Abstract
Rev Bras Ter Intensiva. 2021;33(4):583-591
DOI 10.5935/0103-507X.20210085
To ascertain the cumulative incidence of acute organ failure and intensive care unit admission in cancer patients.
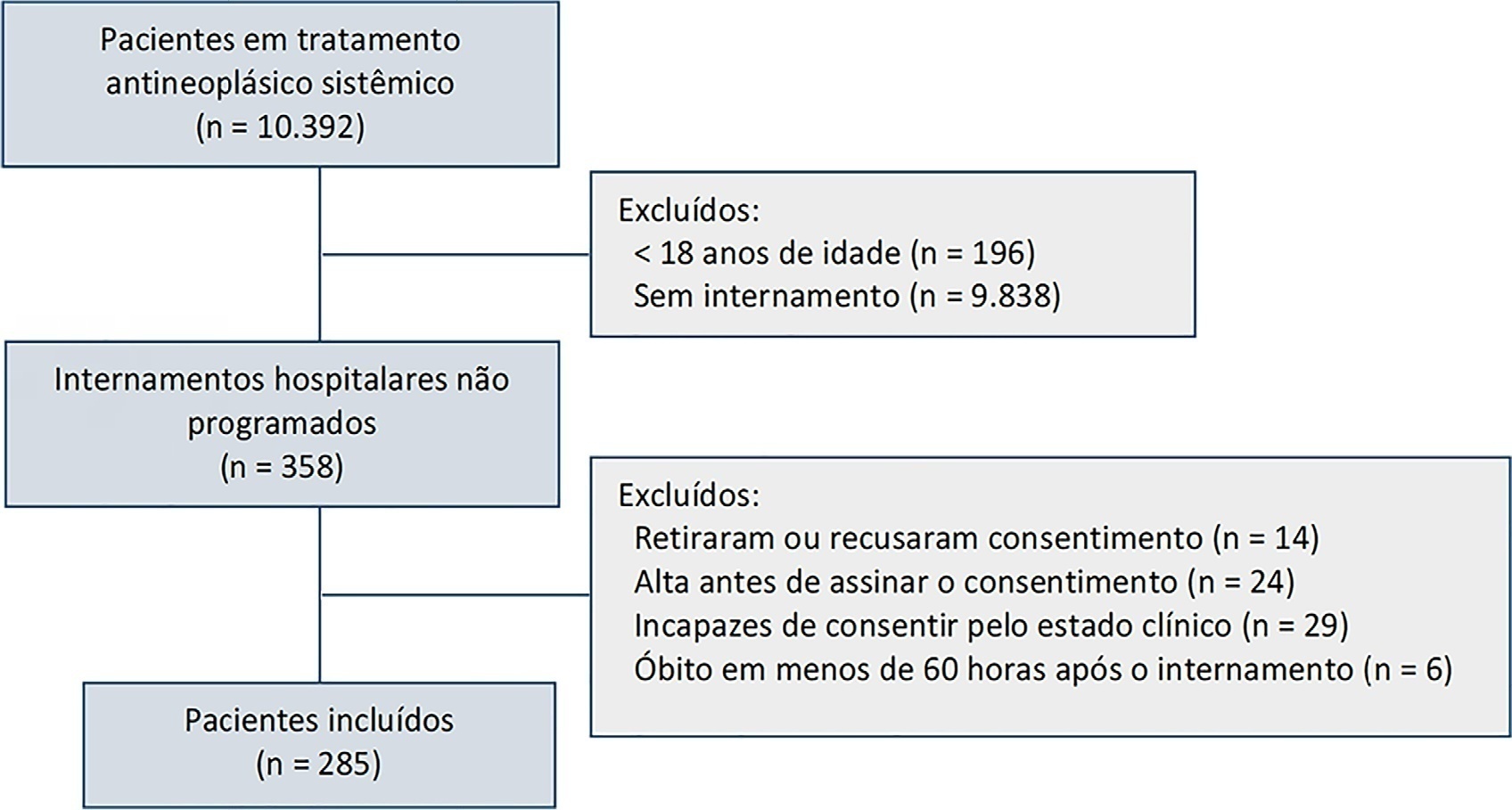
This was a single-center prospective cohort study of adult cancer patients admitted for unscheduled inpatient care while on systemic cancer treatment.
Between August 2018 and February 2019, 10,392 patients were on systemic treatment, 358 had unscheduled inpatient care and were eligible for inclusion, and 285 were included. The mean age was 60.9 years, 50.9% were male, and 17.9% of patients had hematologic cancers. The cumulative risk of acute organ failure was 39.6% (95%CI: 35 - 44), and that of intensive care unit admission among patients with acute organ failure was 15.0% (95%CI: 12 - 18). On admission, 62.1% of patients were considered not eligible for artificial organ replacement therapy. The median follow-up time was 9.5 months. Inpatient mortality was 17.5%, with an intensive care unit mortality rate of 58.8% and a median cohort survival of 134 days (95%CI: 106 - 162). In multivariate analysis, acute organ failure was associated with 6-month postdischarge mortality (HR 1.6; 95%CI: 1.2 - 2.2).
The risk of acute organ failure in cancer patients admitted for unscheduled inpatient care while on systemic treatment was 39.6%, and the risk of intensive care unit admission was 15.0%. Acute organ failure in cancer patients was an independent poor prognostic factor for inpatient hospital mortality and 6-month survival.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):49-57
DOI 10.5935/0103-507X.20200009
To characterize a cohort of acute-on-chronic liver failure patients in Intensive Care and to analyze the all-cause 28-day mortality risk factors assessed at ICU admission and day 3.
This was a retrospective cohort study of consecutive patients admitted to the intensive care unit between March 2013 and December 2016.
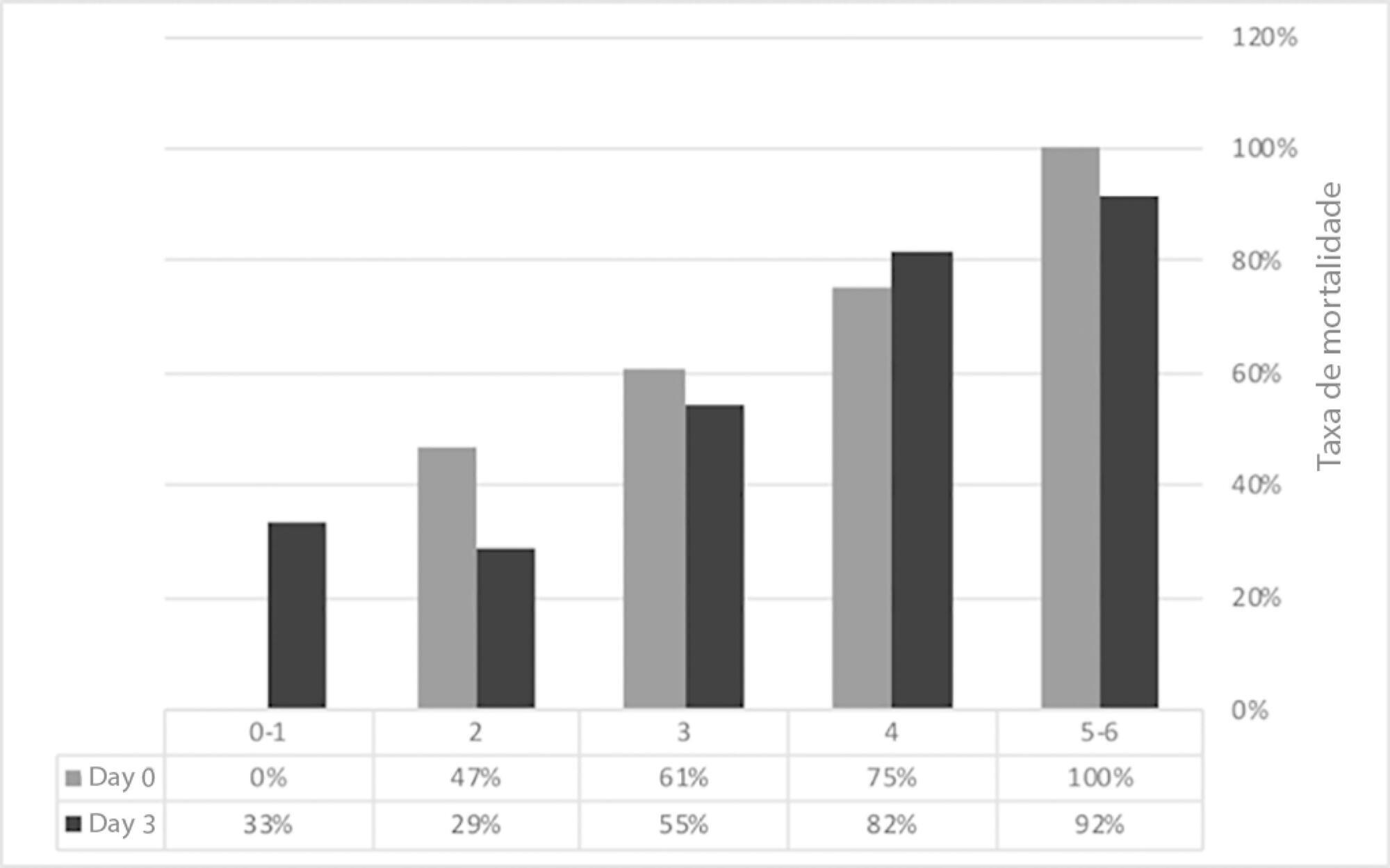
Seventy-one patients were included. The median age was 59 (51 - 64) years, and 81.7% of patients were male. Alcohol consumption alone (53.5%) was the most frequent etiology of cirrhosis and infection (53.5%) was the most common acute-on-chronic liver failure precipitating event. At intensive care unit admission, the clinical severity scores were APACHE II 21 (16 - 23), CLIF-SOFA 13 (11 - 15), Child-Pugh 12 (10 - 13) and MELD 27 (20 - 32). The acute-on-chronic liver failure scores were no-acute-on-chronic liver failure: 11.3%; one: 14.1%; two: 28.2% and three: 46.5%; and the number of organ failures was one: 4.2%; two: 42.3%; three: 32.4%; four: 16.9%; and five: 4.2%. Liver transplantation was performed in 15.5% of patients. The twenty-eight-day mortality rate was 56.3%, and the in-ICU mortality rate was 49.3%. Organ failure at intensive care unit admission (p = 0.02; OR 2.1; 95%CI 1.2 - 3.9), lactate concentration on day 3 (p = 0.02; OR 6.3; 95%CI 1.4 - 28.6) and the international normalized ratio on day 3 (p = 0.03; OR 10.2; 95%CI 1.3 - 82.8) were independent risk factors.
Acute-on-chronic liver failure patients presented with high clinical severity and mortality rates. The number of organ failures at intensive care unit admission and the lactate and international normalized ratio on day 3 were independent risk factors for 28-day mortality. We consider intensive care essential for acute-on-chronic liver failure patients and timely liver transplant was vital for selected patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):582-585
DOI 10.5935/0103-507X.20190075
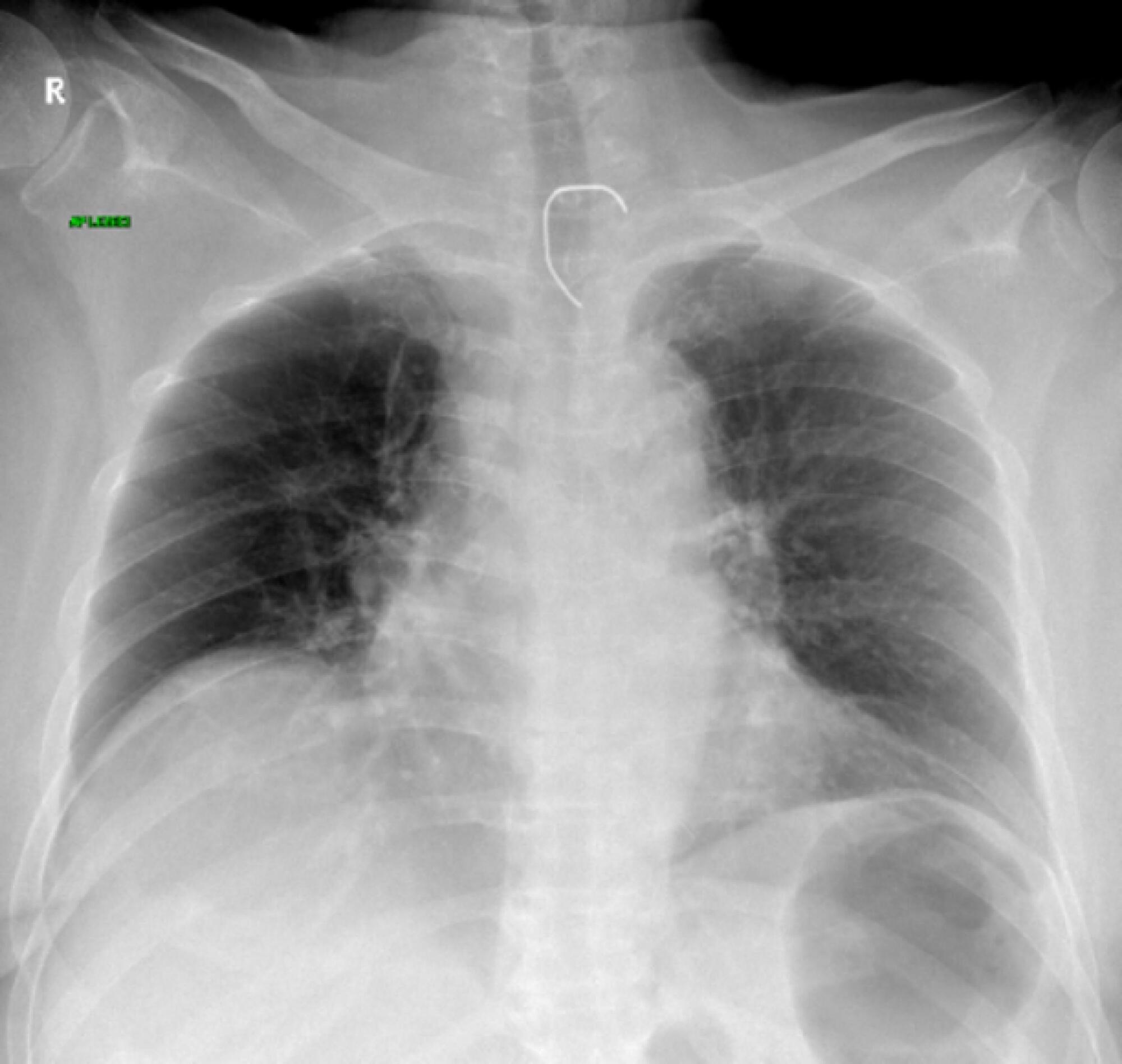
We present the case of a 71-year-old patient who was admitted to the medical intensive care unit in a state of multiple organ dysfunction. After the fourth day of applying all needed life-saving measures (vasopressor stimulation, mechanical ventilation, continuous dialysis treatment, broad spectrum antibiotic therapy, and other supportive measures), nonspecific heteroanamnestic data revealed that the patient had been having a persistent difficulty in swallowing liquids and food for a few days prior to hospital admission. After performing additional radiological and endoscopic diagnostic procedures, a foreign body was detected; a steel wire that had a length of approximately 6cm and was bent in a half had penetrated the esophagus and was projected into the seventh neckline. We managed to evacuate the foreign body endoscopically without further complications, and we stabilized our patient using additional therapeutic measures as needed.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):15-20
DOI 10.5935/0103-507X.20180001
To evaluate the frequency of intra-abdominal hypertension in major burn patients and its association with the occurrence of acute kidney injury.
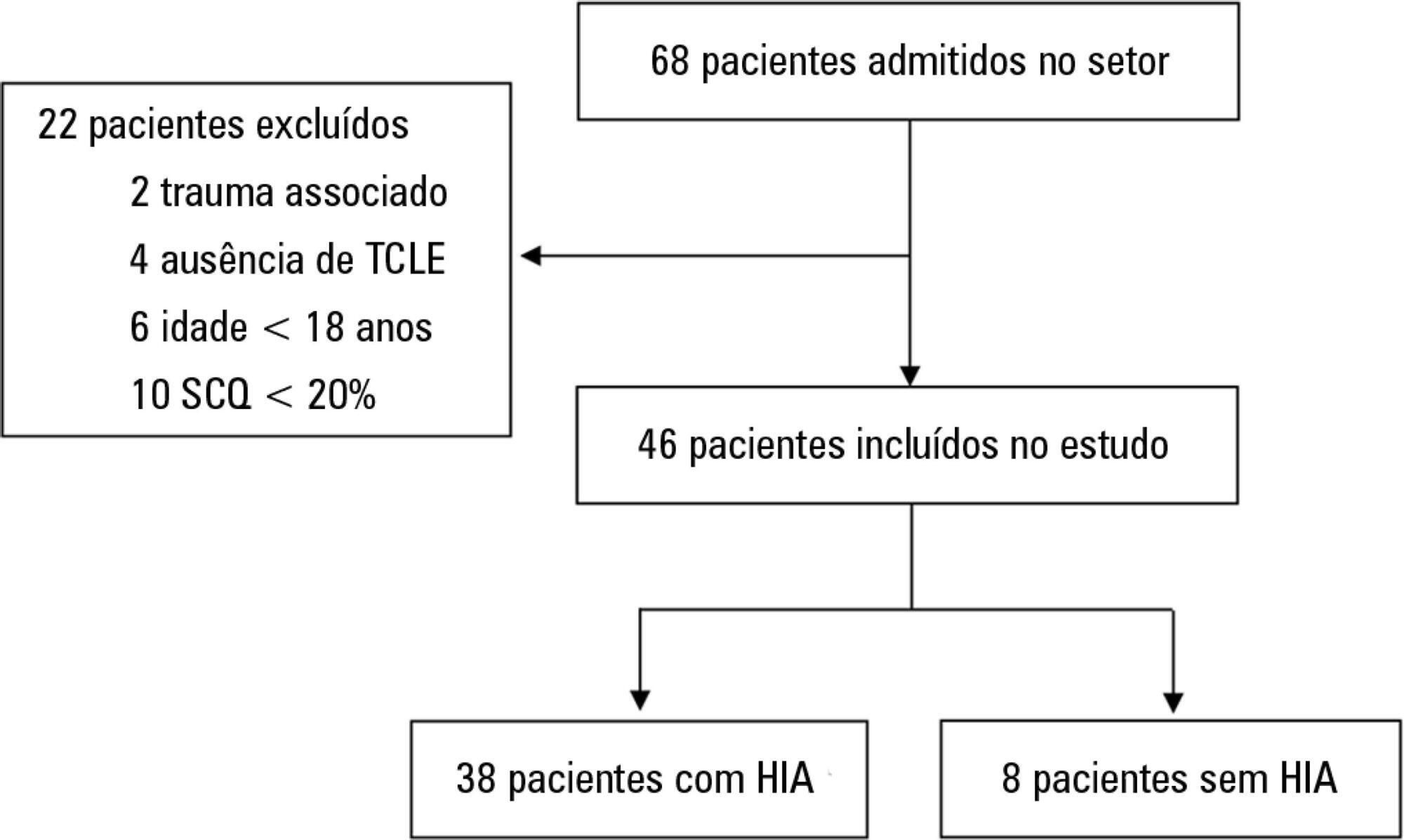
This was a prospective cohort study of a population of burn patients hospitalized in a specialized intensive care unit. A convenience sample was taken of adult patients hospitalized in the period from 1 August 2015 to 31 October 2016. Clinical and burn data were collected, and serial intra-abdominal pressure measurements taken. The significance level used was 5%.
A total of 46 patients were analyzed. Of these, 38 patients developed intra-abdominal hypertension (82.6%). The median increase in intra-abdominal pressure was 15.0mmHg (interquartile range: 12.0 to 19.0). Thirty-two patients (69.9%) developed acute kidney injury. The median time to development of acute kidney injury was 3 days (interquartile range: 1 - 7). The individual analysis of risk factors for acute kidney injury indicated an association with intra-abdominal hypertension (p = 0.041), use of glycopeptides (p = 0.001), use of vasopressors (p = 0.001) and use of mechanical ventilation (p = 0.006). Acute kidney injury was demonstrated to have an association with increased 30-day mortality (log-rank, p = 0.009).
Intra-abdominal hypertension occurred in most patients, predominantly in grades I and II. The identified risk factors for the occurrence of acute kidney injury were intra-abdominal hypertension and use of glycopeptides, vasopressors and mechanical ventilation. Acute kidney injury was associated with increased 30-day mortality.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):206-212
DOI 10.5935/0103-507X.20170029
To assess the frequency of primary multiple organ failure and the role of sepsis as a causative agent in critically ill pediatric patients; and calculate and evaluate the accuracy of the Pediatric Risk of Mortality III (PRISM III) and Pediatric Logistic Organ Dysfunction (PELOD) scores to predict the outcomes of critically ill children.
Retrospective study, which evaluated data from patients admitted from January to December 2011 in the pediatric intensive care unit of the Children's Hospital of the University of Cairo.
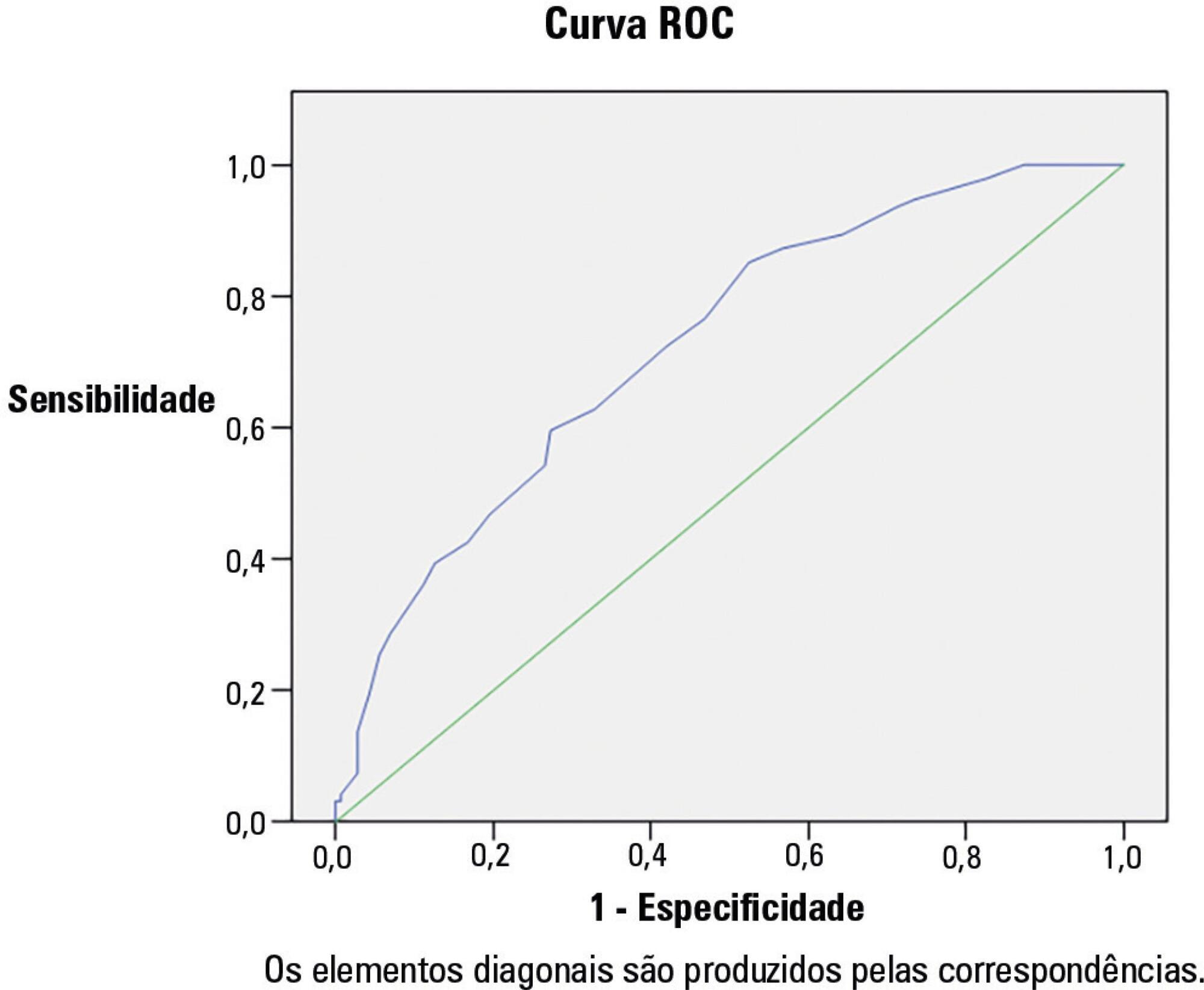
Out of 237 patients in the study, 72% had multiple organ dysfunctions, and 45% had sepsis with multiple organ dysfunctions. The mortality rate in patients with multiple organ dysfunction was 73%. Independent risk factors for death were mechanical ventilation and neurological failure [OR: 36 and 3.3, respectively]. The PRISM III score was more accurate than the PELOD score in predicting death, with a Hosmer-Lemeshow X2 (Chi-square value) of 7.3 (df = 8, p = 0.5). The area under the curve was 0.723 for PRISM III and 0.78 for PELOD.
A multiple organ dysfunctions was associated with high mortality. Sepsis was the major cause. Pneumonia, diarrhea and central nervous system infections were the major causes of sepsis. PRISM III had a better calibration than the PELOD for prognosis of the patients, despite the high frequency of the multiple organ dysfunction syndrome.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):178-184
DOI 10.5935/0103-507X.20150030
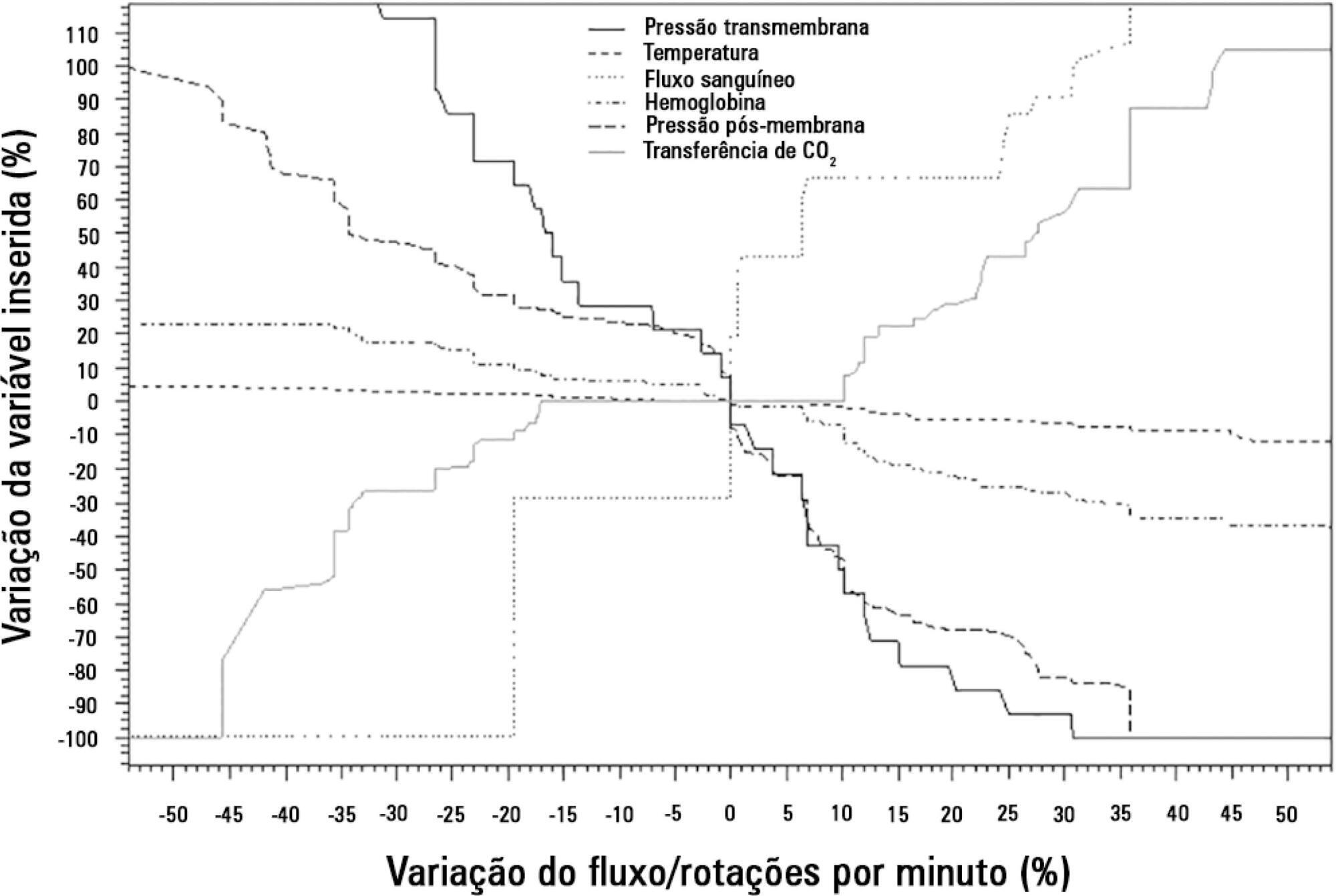
To analyze the correlations of the blood flow/pump rotation ratio and the transmembrane pressure, CO2 and O2 transfer during the extracorporeal respiratory support.
Five animals were instrumented and submitted to extracorporeal membrane oxygenation in a five-step protocol, including abdominal sepsis and lung injury.
This study showed that blood flow/pump rotations ratio variations are dependent on extracorporeal membrane oxygenation blood flow in a positive logarithmic fashion. Blood flow/pump rotation ratio variations are negatively associated with transmembrane pressure (R2 = 0.5 for blood flow = 1500mL/minute and R2 = 0.4 for blood flow = 3500mL/minute, both with p < 0.001) and positively associated with CO2 transfer variations (R2 = 0.2 for sweep gas flow ≤ 6L/minute, p < 0.001, and R2 = 0.1 for sweep gas flow > 6L/minute, p = 0.006), and the blood flow/pump rotation ratio is not associated with O2 transfer variations (R2 = 0.01 for blood flow = 1500mL/minute, p = 0.19, and R2 = - 0.01 for blood flow = 3500 mL/minute, p = 0.46).
Blood flow/pump rotation ratio variation is negatively associated with transmembrane pressure and positively associated with CO2 transfer in this animal model. According to the clinical situation, a decrease in the blood flow/pump rotation ratio can indicate artificial lung dysfunction without the occurrence of hypoxemia.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):148-154
DOI 10.5935/0103-507X.20140022
Patients with traumatic brain injury are particularly susceptible to sepsis, which may exacerbate the systemic inflammatory response and lead to organ dysfunction. The influence of clinical variables on the mortality of intensive care unit patients with traumatic brain injury and sepsis was investigated.
The present investigation was a retrospective study involving 175 patients with traumatic brain injury who were treated in a period of 1 year at a reference hospital for trauma and who had sepsis, severe sepsis, or septic shock. Demographic and clinical data were obtained, and the SOFA score was calculated at the time sepsis was found and after 72 hours.
There was a predominance of young men with severe traumatic brain injury, multiple head injuries, sepsis with a pulmonary focus, prolonged hospital stay, and high mortality (37.7%). Circulatory and respiratory failure had a high incidence, but renal and coagulation failure were less frequent, and liver failure was not observed. After logistic regression, the presence of septic shock and respiratory failure 72 hours after the sepsis diagnosis was associated with higher mortality, with an odds ratio of 7.56 (95%CI=2.04-27.31, p=0.0024) and 6.62 (95%CI=1.93-22.78, p=0.0027), respectively. In addition, there was a higher mortality among patients who had no organ failure on D1 but who developed the condition after 72 hours of sepsis and in those patients who already had organ failure at the time sepsis was diagnosed and remained in this condition after 72 hours.
Septic shock and progressive organ (particularly respiratory) dysfunction increases the mortality of patients with traumatic brain injury and sepsis.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):176-182
DOI 10.5935/0103-507X.20140026
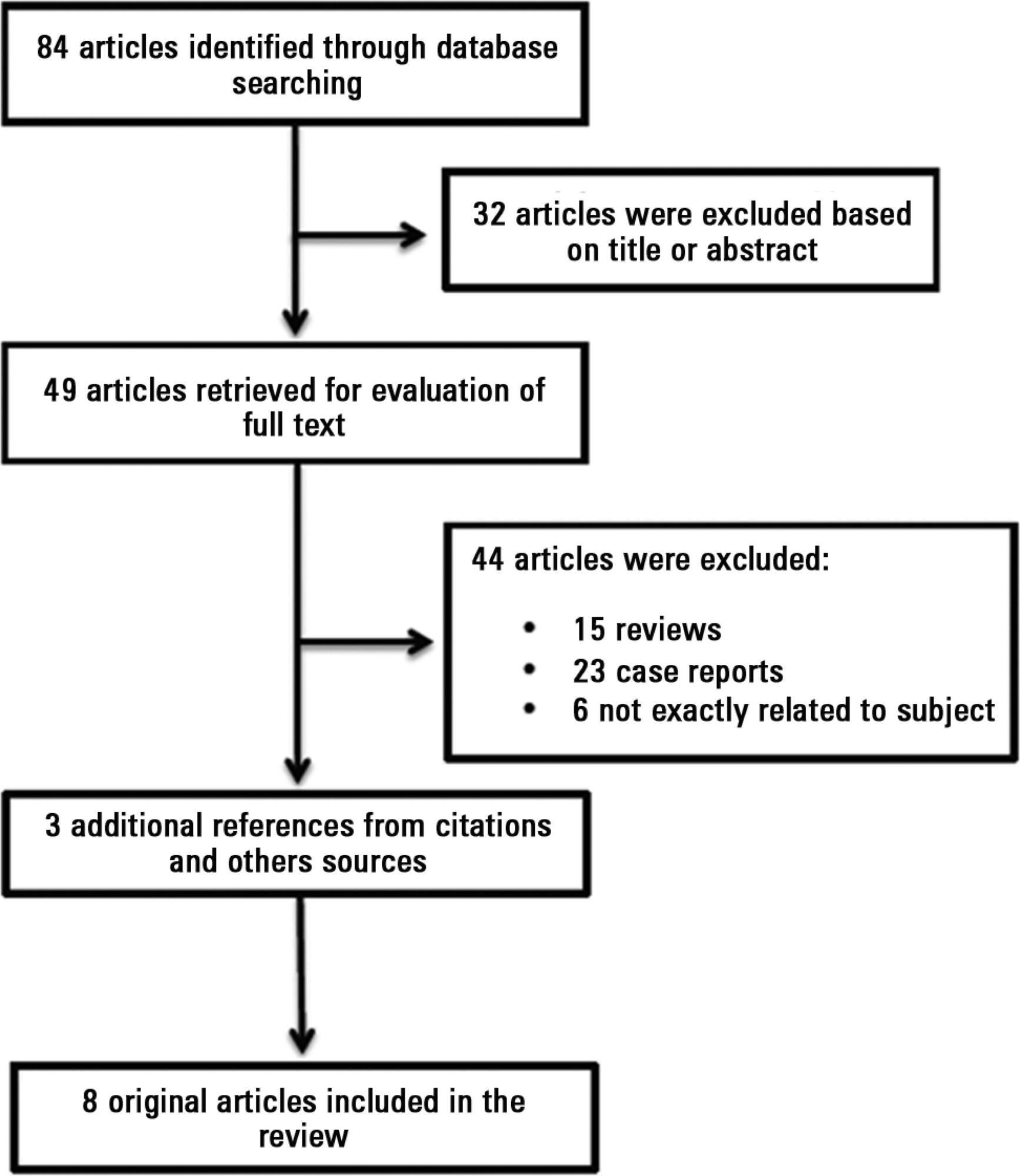
Antiphospholipid antibodies are responsible for a wide spectrum of clinical manifestations. Venous, arterial and microvascular thrombosis and severe catastrophic cases account for a large morbidly/mortality. Through the connection between the immune, inflammatory and hemostatic systems, it is possible that these antibodies may contribute to the development of organ dysfunction and are associated with poor short and long-term prognoses in critically ill patients. We performed a search of the PubMed/MedLine database for articles written during the period from January 2000 to February 2013 to evaluate the frequency of antiphospholipid antibodies in critically ill patients and their impact on the outcomes of these patients. Only eight original studies involving critically ill patients were found. However, the development of antiphospholipid antibodies in critically ill patients seems to be frequent, but more studies are necessary to clarify their pathogenic role and implications for clinical practice.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)