Abstract
Crit Care Sci. 2023;35(1):11-18
DOI 10.5935/2965-2774.20230336-pt
To explain the rationale and protocol of the methods and analyses to be used in the LIVER-PAM randomized clinical trial, which seeks to understand whether a higher mean arterial pressure is capable of reducing the incidence of renal dysfunction postoperatively after liver transplantation.
LIVER-PAM is an open-label, randomized, controlled, singlecenter clinical trial. Patients randomized to the intervention group will have a mean arterial pressure of 85 - 90mmHg in the initial 24 hours of postoperative management, while patients in the control group will have a mean arterial pressure of 65 - 70mmHg in the same period. A sample of 174 patients will be required to demonstrate a 20% reduction in the absolute incidence of renal dysfunction, with a power of 80% and an alpha of 0.05.
If a 20% reduction in the absolute incidence of renal dysfunction in the postoperative period of liver transplantation is achieved with higher target mean arterial pressure in the first 24 hours, this would represent an inexpensive and simple therapy for improving current outcomes in the management of liver transplant patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):561-570
DOI 10.5935/0103-507X.20190076
The liver transplant program in our center started in 1992, and post-liver transplant patients are still admitted to the intensive care unit. For the intensive care physician, a learning curve started then, skills were acquired, and a specific practice was established. Throughout this time, several concepts changed, improving the care of these patients. The practical approach varies between liver transplant centers, according to local specificities. Hence, we wanted to present our routine practice to stimulate the debate between dedicated teams, which can allow the introduction of new ideas and potentially improve each local standard of care.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):57-62
DOI 10.5935/0103-507X.20190016
To assess the Perme mobility scale score as a predictor of functional status and complications in the postoperative period in patients undergoing liver transplantation.
The sample consisted of 30 patients who underwent liver transplantation. The patients were evaluated at two time points to determine their perception of pain, degree of dyspnea, peripheral muscle strength, and functional status according to the Perme scale. The collected data were analyzed by descriptive and inferential statistics. To compare the means between the evaluations, Student's t test for paired samples was applied. In case of asymmetry, the Wilcoxon test was used. In the evaluation of the association between the quantitative variables, the Pearson or Spearman correlation tests were applied.
A total of 30 individuals who underwent liver transplantation were included. The patients were predominantly male, and the mean age was 58.4 ± 9.9 years. The most prevalent underlying pathology was cirrhosis C virus (23.3%). Significant associations of the time on mechanical ventilation with the Perme scale score at discharge from the intensive care unit (r = -0.374; p = 0.042) and the number of physical therapy treatments (r = -0.578; p = 0.001) were recorded. When comparing the results of the initial evaluation and the evaluation at hospital discharge, there was a significant improvement in functional status (p < 0.001).
Functional mobility, peripheral muscle strength, pain perception, and dyspnea are significantly improved at hospital discharge compared with those at inpatient unit admission.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):64-70
DOI 10.5935/0103-507X.20180012
To describe a cohort of patients with acute liver failure and to analyze the demographic and clinical factors associated with mortality.
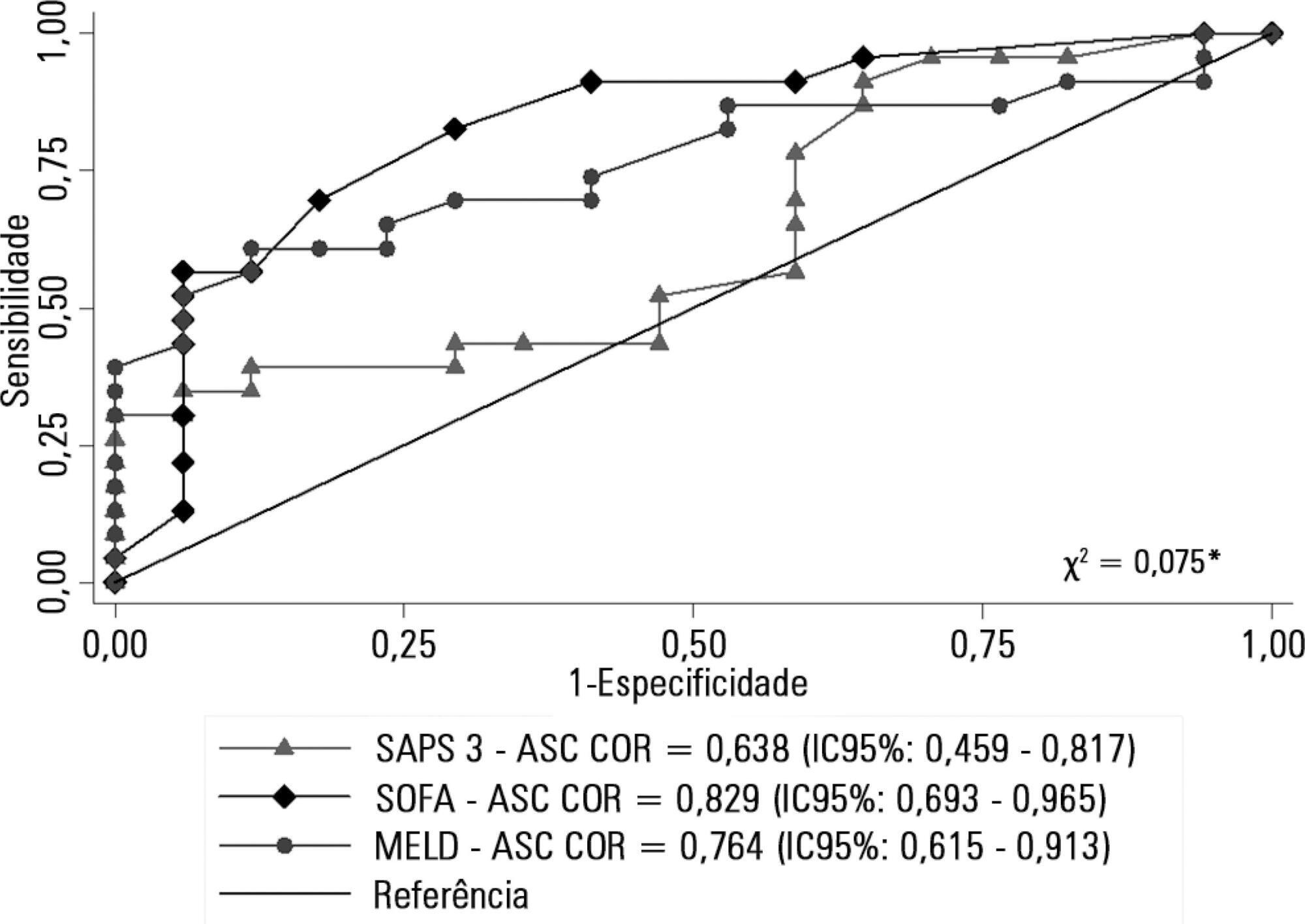
Retrospective cohort study in which all patients admitted for acute liver failure from July 28, 2012, to August 31, 2017, were included. Clinical and demographic data were collected using the Epimed System. The SAPS 3, SOFA, and MELD scores were measured. The odds ratios and 95% confidence intervals were estimated. Receiver operating characteristics curves were obtained for the prognostic scores, along with the Kaplan-Meier survival curve for the score best predicting mortality.
The majority of the 40 patients were female (77.5%), and the most frequent etiology was hepatitis B (n = 13). Only 35% of the patients underwent liver transplantation. The in-hospital mortality rate was 57.5% (95%CI: 41.5 - 73.5). Among the scores investigated, only SOFA remained associated with risk of death (OR = 1.37; 95%CI 1.11 - 1.69; p < 0.001). After SOFA stratification into < 12 and ≥ 12 points, survival was higher in patients with SOFA <12 (log-rank p < 0.001).
SOFA score in the first 24 hours was the best predictor of fatal outcome.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):233-236
DOI 10.5935/0103-507X.20180029
We report the case of a female patient, 58 years of age, without known heart disease, who underwent liver transplantation without complications. On the second postoperative day, the patient developed cardiogenic shock secondary to stress-induced cardiomyopathy (Takotsubo-like syndrome). The patient was successfully managed with veno-arterial peripheral extracorporeal membrane oxygenation for 6 days, with complete recovery of cardiac function and of the hepatic graft. Coronary syndrome and acute myocarditis were excluded as the causes of the shock. The use of extracorporeal membrane oxygenation in this scenario is possible and safe, considering its specialized protocols and treatment.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):161-166
DOI 10.5935/0103-507X.20160031
To correlate the levels of thrombin activatable fibrinolysis inhibitor in the immediate postoperative period and at 24 hours postoperatively with the volume of intraoperative bleeding.
Twenty-one patients allocated immediately before (elective or emergency) liver transplantation were analyzed. Blood samples were collected for thrombin activatable fibrinolysis inhibitor analysis at three different time points: immediately before liver transplantation (preoperative thrombin activatable fibrinolysis inhibitor), immediately after the surgical procedure (immediate postoperative thrombin activatable fibrinolysis inhibitor), and 24 hours after surgery (thrombin activatable fibrinolysis inhibitor 24 hours after surgery). The primary outcome of the study was to correlate the preoperative and immediate postoperative levels of thrombin activatable fibrinolysis inhibitor with intraoperative blood loss.
There was a correlation between the preoperative thrombin activatable fibrinolysis inhibitor levels and bleeding volume (ρ = -0.469; p = 0.05) but no correlation between the immediate postoperative thrombin activatable fibrinolysis inhibitor and bleeding volume (ρ = -0.062; p = 0.79). No variable included in the linear regression analysis (prehemoglobin, prefibrinogen and preoperative thrombin activatable fibrinolysis inhibitor) was a bleeding predictor. There was a similar trend in the variation between the levels of thrombin activatable fibrinolysis inhibitor at the three different time points and fibrinogen levels. Patients who died within 6 months (14.3%) showed decreased preoperative and immediate postoperative levels of thrombin activatable fibrinolysis compared with survivors (preoperative: 1.3 ± 0.15 versus 2.55 ± 0.53, p = 0.06; immediate postoperative: 1.2 ± 0.15 versus 2.5 ± 0.42, p = 0.007).
There was a moderate correlation between preoperative thrombin activatable fibrinolysis inhibitor and intraoperative bleeding in liver transplantation patients, although the predictive role of this variable independent of other variables remains uncertain. Preoperative and immediate postoperative thrombin activatable fibrinolysis inhibitor levels may have a role in the survival prognosis of this population; however, this possibility requires confirmation in further studies with larger sample sizes.
Abstract
Rev Bras Ter Intensiva. 2009;21(2):226-230
DOI 10.1590/S0103-507X2009000200017
Pulmonary artery catheter is frequently used to monitor patients during liver transplantation. Recently developed less invasive methods for estimating cardiac output and pulmonary capillary wedge pressure together with the failure of randomized studies to demonstrate reduced mortality in pulmonary artery catheter-monitored patients, has restricted its applicability. Pulmonary artery rupture by pulmonary artery catheter is a rare, but dangerous complication. The purpose of this report is to describe a pulmonary artery rupture caused by monitorization with a pulmonary artery catheter, reviewing the clinical approach and discussing hemodynamic monitoring with the pulmonary artery catheter during liver transplantation. A 56 year old female patient, with cirrhosis caused by hepatitis C virus (MELD score 26) presented with acute hepatic encephalopathy. She was medicated and received a liver transplantation with invasive monitoring with a pulmonary artery catheter. In the first 24 hours after surgery, the patient presented with hemodynamic instability, low hematocrit, and cardiorespiratory arrest. After cardiopulmonary resuscitation, hemopericardium was diagnosed by transthoracic echocardiography and even after pericardiocentesis the patient developed recurrent hemopericardium. Pulmonary angiography did not disclose large vessellesions. The pulmonary artery rupture diagnosis was only made after sternotomy and direct lesion observation. Complications from use of pulmonary artery catheter are infrequent, however, due to their clinical severity, can cause high morbidity and mortality. A decreased use of pulmonary artery catheter reduced the number of complications observed. New clinical studies comparing pulmonary artery catheter with non-invasive methods for pulmonary capillary wedge pressure measurement must be conducted in liver transplantation.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)