Abstract
Rev Bras Ter Intensiva. 2019;31(4):582-585
DOI 10.5935/0103-507X.20190075
We present the case of a 71-year-old patient who was admitted to the medical intensive care unit in a state of multiple organ dysfunction. After the fourth day of applying all needed life-saving measures (vasopressor stimulation, mechanical ventilation, continuous dialysis treatment, broad spectrum antibiotic therapy, and other supportive measures), nonspecific heteroanamnestic data revealed that the patient had been having a persistent difficulty in swallowing liquids and food for a few days prior to hospital admission. After performing additional radiological and endoscopic diagnostic procedures, a foreign body was detected; a steel wire that had a length of approximately 6cm and was bent in a half had penetrated the esophagus and was projected into the seventh neckline. We managed to evacuate the foreign body endoscopically without further complications, and we stabilized our patient using additional therapeutic measures as needed.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):586-591
DOI 10.5935/0103-507X.20190068
Among the infections caused by Streptococcus β hemolyticus from the Lancefield serogroup A, toxic shock syndrome is perhaps the most severe, and its mortality rate is high. Its clinical similarity to other forms of shock, especially septic shock, can often confuse the evaluator and interfere with the selection of the most appropriate therapy. This report aims to inform readers of the need to add this syndrome as a differential diagnosis in cases of shock, especially those with no well-defined clinical manifestations. For this purpose, we present the case of an infant with common flu-like symptoms who progressed rapidly with a rash, a reduced level of consciousness and clinical and laboratory signs of shock that required intensive support. In addition to cultures indicating the etiological agent, the appearance of exanthema and necrotizing fasciitis led to the diagnosis. However, less than 50% of cases present classic clinical signs of this entity. Penicillins combined with aminoglycosides are still the therapy of choice and are supported by a high level of evidence. Despite the severity of this patient's presentation, the progression was satisfactory.

Abstract
Rev Bras Ter Intensiva. 2018;30(1):121-126
DOI 10.5935/0103-507X.20180018
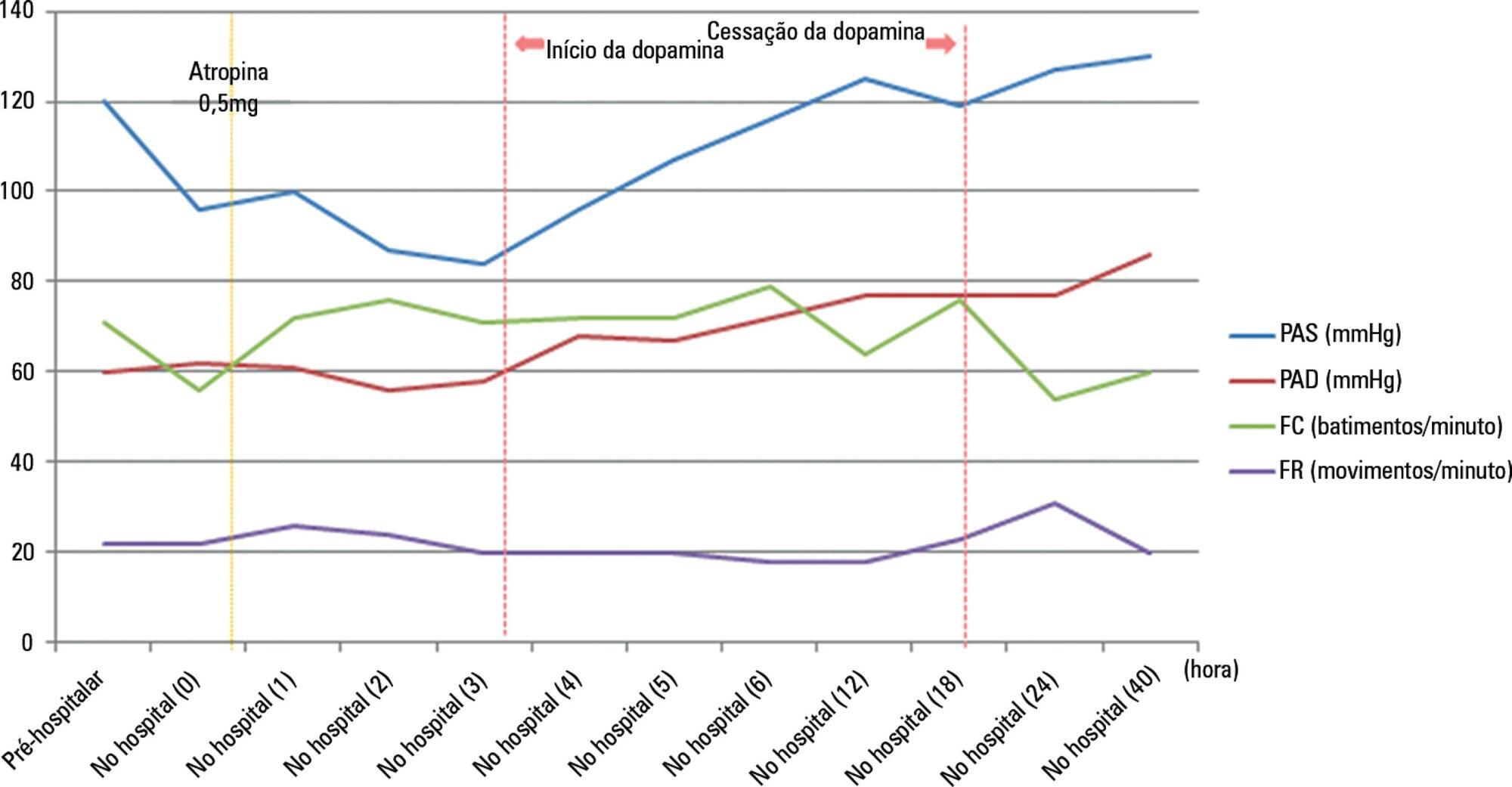
Nicotine is a dangerous substance extracted from tobacco leaves. When nicotine is absorbed in excessive amounts, it can lead to respiratory failure and cardiac arrest. The commercialization of electronic cigarettes (e-cigarettes) has allowed users to directly handle e-cigarette liquid. Consequently, the risk of liquid nicotine exposure has increased. We describe our experience of managing the case of a patient who orally ingested a high concentration of liquid nicotine from e-cigarette liquid. The patient presented with bradycardia and hypotension, which are symptoms of parasympathetic stimulation, together with impaired consciousness. He recovered following treatment with atropine and a vasopressor.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):127-130
DOI 10.5935/0103-507X.20180019
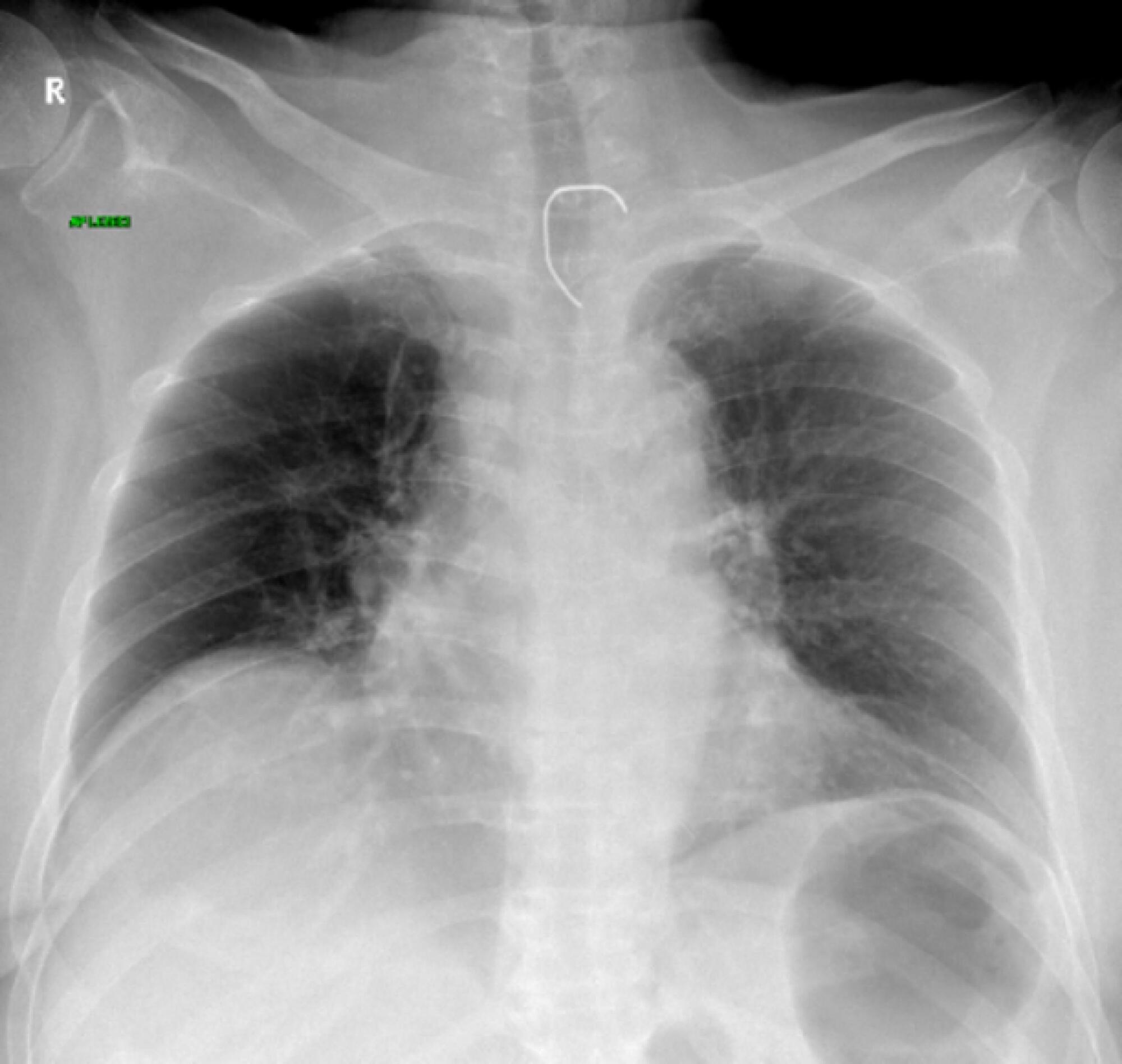
In the 2014 - 2015 season, most influenza infections were due to A (H3N2) viruses. More than two-thirds of circulating A (H3N2) viruses are antigenically and genetically different (drifted) from the A (H3N2) vaccine component of 2014 - 2015 northern and southern Hemisphere seasonal influenza vaccines. The purpose of this paper is to report a case of seasonal influenza A non-H1N1 infection that occurred in June 2015 in an adult cystic fibrosis patient with severe lung disease previously vaccinated with the anti-flu trivalent vaccine. The patient evolved to respiratory and renal failure (without rhabdomyolysis) and was placed under mechanical ventilation and hemodialysis. The clinical outcome was positive after 39 days of hospital stay. In addition, the patient was clinically stable after 18 months of follow-up. With the recent advances in critical care medicine and in cystic fibrosis treatment, survival with advanced pulmonary disease in cystic fibrosis presents new questions and potential problems, which are still being formulated.

Abstract
Rev Bras Ter Intensiva. 2018;30(1):112-115
DOI 10.5935/0103-507X.20180017
Among the main causes of death in our country are car accidents, drowning and accidental burns. Strangulation is a potentially fatal injury and an important cause of homicide and suicide among adults and adolescents. In children, its occurrence is usually accidental. However, in recent years, several cases of accidental strangulation in children around the world have been reported. A 2-year-old male patient was strangled in a car window. The patient was admitted to the pediatric intensive care unit with a Glasgow Coma Scale score of 8 and presented with progressive worsening of respiratory dysfunction and torpor. The patient also presented acute respiratory distress syndrome, acute pulmonary edema and shock. He was managed with protective mechanical ventilation, vasoactive drugs and antibiotic therapy. He was discharged from the intensive care unit without neurological or pulmonary sequelae. After 12 days of hospitalization, he was discharged from the hospital, and his state was very good. The incidence of automobile window strangulation is rare but of high morbidity and mortality due to the resulting choking mechanism. Fortunately, newer cars have devices that stop the automatic closing of the windows if resistance is encountered. However, considering the severity of complications strangulated patients experience, the intensive neuro-ventilatory and hemodynamic management of the pathologies involved is important to reduce morbidity and mortality, as is the need to implement new campaigns for the education of parents and caregivers of children, aiming to avoid easily preventable accidents and to optimize safety mechanisms in cars with electric windows.

Abstract
Rev Bras Ter Intensiva. 2018;30(2):237-243
DOI 10.5935/0103-507X.20180035
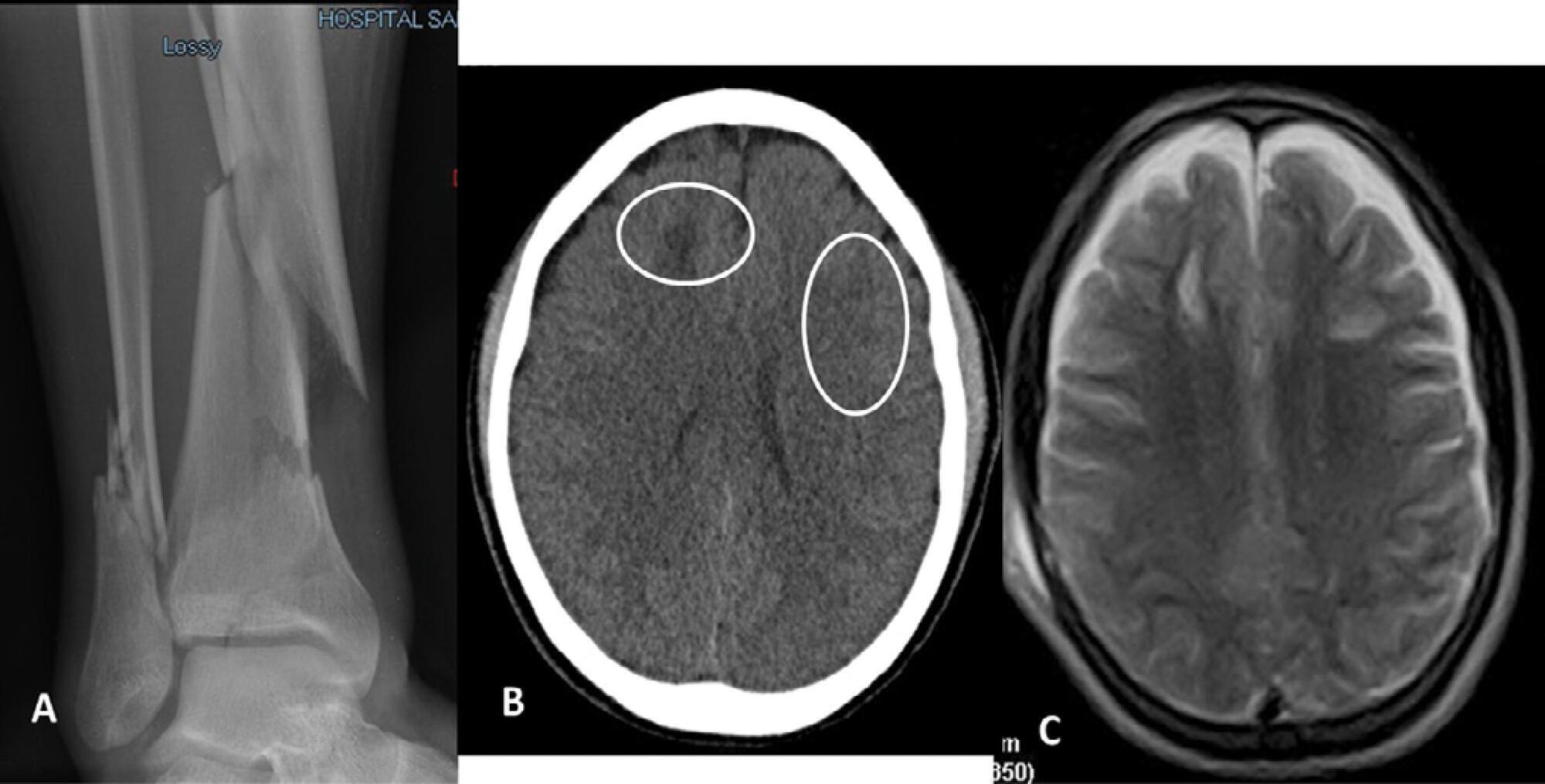
Paroxysmal sympathetic hyperactivity represents an uncommon and potentially life-threatening complication of severe brain injuries, which are most commonly traumatic. This syndrome is a clinical diagnosis based on the recurrent occurrence of tachycardia, hypertension, diaphoresis, tachypnea, and occasionally high fever and dystonic postures. The episodes may be induced by stimulation or may occur spontaneously. Underdiagnosis is common, and delayed recognition may increase morbidity and long-term disability. Trigger avoidance and pharmacological therapy can be very successful in controlling this complication. Fat embolism syndrome is a rare but serious complication of long bone fractures. Neurologic signs, petechial hemorrhages and acute respiratory failure constitute the characteristic presenting triad. The term cerebral fat embolism is used when the neurological involvement predominates. The diagnosis is clinical, but specific neuroimaging findings can be supportive. The neurologic manifestations include different degrees of alteration of consciousness, focal deficits or seizures. Management is supportive, but good outcomes are possible even in cases with very severe presentation. We report two cases of paroxysmal sympathetic hyperactivity after cerebral fat embolism, which is a very uncommon association.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):233-236
DOI 10.5935/0103-507X.20180029
We report the case of a female patient, 58 years of age, without known heart disease, who underwent liver transplantation without complications. On the second postoperative day, the patient developed cardiogenic shock secondary to stress-induced cardiomyopathy (Takotsubo-like syndrome). The patient was successfully managed with veno-arterial peripheral extracorporeal membrane oxygenation for 6 days, with complete recovery of cardiac function and of the hepatic graft. Coronary syndrome and acute myocarditis were excluded as the causes of the shock. The use of extracorporeal membrane oxygenation in this scenario is possible and safe, considering its specialized protocols and treatment.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):105-110
DOI 10.5935/0103-507X.20170015
Acute respiratory distress syndrome is characterized by diffuse inflammatory lung injury and is classified as mild, moderate, and severe. Clinically, hypoxemia, bilateral opacities in lung images, and decreased pulmonary compliance are observed. Sepsis is one of the most prevalent causes of this condition (30 - 50%). Among the direct causes of acute respiratory distress syndrome, chlorine inhalation is an uncommon cause, generating mucosal and airway irritation in most cases. We present a case of severe acute respiratory distress syndrome after accidental inhalation of chlorine in a swimming pool, with noninvasive ventilation used as a treatment with good response in this case. We classified severe acute respiratory distress syndrome based on an oxygen partial pressure/oxygen inspired fraction ratio <100, although the Berlin classification is limited in considering patients with severe hypoxemia managed exclusively with noninvasive ventilation. The failure rate of noninvasive ventilation in cases of acute respiratory distress syndrome is approximately 52% and is associated with higher mortality. The possible complications of using noninvasive positive-pressure mechanical ventilation in cases of acute respiratory distress syndrome include delays in orotracheal intubation, which is performed in cases of poor clinical condition and with high support pressure levels, and deep inspiratory efforts, generating high tidal volumes and excessive transpulmonary pressures, which contribute to ventilation-related lung injury. Despite these complications, some studies have shown a decrease in the rates of orotracheal intubation in patients with acute respiratory distress syndrome with low severity scores, hemodynamic stability, and the absence of other organ dysfunctions.

Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)