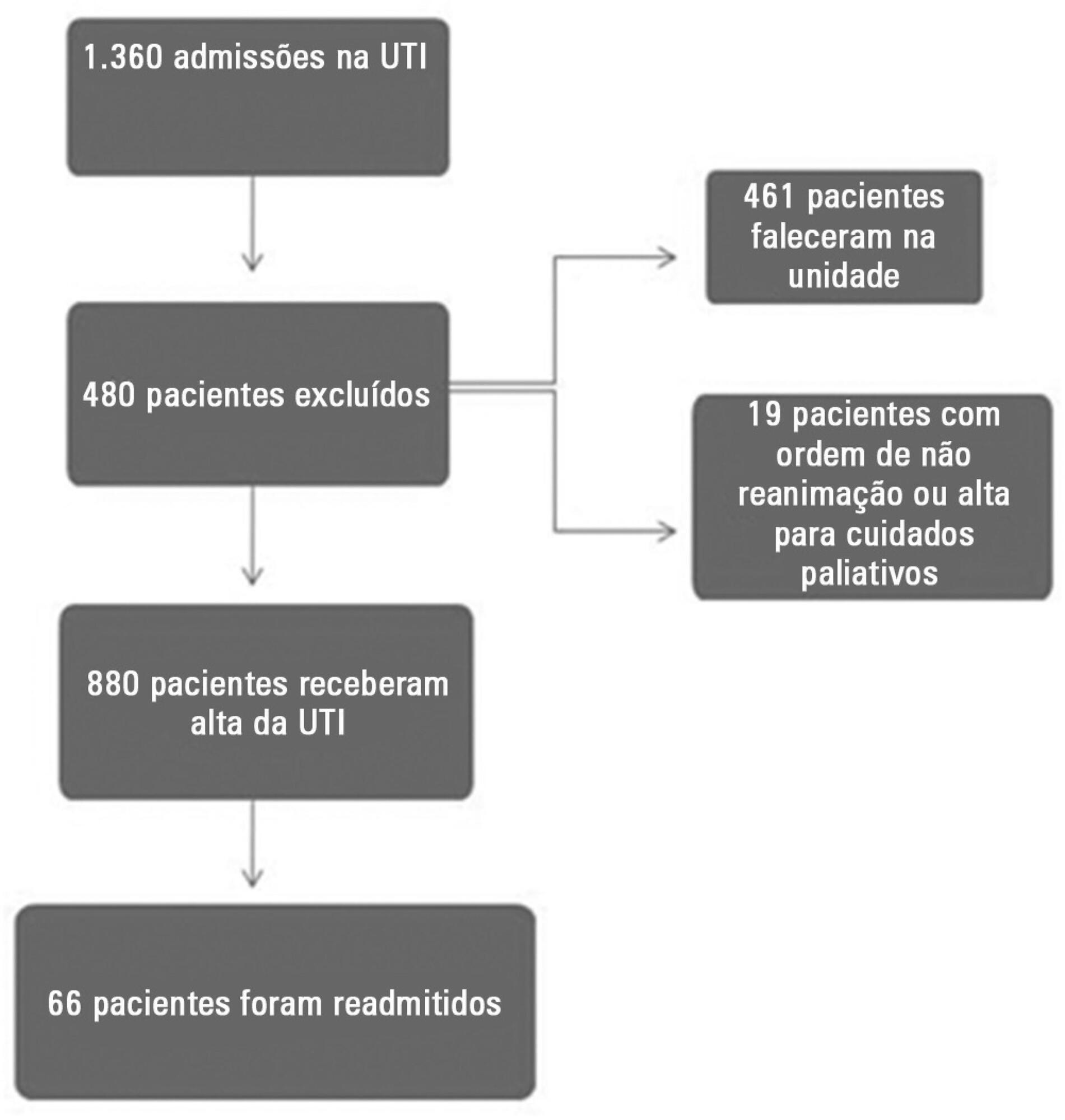
This prospective and observational study collected data from 1,360 patients who were admitted consecutively to a clinical-surgical intensive care unit from August 2011 to August 2012. The clinical characteristics and laboratory data of readmitted and non-readmitted patients after discharge from the intensive care unit were compared. Using a multivariate analysis, the risk factors independently associated with readmission were identified.
The C-reactive protein, central venous oxygen saturation, base deficit, and lactate levels and the SWIFT and SOFA scores did not correlate with the readmission of critically ill patients. Increased age and contact isolation because of multidrug-resistant organisms were identified as risk factors that were independently associated with readmission in this study group.
Inflammatory and perfusion parameters were not associated with patient readmission. Increased age and contact isolation because of multidrug-resistant organisms were identified as predictors of readmission to the intensive care unit.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)