Abstract
Crit Care Sci. 2023;35(2):177-186
DOI 10.5935/2965-2774.20230348-pt
To measure the prognostic value of peripheral ischemic microvascular reserve in the context of persistent sepsis-induced hyperlactatemia and measure its influence on the temporal dynamics of lactate and the strength of association between these variables.
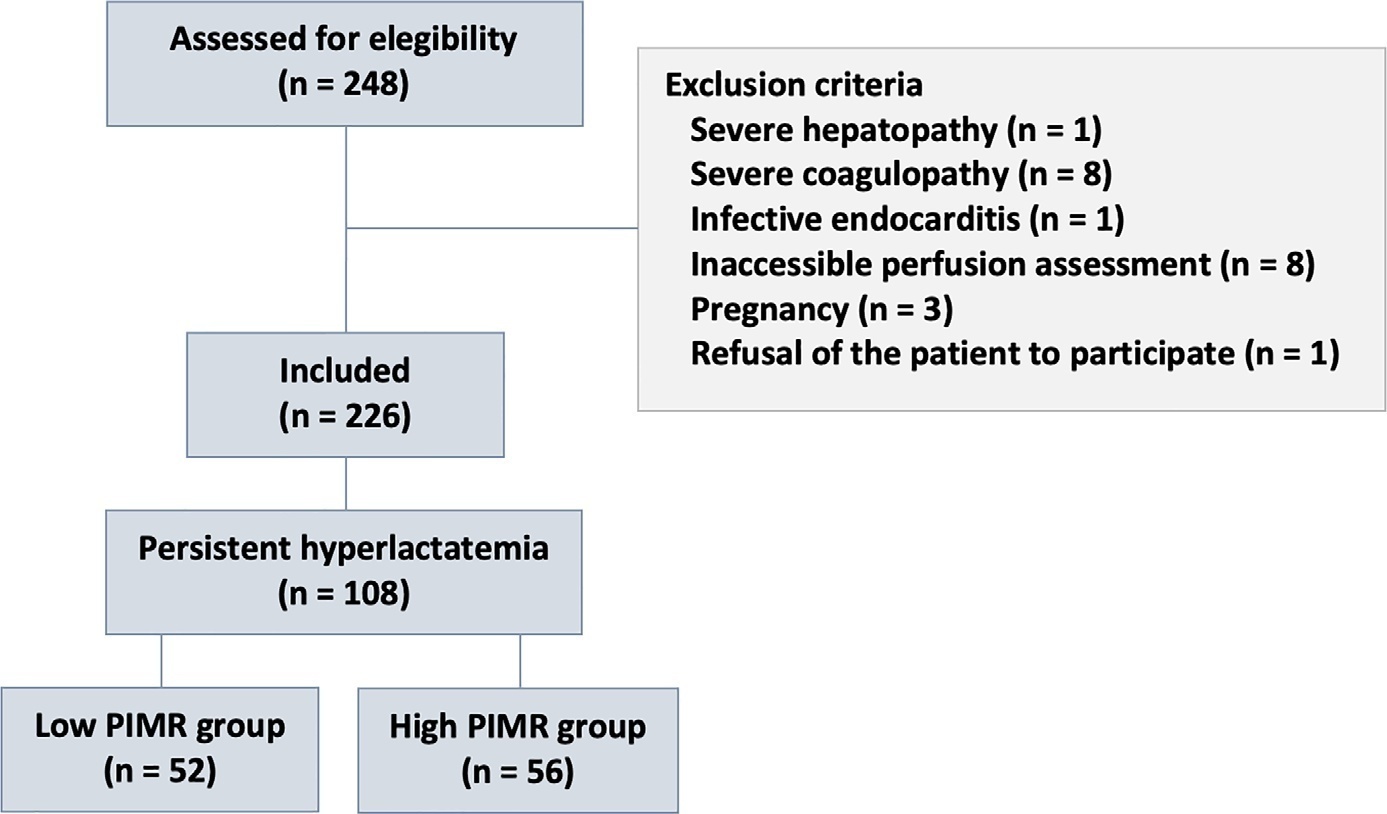
This post hoc analysis of the peripheral perfusion index/postocclusive reactive hyperemia trial, an observational cohort study that enrolled patients with sepsis who persisted with lactate levels ≥ 2mmol/L after fluid resuscitation (with or without shock). Peripheral ischemic microvascular reserve was evaluated using the association of the peripheral perfusion index and postocclusive reactive hyperemia techniques. The cutoff point of ∆ peripheral perfusion index peak values (%) defined the groups with low (≤ 62%) and high peripheral ischemic microvascular reserve (> 62%).
A total of 108 consecutive patients with persistent sepsis-induced hyperlactatemia were studied. The high peripheral ischemic microvascular reserve group showed higher 28-day mortality than the low peripheral ischemic microvascular reserve group (p < 0.01). The temporal dynamics of lactate within the first 48 hours showed a rapid decrease in lactate levels in the low peripheral ischemic microvascular reserve group (p < 0.01). However, this result was not reproduced in the linear mixed effects model. A weak correlation between peripheral ischemic microvascular reserve (%) and lactate level (mmol/L) was observed within the first 24 hours (r = 0.23; p < 0.05).
The prognostic value of high peripheral ischemic microvascular reserve was confirmed in the context of persistent sepsis-induced hyperlactatemia. Although there was a weak positive correlation between peripheral ischemic microvascular reserve value and lactate level within the first 24 hours of sepsis diagnosis, the low peripheral ischemic microvascular reserve group appeared to have a faster decrease in lactate over the 48 hours of follow-up.
Abstract
Rev Bras Ter Intensiva. 2022;34(1):154-162
DOI 10.5935/0103-507X.20220010-en
To evaluate the influence of patient characteristics on hyperlactatemia in an infected population admitted to intensive care units and the influence of hyperlactatemia severity on hospital mortality.
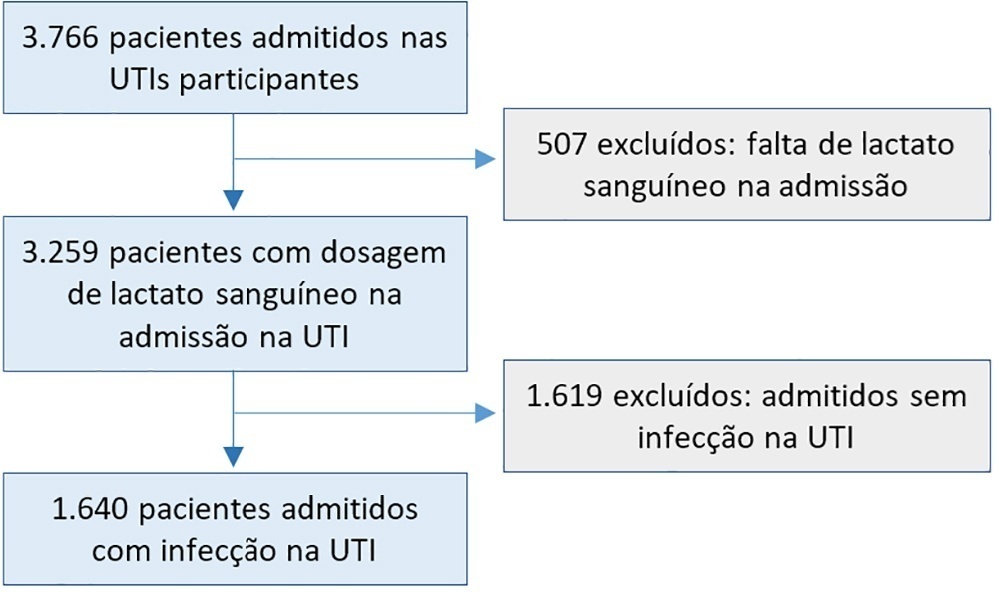
A post hoc analysis of hyperlactatemia in the INFAUCI study, a national prospective, observational, multicenter study, was conducted in 14 Portuguese intensive care units. Infected patients admitted to intensive care units with a lactate measurement in the first 12 hours of admission were selected. Sepsis was identified according to the Sepsis-2 definition accepted at the time of data collection. The severity of hyperlactatemia was classified as mild (2 - 3.9mmol/L), moderate (4.0 - 9.9mmol/L) or severe (> 10mmol/L).
In a total of 1,640 patients infected on admission, hyperlactatemia occurred in 934 patients (57%), classified as mild, moderate and severe in 57.0%, 34.4% and 8.7% of patients, respectively. The presence of hyperlactatemia and a higher degree of hyperlactatemia were both associated with a higher Simplified Acute Physiology Score II, a higher Charlson Comorbidity Index and the presence of septic shock. The lactate Receiver Operating Characteristic curve for hospital mortality had an area under the curve of 0.64 (95%CI 0.61 - 0.72), which increased to 0.71 (95%CI 0.68 - 0.74) when combined with Sequential Organ Failure Assessment score. In-hospital mortality with other covariates adjusted by Simplified Acute Physiology Score II was associated with moderate and severe hyperlactatemia, with odds ratio of 1.95 (95%CI 1.4 - 2.7; p < 0.001) and 4.54 (95%CI 2.4 - 8.5; p < 0.001), respectively.
Blood lactate levels correlate independently with in-hospital mortality for moderate and severe degrees of hyperlactatemia.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):49-57
DOI 10.5935/0103-507X.20200009
To characterize a cohort of acute-on-chronic liver failure patients in Intensive Care and to analyze the all-cause 28-day mortality risk factors assessed at ICU admission and day 3.
This was a retrospective cohort study of consecutive patients admitted to the intensive care unit between March 2013 and December 2016.
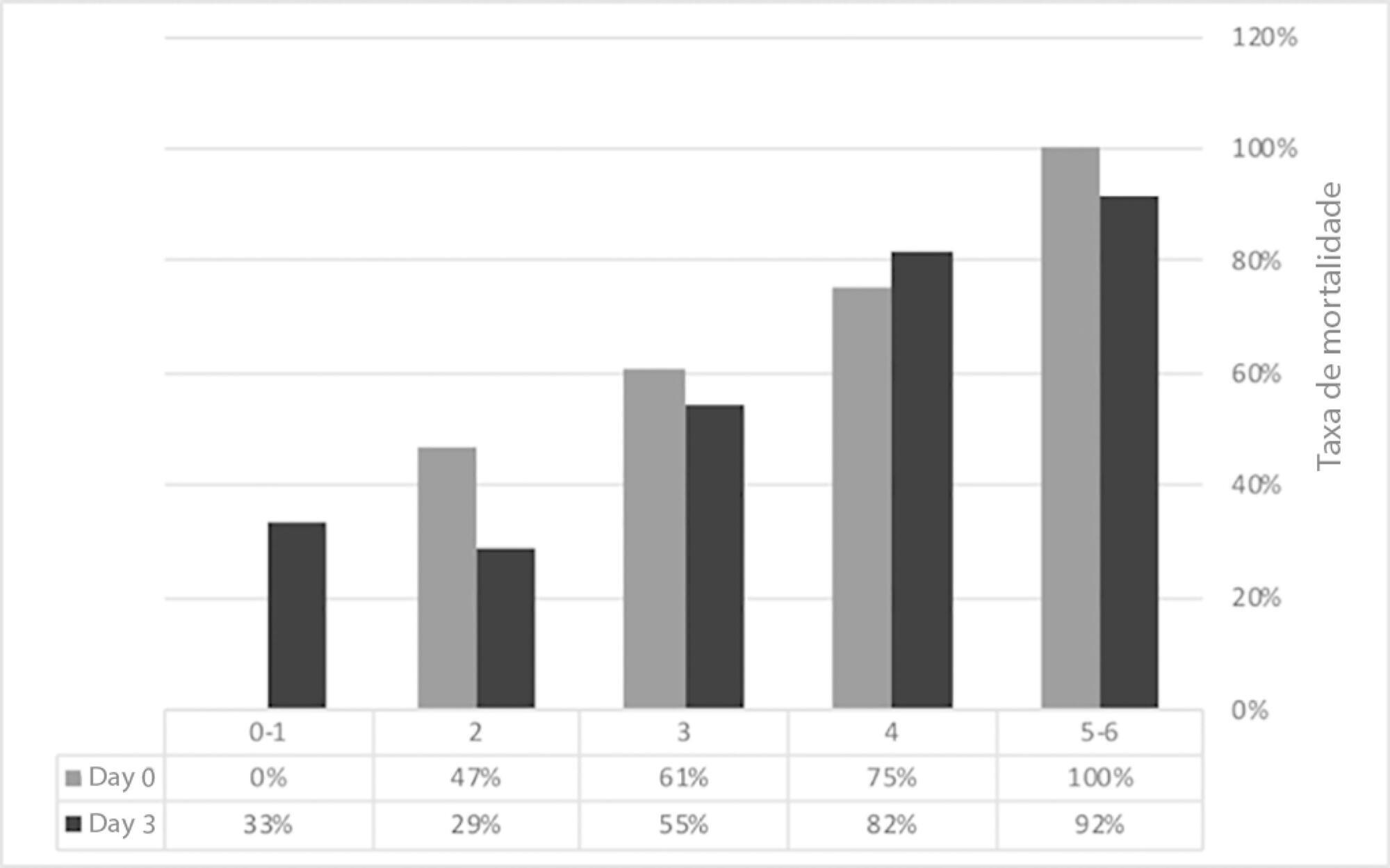
Seventy-one patients were included. The median age was 59 (51 - 64) years, and 81.7% of patients were male. Alcohol consumption alone (53.5%) was the most frequent etiology of cirrhosis and infection (53.5%) was the most common acute-on-chronic liver failure precipitating event. At intensive care unit admission, the clinical severity scores were APACHE II 21 (16 - 23), CLIF-SOFA 13 (11 - 15), Child-Pugh 12 (10 - 13) and MELD 27 (20 - 32). The acute-on-chronic liver failure scores were no-acute-on-chronic liver failure: 11.3%; one: 14.1%; two: 28.2% and three: 46.5%; and the number of organ failures was one: 4.2%; two: 42.3%; three: 32.4%; four: 16.9%; and five: 4.2%. Liver transplantation was performed in 15.5% of patients. The twenty-eight-day mortality rate was 56.3%, and the in-ICU mortality rate was 49.3%. Organ failure at intensive care unit admission (p = 0.02; OR 2.1; 95%CI 1.2 - 3.9), lactate concentration on day 3 (p = 0.02; OR 6.3; 95%CI 1.4 - 28.6) and the international normalized ratio on day 3 (p = 0.03; OR 10.2; 95%CI 1.3 - 82.8) were independent risk factors.
Acute-on-chronic liver failure patients presented with high clinical severity and mortality rates. The number of organ failures at intensive care unit admission and the lactate and international normalized ratio on day 3 were independent risk factors for 28-day mortality. We consider intensive care essential for acute-on-chronic liver failure patients and timely liver transplant was vital for selected patients.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):130-136
DOI 10.5935/0103-507X.20140019
To assess the performance of central venous oxygen saturation, lactate, base deficit, and C-reactive protein levels and SOFA and SWIFT scores on the day of discharge from the intensive care unit as predictors of patient readmission to the intensive care unit.
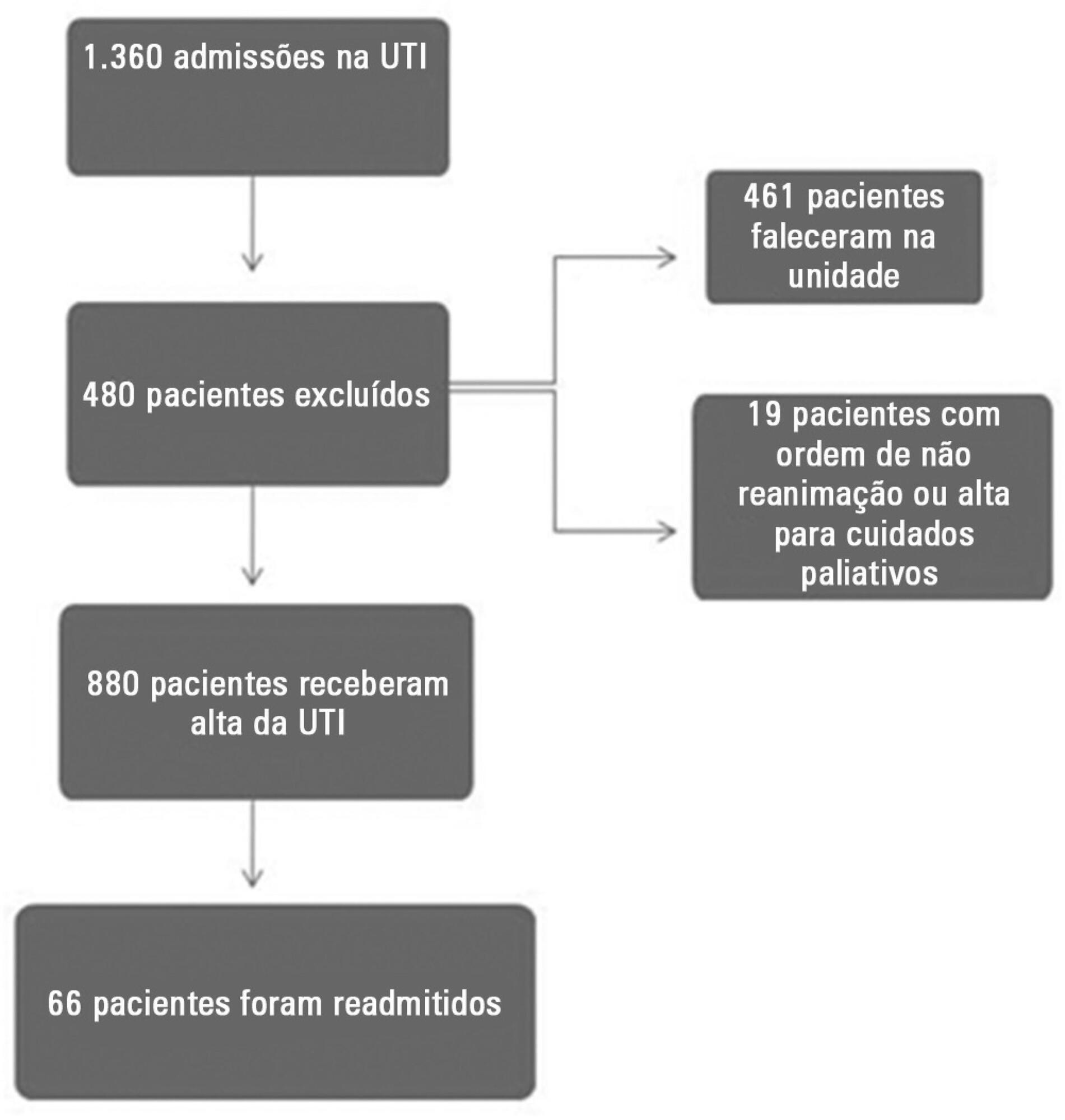
This prospective and observational study collected data from 1,360 patients who were admitted consecutively to a clinical-surgical intensive care unit from August 2011 to August 2012. The clinical characteristics and laboratory data of readmitted and non-readmitted patients after discharge from the intensive care unit were compared. Using a multivariate analysis, the risk factors independently associated with readmission were identified.
The C-reactive protein, central venous oxygen saturation, base deficit, and lactate levels and the SWIFT and SOFA scores did not correlate with the readmission of critically ill patients. Increased age and contact isolation because of multidrug-resistant organisms were identified as risk factors that were independently associated with readmission in this study group.
Inflammatory and perfusion parameters were not associated with patient readmission. Increased age and contact isolation because of multidrug-resistant organisms were identified as predictors of readmission to the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):118-124
DOI 10.1590/S0103-507X2010000200004
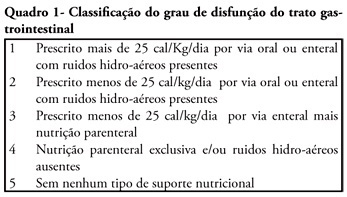
OBJECTIVE: We aimed to investigate the prevalence and independent predictors of prolonged gastrointestinal dysfunction in critically ill patients admitted to the intensive care unit. METHODS: Retrospective and observational cohort study performed in a mixed 24 beds intensive care unit in a tertiary center. Patients admitted in the intensive care unit between August 2003 and January 2004, who had a length of stay in the intensive care unit greater than 4 days were enrolled. Gastrointestinal function was evaluated daily according to a classification that considered physical examination (bowel sounds or distension) and the nutritional support progress. RESULTS: Were included 128 patients. The mean age was 56 ± 19 years, 63.3% were male and 77.3% were surgical patients. Prolonged gastrointestinal dysfunction occurred in 35% of patients, with prevalence 3.3 times higher in surgical patients (27%) than in medical patients (8%). Endoscopies were performed in 38 patients (29.7%), and in three quarters of them erosive lesions and or bleeding were observed. Gastrointestinal dysfunction was more frequent in patients presenting moderate or severe edema (51%) than in patients without edema (22.5%) (p<0.05). In the logistic regression analysis, a serum lactate level higher than 5.2 mEq/L (RR 6.69 95%CI 15-38.7, P = 0.034) and the presence of a low oxygenation index (RR 12.4 95%CI 2.18-70.8, p = 0.005) were predictive of gastrointestinal dysfunction. CONCLUSION: Prolonged gastrointestinal dysfunction was highly prevalent in this heterogeneous population of critically ill patients. Admission high serum lactate levels and a low oxygenation index were predictive of prolonged gastrointestinal dysfunction.
Abstract
Rev Bras Ter Intensiva. 2006;18(4):360-365
DOI 10.1590/S0103-507X2006000400007
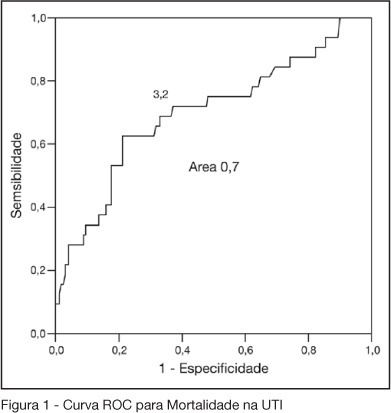
BACKGROUND AND OBJECTIVES: One of the greatest challenges found by the intensivists in their daily activities is tissue hipoperfusion control. Blood lactate is generally accepted as a marker of tissular hypoxia and several studies have demonstrated good correlation between blood lactate and prognosis during shock and resuscitation. The aim of this study was to evaluate the clinical utility of arterial blood lactate as a marker of morbidity and mortality in critically ill patients in the post-operative period of high risk non-cardiac surgeries. METHODS: Prospective and observational cohort study realized in an ICU of a tertiary hospital during a four month period. Demographic data of the patients submitted to high risk surgeries were collected, besides arterial lactate measures and number and type of complications in the post-operative period. To the statistic analysis was considered as significant a p < 0.05. The predictive ability of the indexes to differentiate survivors from non-survivors was tested using ROC curves. Lenght of ICU stay estimation where calculated by Kaplan Meier method. RESULTS: Were included 202 patients. 50.2% were female and their mean age was 66.5 ± 13.6 years. APACHE II score was 17.4 ± 3.0 and the median of MODS score was 4 (2-6). Median lenght of surgeries was 4h (3-6h). 70.7% of the surgeries were elective ones. ICU and hospital mortality were 15.6% and 33.7%, respectively. The best lactate value to discriminate mortality was 3.2 mmol/L, with sensitivity of 62.5%, specificity of 78.8% and an area under the curve of 0.7. 62.5% of patients with lactate > 3.2 did not survive versus 21.2% of survivors (OR = 2.95 IC95% 1.98- 4.38, p < 0.0001). ICU lenght of stay was greater when > 3.2 mmol/L (log rank 0.007) lactate. CONCLUSIONS: High risk patients submitted to non cardiac surgeries and admitted to the ICU with hiperlactatemia, defined as an arterial lactate > 3.2 mmol/L, are prone to a longer ICU lenght of stay and to die.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)