You searched for:"Rui Pereira"
We found (2) results for your search.-
Original Article
Acute-on-chronic liver failure syndrome – clinical results from an intensive care unit in a liver transplant center
Rev Bras Ter Intensiva. 2020;32(1):49-57
Abstract
Original ArticleAcute-on-chronic liver failure syndrome – clinical results from an intensive care unit in a liver transplant center
Rev Bras Ter Intensiva. 2020;32(1):49-57
DOI 10.5935/0103-507X.20200009
Views0ABSTRACT
Objective:
To characterize a cohort of acute-on-chronic liver failure patients in Intensive Care and to analyze the all-cause 28-day mortality risk factors assessed at ICU admission and day 3.
Methods:
This was a retrospective cohort study of consecutive patients admitted to the intensive care unit between March 2013 and December 2016.
Results:
Seventy-one patients were included. The median age was 59 (51 – 64) years, and 81.7% of patients were male. Alcohol consumption alone (53.5%) was the most frequent etiology of cirrhosis and infection (53.5%) was the most common acute-on-chronic liver failure precipitating event. At intensive care unit admission, the clinical severity scores were APACHE II 21 (16 – 23), CLIF-SOFA 13 (11 – 15), Child-Pugh 12 (10 – 13) and MELD 27 (20 – 32). The acute-on-chronic liver failure scores were no-acute-on-chronic liver failure: 11.3%; one: 14.1%; two: 28.2% and three: 46.5%; and the number of organ failures was one: 4.2%; two: 42.3%; three: 32.4%; four: 16.9%; and five: 4.2%. Liver transplantation was performed in 15.5% of patients. The twenty-eight-day mortality rate was 56.3%, and the in-ICU mortality rate was 49.3%. Organ failure at intensive care unit admission (p = 0.02; OR 2.1; 95%CI 1.2 – 3.9), lactate concentration on day 3 (p = 0.02; OR 6.3; 95%CI 1.4 – 28.6) and the international normalized ratio on day 3 (p = 0.03; OR 10.2; 95%CI 1.3 – 82.8) were independent risk factors.
Conclusion:
Acute-on-chronic liver failure patients presented with high clinical severity and mortality rates. The number of organ failures at intensive care unit admission and the lactate and international normalized ratio on day 3 were independent risk factors for 28-day mortality. We consider intensive care essential for acute-on-chronic liver failure patients and timely liver transplant was vital for selected patients.
Keywords:CirrhosisCritical illnessInternational normalized ratioLactateMultiple organ failureTreatment outcomeSee more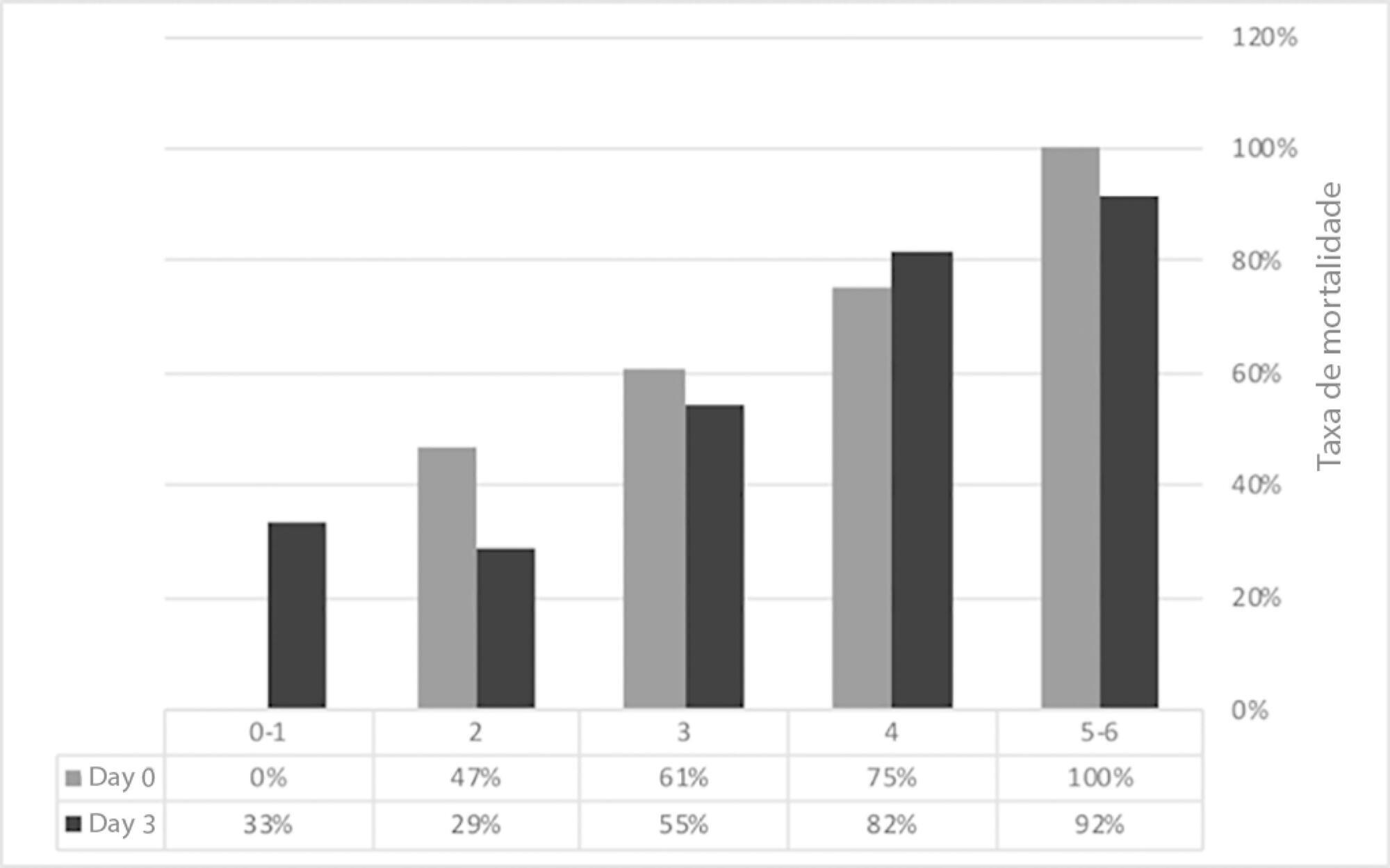
-
Review Articles
Approach to the liver transplant early postoperative period: an institutional standpoint
Rev Bras Ter Intensiva. 2019;31(4):561-570
Abstract
Review ArticlesApproach to the liver transplant early postoperative period: an institutional standpoint
Rev Bras Ter Intensiva. 2019;31(4):561-570
DOI 10.5935/0103-507X.20190076
Views0ABSTRACT
The liver transplant program in our center started in 1992, and post-liver transplant patients are still admitted to the intensive care unit. For the intensive care physician, a learning curve started then, skills were acquired, and a specific practice was established. Throughout this time, several concepts changed, improving the care of these patients. The practical approach varies between liver transplant centers, according to local specificities. Hence, we wanted to present our routine practice to stimulate the debate between dedicated teams, which can allow the introduction of new ideas and potentially improve each local standard of care.
Keywords:Intensive careLiver transplantationLiver/surgeryPerioperative period/adverse effectsPostoperative periodSee more
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




