Abstract
Rev Bras Ter Intensiva. 2006;18(4):360-365
DOI 10.1590/S0103-507X2006000400007
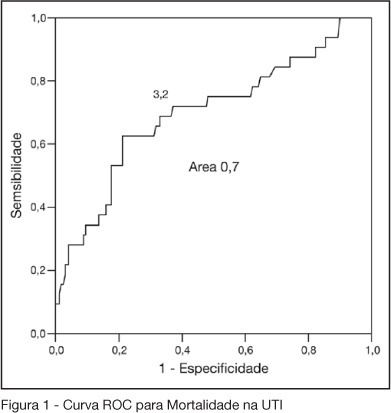
BACKGROUND AND OBJECTIVES: One of the greatest challenges found by the intensivists in their daily activities is tissue hipoperfusion control. Blood lactate is generally accepted as a marker of tissular hypoxia and several studies have demonstrated good correlation between blood lactate and prognosis during shock and resuscitation. The aim of this study was to evaluate the clinical utility of arterial blood lactate as a marker of morbidity and mortality in critically ill patients in the post-operative period of high risk non-cardiac surgeries. METHODS: Prospective and observational cohort study realized in an ICU of a tertiary hospital during a four month period. Demographic data of the patients submitted to high risk surgeries were collected, besides arterial lactate measures and number and type of complications in the post-operative period. To the statistic analysis was considered as significant a p < 0.05. The predictive ability of the indexes to differentiate survivors from non-survivors was tested using ROC curves. Lenght of ICU stay estimation where calculated by Kaplan Meier method. RESULTS: Were included 202 patients. 50.2% were female and their mean age was 66.5 ± 13.6 years. APACHE II score was 17.4 ± 3.0 and the median of MODS score was 4 (2-6). Median lenght of surgeries was 4h (3-6h). 70.7% of the surgeries were elective ones. ICU and hospital mortality were 15.6% and 33.7%, respectively. The best lactate value to discriminate mortality was 3.2 mmol/L, with sensitivity of 62.5%, specificity of 78.8% and an area under the curve of 0.7. 62.5% of patients with lactate > 3.2 did not survive versus 21.2% of survivors (OR = 2.95 IC95% 1.98- 4.38, p < 0.0001). ICU lenght of stay was greater when > 3.2 mmol/L (log rank 0.007) lactate. CONCLUSIONS: High risk patients submitted to non cardiac surgeries and admitted to the ICU with hiperlactatemia, defined as an arterial lactate > 3.2 mmol/L, are prone to a longer ICU lenght of stay and to die.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):348-353
DOI 10.1590/S0103-507X2007000300014
BACKGROUND AND OBJECTIVES: Each intensive care units result has to be observed in the context of medical care, as well as the institution witch it belongs. There are many types of prognostic index in intensive care. The APACHE II was introduced by Knaus et al. in 1985, being a widely used system to evaluate the illness severity in intensive care patients. This objective was evaluated the prognostic index (APACHE II) in patients submitted to elective or emergency gastrointestinal surgery admitted to the ICU. METHODS: Medical school intensive care unit. It was collected the following data: age, sex, length of stay, intensive care indication, type of surgery (elective or emergency), body mass index (BMI) APACHE II and predicted mortality. RESULTS: A total of 38 patients data were collected during the period of April 2005 to April 2006. Eighteen patients died and twenty survived. The age of the non-survivors varied from 44 to 92 (mean age 66.6); while the age of the survivors varied from 28 to 78 (mean age 59. 1). The BMI of the non-survivors varied from 22 to 29 (mean body mass index 26) while in the other group the mean body mass index was 25. 6. No significant difference was noted in the age and body mass index of both groups. The length of stay varied from 2 to 52 days in the non-survivors group (mean 11.3 days), while in the survivors group varied from 1 to 30 days (mean 4.9). The APACHE II varied from 5 to 32 in the non-survivors group (mean 19.14). While in the survivors group varied from 1 to 18 (mean 8.6). The length of stay and APACHE II demonstrated a significant difference in both groups, being higher in the non-survivors group. The non-survivors predicted mortality varied from 3.1 to 84.9 (mean 38.8); while the survivors mean was 7.5. The Standardized Mortality Rate in this study was 1.22. CONCLUSIONS: Non-survivors patients APACHE II was higher than the survivors; the SMR was similar to others studies; the length of stay was longer in the non-survivors group; no statistic difference was noted in the body mass index.