You searched for:"Rui Paulo Moreno"
We found (4) results for your search.-
Original Articles
American Society of Anesthesiologists Score: still useful after 60 years? Results of the EuSOS Study
Rev Bras Ter Intensiva. 2015;27(2):105-112
Abstract
Original ArticlesAmerican Society of Anesthesiologists Score: still useful after 60 years? Results of the EuSOS Study
Rev Bras Ter Intensiva. 2015;27(2):105-112
DOI 10.5935/0103-507X.20150020
Views0See moreABSTRACT
Objective:
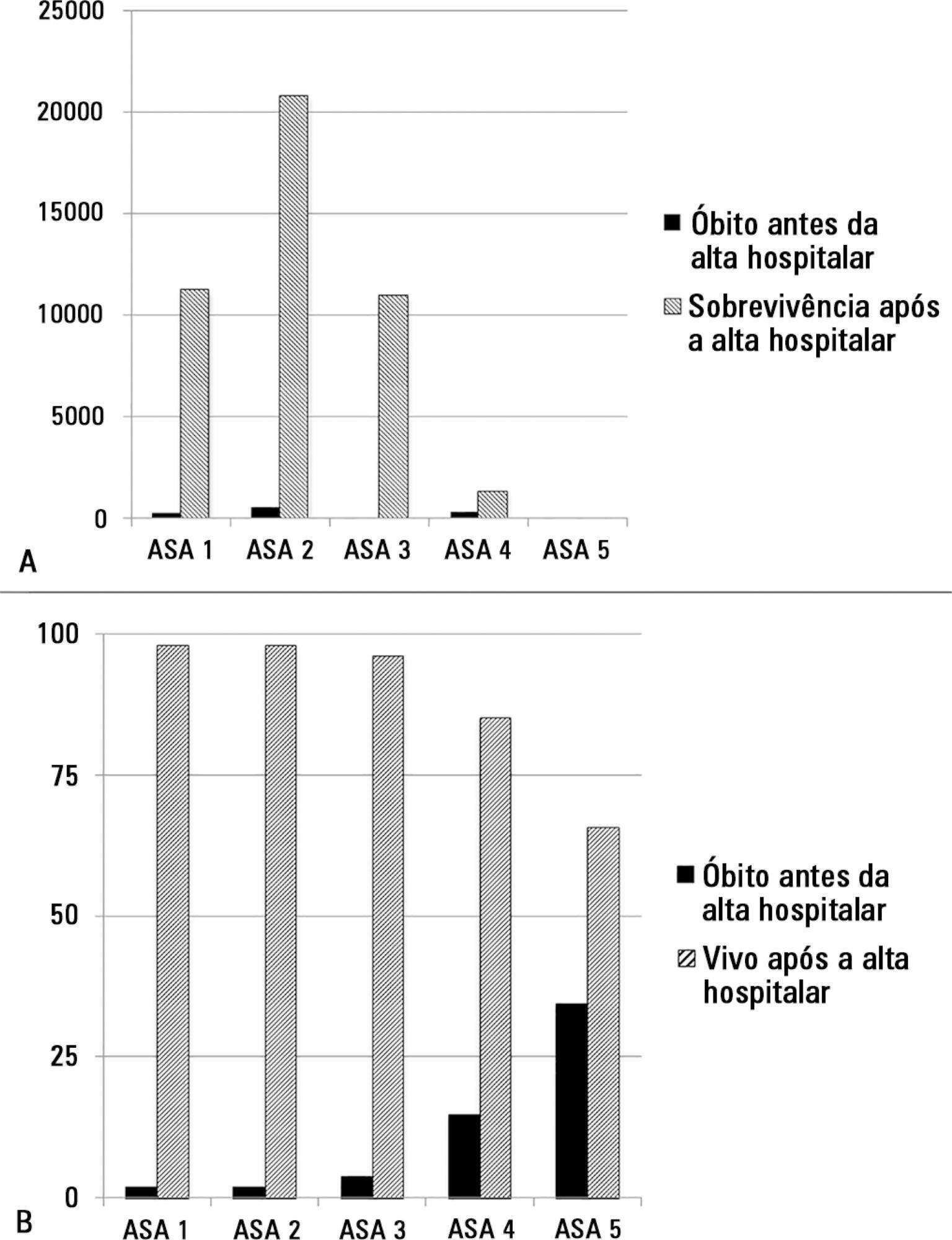
The European Surgical Outcomes Study described mortality following in-patient surgery. Several factors were identified that were able to predict poor outcomes in a multivariate analysis. These included age, procedure urgency, severity and type and the American Association of Anaesthesia score. This study describes in greater detail the relationship between the American Association of Anaesthesia score and postoperative mortality.
Methods:
Patients in this 7-day cohort study were enrolled in April 2011. Consecutive patients aged 16 years and older undergoing inpatient non-cardiac surgery with a recorded American Association of Anaesthesia score in 498 hospitals across 28 European nations were included and followed up for a maximum of 60 days. The primary endpoint was in-hospital mortality. Decision tree analysis with the CHAID (SPSS) system was used to delineate nodes associated with mortality.
Results:
The study enrolled 46,539 patients. Due to missing values, 873 patients were excluded, resulting in the analysis of 45,666 patients. Increasing American Association of Anaesthesia scores were associated with increased admission rates to intensive care and higher mortality rates. Despite a progressive relationship with mortality, discrimination was poor, with an area under the ROC curve of 0.658 (95% CI 0.642 – 0.6775). Using regression trees (CHAID), we identified four discrete American Association of Anaesthesia nodes associated with mortality, with American Association of Anaesthesia 1 and American Association of Anaesthesia 2 compressed into the same node.
Conclusion:
The American Association of Anaesthesia score can be used to determine higher risk groups of surgical patients, but clinicians cannot use the score to discriminate between grades 1 and 2. Overall, the discriminatory power of the model was less than acceptable for widespread use.
-
Review Articles
Delirium in intensive care: an under-diagnosed reality
Rev Bras Ter Intensiva. 2013;25(2):137-147
Abstract
Review ArticlesDelirium in intensive care: an under-diagnosed reality
Rev Bras Ter Intensiva. 2013;25(2):137-147
DOI 10.5935/0103-507X.20130025
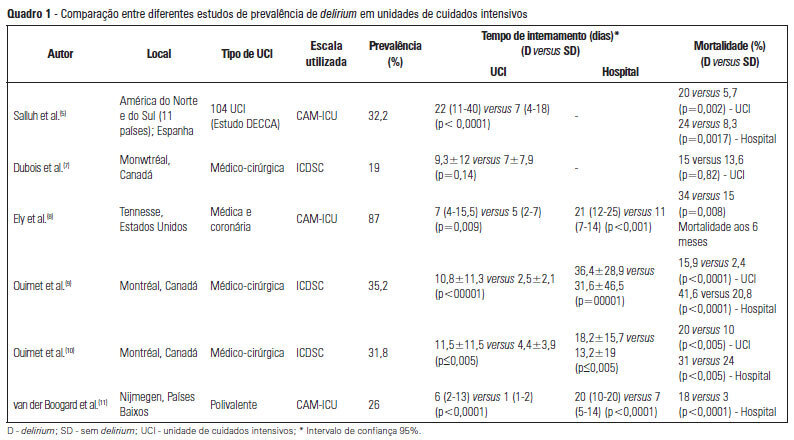
Views0See moreDelirium occurs in up to 80% of patients admitted to intensive care units. Although under-diagnosed, delirium is associated with a significant increase in morbidity and mortality in critical patients. Here, we review the main risk factors, clinical manifestations and preventative and therapeutic approaches (pharmacological and non-pharmacological) for this illness.
-
Special Article
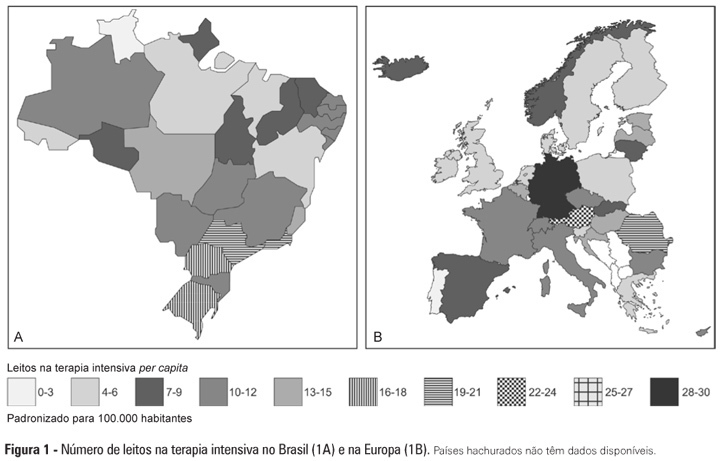
Intensive care provision: a global problem
Rev Bras Ter Intensiva. 2012;24(4):322-325
Abstract
-
Original Articles – Clinical Research
Mortality assessment in patients with severe acute pancreatitis: a comparative study of specific and general severity indices
Rev Bras Ter Intensiva. 2012;24(3):246-251
Abstract
Original Articles – Clinical ResearchMortality assessment in patients with severe acute pancreatitis: a comparative study of specific and general severity indices
Rev Bras Ter Intensiva. 2012;24(3):246-251
DOI 10.1590/S0103-507X2012000300007
Views0OBJECTIVE: This study compared the general and specific severity indices to assess the prognosis of severe acute pancreatitis at a polyvalent intensive care unit. METHODS: This retrospective study included 108 patients who were diagnosed with severe acute pancreatitis from July 1, 1999 to March 31, 2012. Their demographic and clinical data were collected, and the following severity indices were calculated: Ranson, Osborne, Blamey and Imrie, Balthazar, POP, APACHE II, SAPS II, and SOFA. The discriminative power of these indices with regard to mortality at the intensive care unit and hospital was assessed using the area under the ROC curve. RESULTS: The demographic data of the surviving and deceased patients did not significantly differ at baseline. The mortality rates were 27% and 39% at the intensive care unit and hospital, respectively. The severity indices that exhibited the greatest discriminative power with regard to mortality at the intensive care unit and hospital were the POP 0, POP 24, SOFA (at admission, 24 hours, 48 hours, and discharge), SAPS II, and APACHE II. CONCLUSION: The POP performed better than the other indices (aROC>0.8) at admission and 24 hours later (as originally described). The general physiological dysfunction indices also exhibited reasonable discriminative power (aROC=0.75-0.8), which was unlike the remaining pancreatitis specific indices, whose discriminative power was lower.
Keywords:Acute pancreatitisCritical careHospital mortalityMortalityPrognosisSeverity of illness indexSee more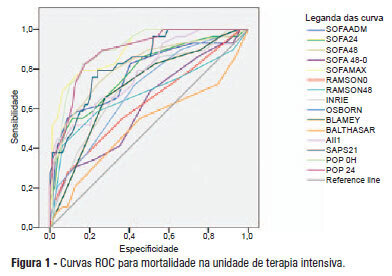
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




