Abstract
Crit Care Sci. 2023;35(4):377-385
DOI 10.5935/2965-2774.20230215-pt
To evaluate the occurrence of adverse events in the postoperative period of cardiac surgery in a pediatric intensive care unit and to find any patient characteristics that can predict such events.
This was a historical cohort study of patients recovering in the pediatric intensive care unit for the first 7 days after cardiac surgery between April and December 2019, by reviewing the medical records. The following were reviewed: demographic, clinical, and laboratory characteristics; patient severity scores; and selected adverse events, grouped into device-related, surgical, and nonsurgical.
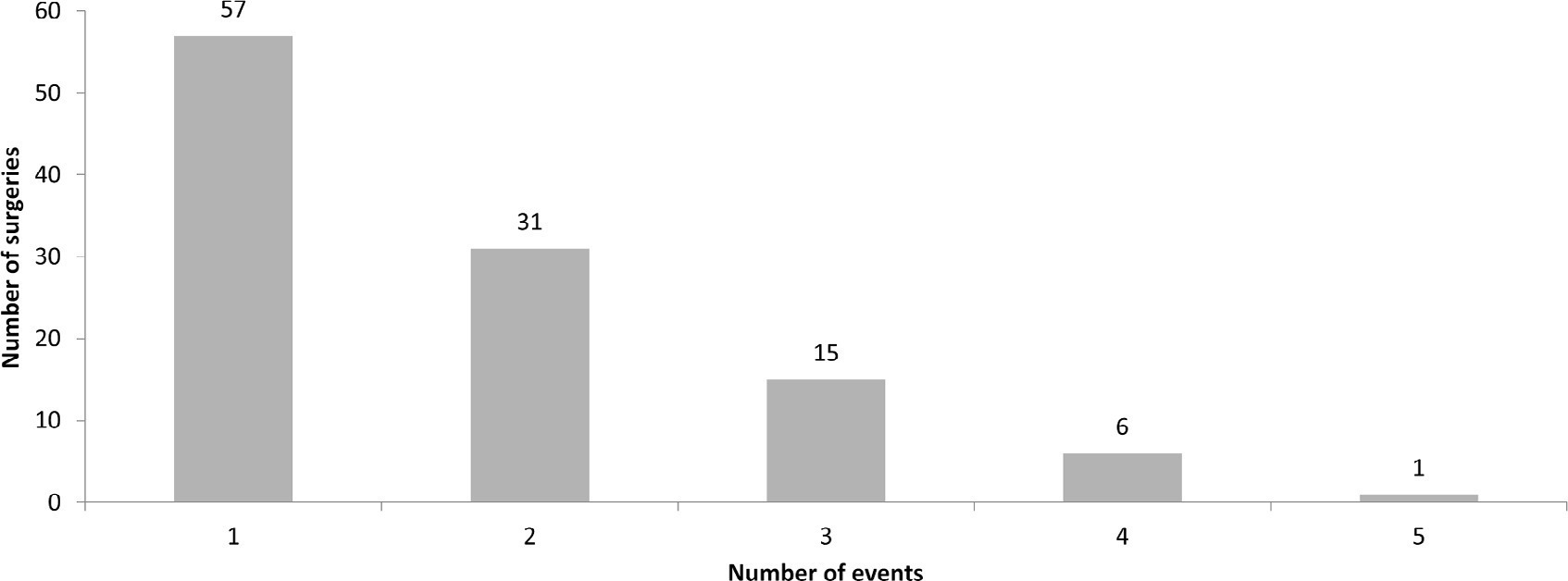
A total of 238 medical records were included. At least one adverse event occurred in 110 postoperative patients (46.2%). The total number of adverse events was 193 (81%). Vascular catheters were the most common cause, followed by cardiac arrest, bleeding, and surgical reexploration. In the univariate analysis, the vasoactive-inotropic score (VIS), Risk Adjustment in Congenital Heart Surgery (RACHS-1) score, age, Pediatric Index of Mortality (PIM-2), cardiopulmonary bypass and aortic clamping duration were significantly associated with adverse events. In the multivariate analysis, VIS ≥ 20 (OR 2.90; p = 0.004) and RACHS-1 ≥ 3 (OR 2.11; p = 0.019) were significant predictors, while age and delayed sternal closure showed only trends toward significance. To predict the occurrence of adverse events from VIS and RACHS-1, the area under the curve was 0.73 (95%CI 0.66 - 0.79).
Adverse events were quite frequent in children after cardiac surgery, especially those related to devices. The VIS and RACHS-1, used together, predicted the occurrence of adverse events well in this pediatric sample.
Abstract
Crit Care Sci. 2023;35(1):11-18
DOI 10.5935/2965-2774.20230336-pt
To explain the rationale and protocol of the methods and analyses to be used in the LIVER-PAM randomized clinical trial, which seeks to understand whether a higher mean arterial pressure is capable of reducing the incidence of renal dysfunction postoperatively after liver transplantation.
LIVER-PAM is an open-label, randomized, controlled, singlecenter clinical trial. Patients randomized to the intervention group will have a mean arterial pressure of 85 - 90mmHg in the initial 24 hours of postoperative management, while patients in the control group will have a mean arterial pressure of 65 - 70mmHg in the same period. A sample of 174 patients will be required to demonstrate a 20% reduction in the absolute incidence of renal dysfunction, with a power of 80% and an alpha of 0.05.
If a 20% reduction in the absolute incidence of renal dysfunction in the postoperative period of liver transplantation is achieved with higher target mean arterial pressure in the first 24 hours, this would represent an inexpensive and simple therapy for improving current outcomes in the management of liver transplant patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):561-570
DOI 10.5935/0103-507X.20190076
The liver transplant program in our center started in 1992, and post-liver transplant patients are still admitted to the intensive care unit. For the intensive care physician, a learning curve started then, skills were acquired, and a specific practice was established. Throughout this time, several concepts changed, improving the care of these patients. The practical approach varies between liver transplant centers, according to local specificities. Hence, we wanted to present our routine practice to stimulate the debate between dedicated teams, which can allow the introduction of new ideas and potentially improve each local standard of care.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):479-486
DOI 10.5935/0103-507X.20180069
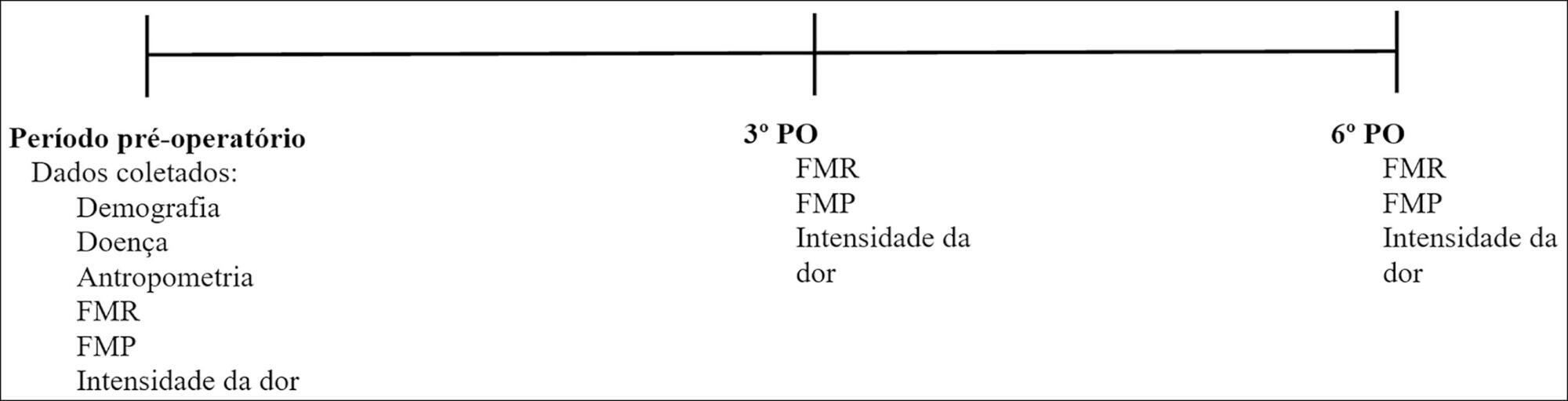
To evaluate respiratory and peripheral muscle strength after cardiac surgery. Additionally, we compared the changes in these variables on the third and sixth postoperative days.
Forty-six patients were recruited, including 17 women and 29 men, with a mean age of 60.50 years (SD = 9.20). Myocardial revascularization surgery was performed in 36 patients, replacement of the aortic valve in 5 patients, and replacement of the mitral valve in 5 patients.
A significant reduction in respiratory and peripheral muscle strength and a significant increase in pain intensity were observed on the third and sixth postoperative days (p < 0.05), except for the variable maximal inspiratory pressure; on the sixth postoperative day, maximal inspiratory pressure values were already similar to the preoperative and predicted values (p > 0.05). There was an association between peripheral muscle strength, specifically between maximal expiratory pressure preoperatively (rs = 0.383; p = 0.009), on the third postoperative day (rs = 0.468; p = 0.001) and on the sixth postoperative day (rs = 0.311; p = 0.037). The effect sizes were consistently moderate-to-large for respiratory muscle strength, the Medical Research Council scale and the visual analog scale, in particular between preoperative assessment and the sixth postoperative day.
There is a decrease in respiratory and peripheral muscle strength after cardiac surgery. In addition, maximal expiratory pressure is the variable that is most associated with peripheral muscle strength. These variables, especially respiratory and peripheral muscle strength, should be considered by professionals working in the intensive care setting.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):453-459
DOI 10.5935/0103-507X.20170069
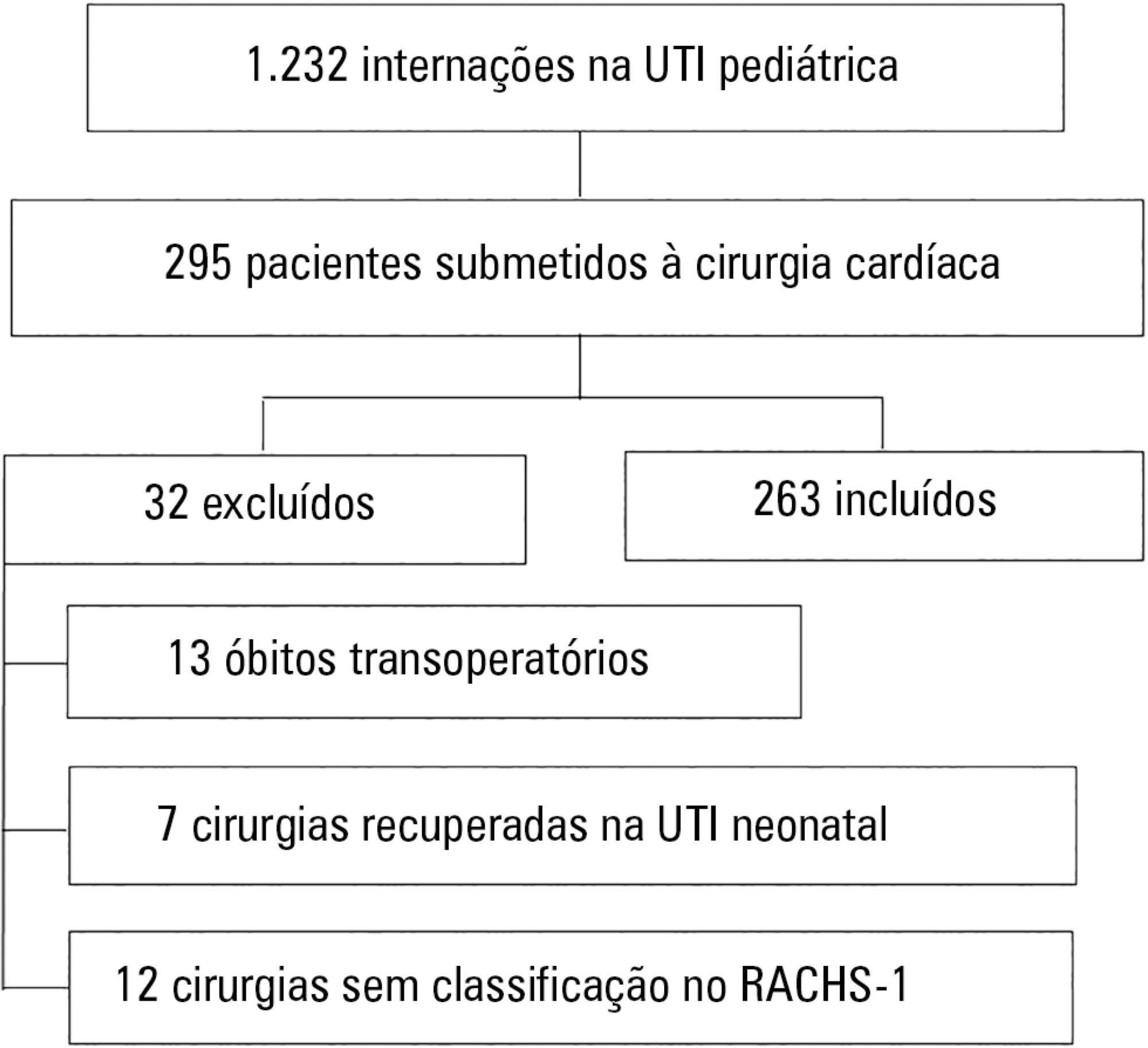
To assess the performance of the Pediatric Index of Mortality (PIM) 2 and the Risk Adjustment for Congenital Heart Surgery (RACHS) in the postoperative period of congenital heart disease patients.
Retrospective cross-sectional study. Data were collected from patient records to generate the scores and predictions using recommended techniques, demographic data and outcomes. The Mann-Whitney test, Hosmer-Lemeshow test, standardized mortality rate, area under the receiver operating characteristic (ROC) curve, chi square test, Poisson regression with robust variance and Spearman's test were used for statistical analysis.
A total of 263 patients were evaluated, and 72 died (27.4%). These patients presented significantly higher PIM-2 values than survivors (p < 0.001). In the RACHS-1 classification, mortality was progressively higher according to the complexity of the procedure, with a 3.24-fold increase in the comparison between groups 6 and 2. The area under the ROC curve for PIM-2 was 0.81 (95%CI 0.75 - 0.87), while for RACHS-1, it was 0.70 (95%CI 0.63 - 0.77). The RACHS presented better calibration power in the sample analyzed. A significantly positive correlation was found between the results of both scores (rs = 0.532; p < 0.001).
RACHS presented good calibration power, and RACHS-1 and PIM-2 demonstrated good performance with regard to their discriminating capacities between survivors and non-survivors. Moreover, a positive correlation was found between the results of the two risk scores.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):18-25
DOI 10.5935/0103-507X.20150005
To evaluate and compare stressors identified by patients of a coronary intensive care unit with those perceived by patients of a general postoperative intensive care unit.
This cross-sectional and descriptive study was conducted in the coronary intensive care and general postoperative intensive care units of a private hospital. In total, 60 patients participated in the study, 30 in each intensive care unit. The stressor scale was used in the intensive care units to identify the stressors. The mean score of each item of the scale was calculated followed by the total stress score. The differences between groups were considered significant when p < 0.05.
The mean ages of patients were 55.63 ± 13.58 years in the coronary intensive care unit and 53.60 ± 17.47 years in the general postoperative intensive care unit. For patients in the coronary intensive care unit, the main stressors were “being in pain”, “being unable to fulfill family roles” and “being bored”. For patients in the general postoperative intensive care unit, the main stressors were “being in pain”, “being unable to fulfill family roles” and “not being able to communicate”. The mean total stress scores were 104.20 ± 30.95 in the coronary intensive care unit and 116.66 ± 23.72 (p = 0.085) in the general postoperative intensive care unit. When each stressor was compared separately, significant differences were noted only between three items. “Having nurses constantly doing things around your bed” was more stressful to the patients in the general postoperative intensive care unit than to those in the coronary intensive care unit (p = 0.013). Conversely, “hearing unfamiliar sounds and noises” and “hearing people talk about you” were the most stressful items for the patients in the coronary intensive care unit (p = 0.046 and 0.005, respectively).
The perception of major stressors and the total stress score were similar between patients in the coronary intensive care and general postoperative intensive care units.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):105-112
DOI 10.5935/0103-507X.20150020
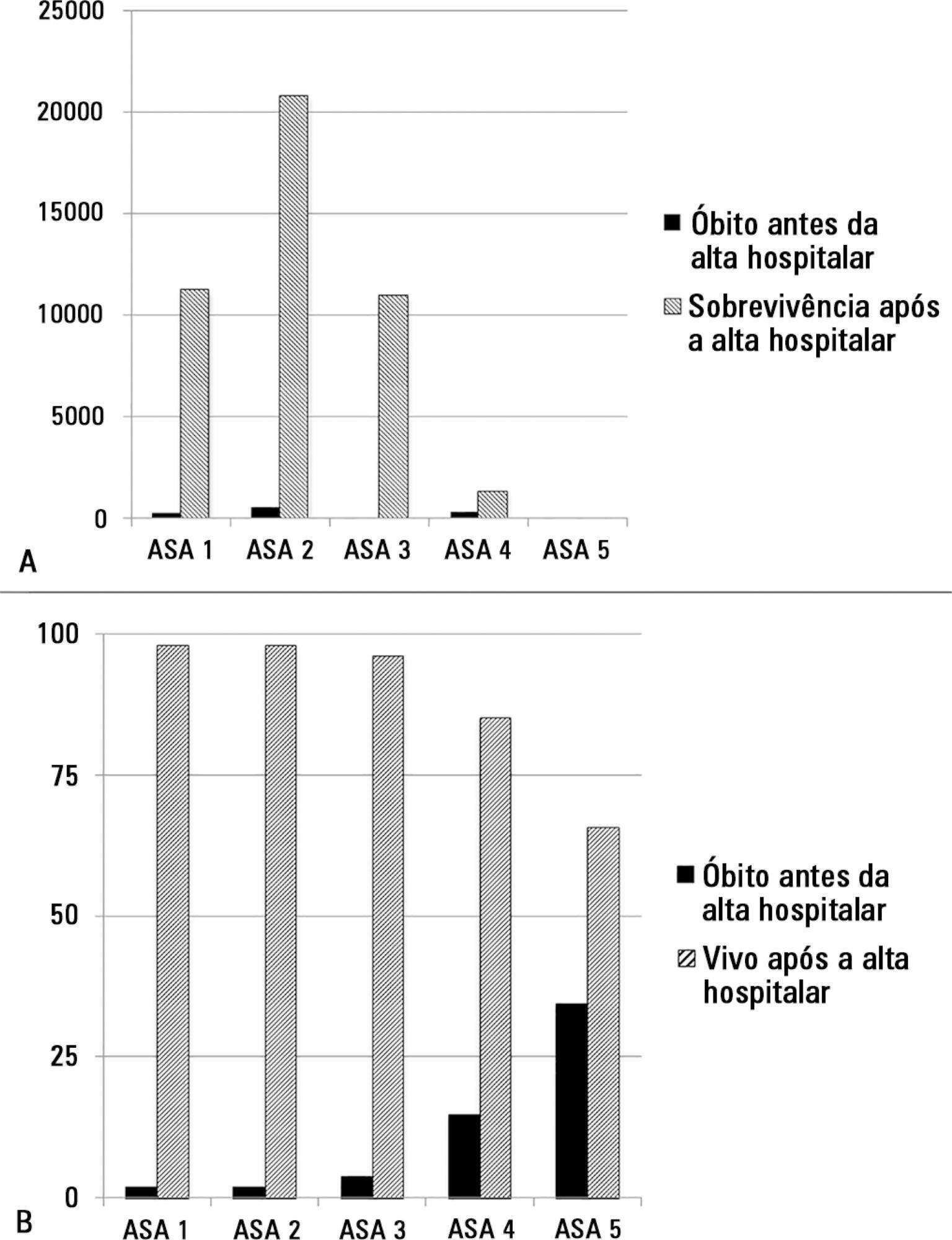
The European Surgical Outcomes Study described mortality following in-patient surgery. Several factors were identified that were able to predict poor outcomes in a multivariate analysis. These included age, procedure urgency, severity and type and the American Association of Anaesthesia score. This study describes in greater detail the relationship between the American Association of Anaesthesia score and postoperative mortality.
Patients in this 7-day cohort study were enrolled in April 2011. Consecutive patients aged 16 years and older undergoing inpatient non-cardiac surgery with a recorded American Association of Anaesthesia score in 498 hospitals across 28 European nations were included and followed up for a maximum of 60 days. The primary endpoint was in-hospital mortality. Decision tree analysis with the CHAID (SPSS) system was used to delineate nodes associated with mortality.
The study enrolled 46,539 patients. Due to missing values, 873 patients were excluded, resulting in the analysis of 45,666 patients. Increasing American Association of Anaesthesia scores were associated with increased admission rates to intensive care and higher mortality rates. Despite a progressive relationship with mortality, discrimination was poor, with an area under the ROC curve of 0.658 (95% CI 0.642 - 0.6775). Using regression trees (CHAID), we identified four discrete American Association of Anaesthesia nodes associated with mortality, with American Association of Anaesthesia 1 and American Association of Anaesthesia 2 compressed into the same node.
The American Association of Anaesthesia score can be used to determine higher risk groups of surgical patients, but clinicians cannot use the score to discriminate between grades 1 and 2. Overall, the discriminatory power of the model was less than acceptable for widespread use.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)