You searched for:"Jefferson Pedro Piva"
We found (17) results for your search.-
Letter to the Editor
Death by community-based methicillin-resistant Staphylococcus aureus: case report
Crit Care Sci. 2023;35(4):416-420
Abstract
Letter to the EditorDeath by community-based methicillin-resistant Staphylococcus aureus: case report
Crit Care Sci. 2023;35(4):416-420
DOI 10.5935/2965-2774.20230078-pt
Views19INTRODUCTIONCommunity methicillin-resistant Staphylococcus aureus (CA-MRSA) has by definition a minimum inhibitory concentration for oxacillin ≥ 4mcg/mL, giving it intrinsic resistance to all beta-lactams, including cephalosporins, which is associated with the presence of the mecA gene. It also has bacteriological and epidemiological characteristics distinct from hospital-acquired MRSA, including its resistance profile to other antimicrobials, its genotypic […]See more
-
Original Article
Characteristics and outcome of burned children admitted to a pediatric intensive care unit
Rev Bras Ter Intensiva. 2018;30(3):333-337
Abstract
Original ArticleCharacteristics and outcome of burned children admitted to a pediatric intensive care unit
Rev Bras Ter Intensiva. 2018;30(3):333-337
DOI 10.5935/0103-507X.20180045
Views2See moreABSTRACT
Objective:
To analyze the characteristics and outcomes of children hospitalized for burns in a pediatric trauma intensive care unit for burn patients.
Methods:
An observational study was conducted through the retrospective analysis of children (< 16 years) admitted to the pediatric trauma intensive care unit for burn victims between January 2013 and December 2015. Sociodemographic and clinical variables were analyzed including the causal agent, burned body surface, presence of inhalation injury, length of hospital stay and mortality.
Results:
The study analyzed a sum of 140 patients; 61.8% were male, with a median age of 24 months and an overall mortality of 5%. The main cause of burns was scalding (51.4%), followed by accidents involving fire (38.6%) and electric shock (6.4%). Mechanical ventilation was used in 20.7% of the cases. Associated inhalation injury presented a relative risk of 6.1 (3.5 – 10.7) of needing ventilatory support and a relative risk of mortality of 14.1 (2.9 – 68.3) compared to patients without this associated injury. A significant connection was found between burned body surface and mortality (p < 0.002), reaching 80% in patients with a burned area greater than 50%. Patients who died had a significantly higher Tobiasen Abbreviated Burn Severity Index than survivors (9.6 ± 2.2 versus 4.4 ± 1.1; p < 0.001). A Tobiasen Abbreviated Burn Severity Index ≥ 7 represented a relative risk of death of 68.4 (95%CI 9.1 - 513.5).
Conclusion:
Scalding burns are quite frequent and are associated with high morbidity. Mortality is associated with the amount of burned body surface and the presence of inhalation injury. Special emphasis should be given to accidents involving fire, reinforcing proper diagnosis and treatment of inhalation injury.
-
Commentaries
From the International Pediatric Sepsis Conference 2005 to the Sepsis-3 Consensus
Rev Bras Ter Intensiva. 2018;30(1):1-5
Abstract
CommentariesFrom the International Pediatric Sepsis Conference 2005 to the Sepsis-3 Consensus
Rev Bras Ter Intensiva. 2018;30(1):1-5
DOI 10.5935/0103-507X.20180005
Views1INTRODUCTIONIn the last decades, sepsis, due to an immune response, has been defined as a potentially fatal organ dysfunction resulting from a dysregulated organism response to an infectious insult, in which pro- and anti-inflammatory responses can coexist in the early phase of the disease and which, together with non-immunological mechanisms, decisively influence prognosis and evolution.(–) […]See more -
Original Articles
Translation and cross-cultural adaptation of the Pediatric Confusion Assessment Method for the Intensive Care Unit into Brazilian Portuguese for the detection of delirium in pediatric intensive care units
Rev Bras Ter Intensiva. 2018;30(1):71-79
Abstract
Original ArticlesTranslation and cross-cultural adaptation of the Pediatric Confusion Assessment Method for the Intensive Care Unit into Brazilian Portuguese for the detection of delirium in pediatric intensive care units
Rev Bras Ter Intensiva. 2018;30(1):71-79
DOI 10.5935/0103-507X.20180013
Views0ABSTRACT
Objective:
To undertake the translation and cross-cultural adaption into Brazilian Portuguese of the Pediatric Confusion Assessment Method for the Intensive Care Unit for the detection of delirium in pediatric intensive care units, including the algorithm and instructions.
Methods:
A universalist approach for the translation and cross-cultural adaptation of health measurement instruments was used. A group of pediatric critical care specialists assessed conceptual and item equivalences. Semantic equivalence was evaluated by means of a translation from English to Portuguese by two independent translators; reconciliation into a single version; back-translation by a native English speaker; and consensus among six experts with respect to language and content understanding by means of Likert scale responses and the Content Validity Index. Finally, operational equivalence was assessed by applying a pre-test to 30 patients.
Results:
The back-translation was approved by the original authors. The medians of the expert consensus responses varied between good and excellent, except for the feature “acute onset” of the instructions. Items with a low Content Validity Index for the features “acute onset” and “disorganized thinking” were adapted. In the pre-test, the expression “signal with your head” was modified into “nod your head” for better understanding. No further adjustments were necessary, resulting in the final version for Brazilian Portuguese.
Conclusion:
The Brazilian version of the Pediatric Confusion Assessment Method for the Intensive Care Unit was generated in agreement with the international recommendations and can be used in Brazil for the diagnosis of delirium in critically ill children 5 years of age or above and with no developmental cognitive disabilities.
Keywords:Confusion/diagnosisDelirium/diagnosisIntensive care units, pediatricpCAM-ICUSurveys and Questionnaires/standardsTranslationSee more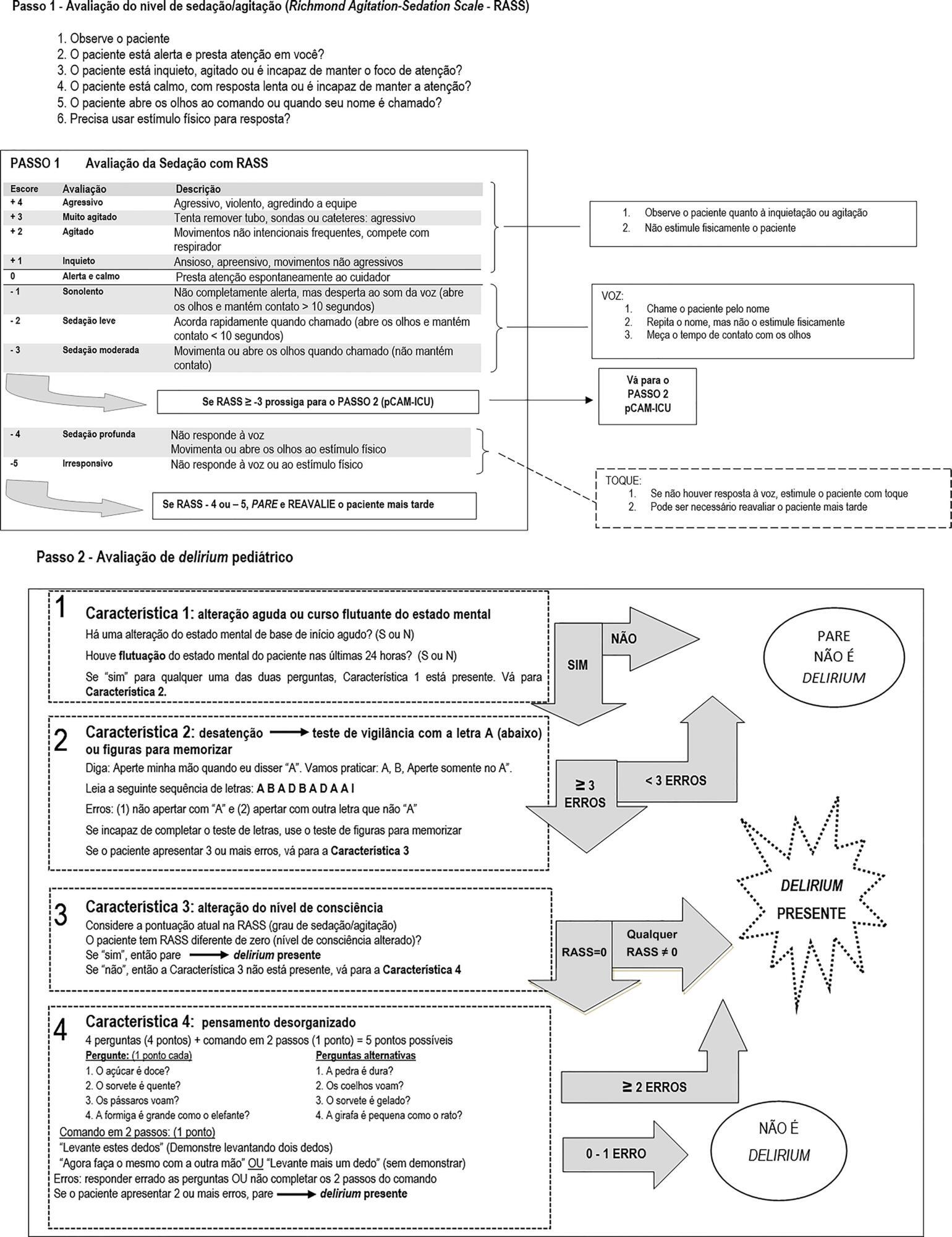
-
Case Reports
Accidental strangulation in children by the automatic closing of a car window
Rev Bras Ter Intensiva. 2018;30(1):112-115
Abstract
Case ReportsAccidental strangulation in children by the automatic closing of a car window
Rev Bras Ter Intensiva. 2018;30(1):112-115
DOI 10.5935/0103-507X.20180017
Views1See moreABSTRACT
Among the main causes of death in our country are car accidents, drowning and accidental burns. Strangulation is a potentially fatal injury and an important cause of homicide and suicide among adults and adolescents. In children, its occurrence is usually accidental. However, in recent years, several cases of accidental strangulation in children around the world have been reported. A 2-year-old male patient was strangled in a car window. The patient was admitted to the pediatric intensive care unit with a Glasgow Coma Scale score of 8 and presented with progressive worsening of respiratory dysfunction and torpor. The patient also presented acute respiratory distress syndrome, acute pulmonary edema and shock. He was managed with protective mechanical ventilation, vasoactive drugs and antibiotic therapy. He was discharged from the intensive care unit without neurological or pulmonary sequelae. After 12 days of hospitalization, he was discharged from the hospital, and his state was very good. The incidence of automobile window strangulation is rare but of high morbidity and mortality due to the resulting choking mechanism. Fortunately, newer cars have devices that stop the automatic closing of the windows if resistance is encountered. However, considering the severity of complications strangulated patients experience, the intensive neuro-ventilatory and hemodynamic management of the pathologies involved is important to reduce morbidity and mortality, as is the need to implement new campaigns for the education of parents and caregivers of children, aiming to avoid easily preventable accidents and to optimize safety mechanisms in cars with electric windows.

-
Commentaries
Neurally adjusted ventilatory assist in pediatrics: why, when, and how?
Rev Bras Ter Intensiva. 2017;29(4):408-413
Abstract
CommentariesNeurally adjusted ventilatory assist in pediatrics: why, when, and how?
Rev Bras Ter Intensiva. 2017;29(4):408-413
DOI 10.5935/0103-507X.20170064
Views0IntroductionIn pediatrics, good synchrony in controlled assisted ventilation is not always possible and may delay recovery, prolong mechanical ventilation (MV), and contribute to loss of muscle strength and increased calorie expenditure.()In controlled assisted ventilation, the trigger (drive) is a decisive factor in the release of the assisted cycle, as it is regulated by the pressure […]See more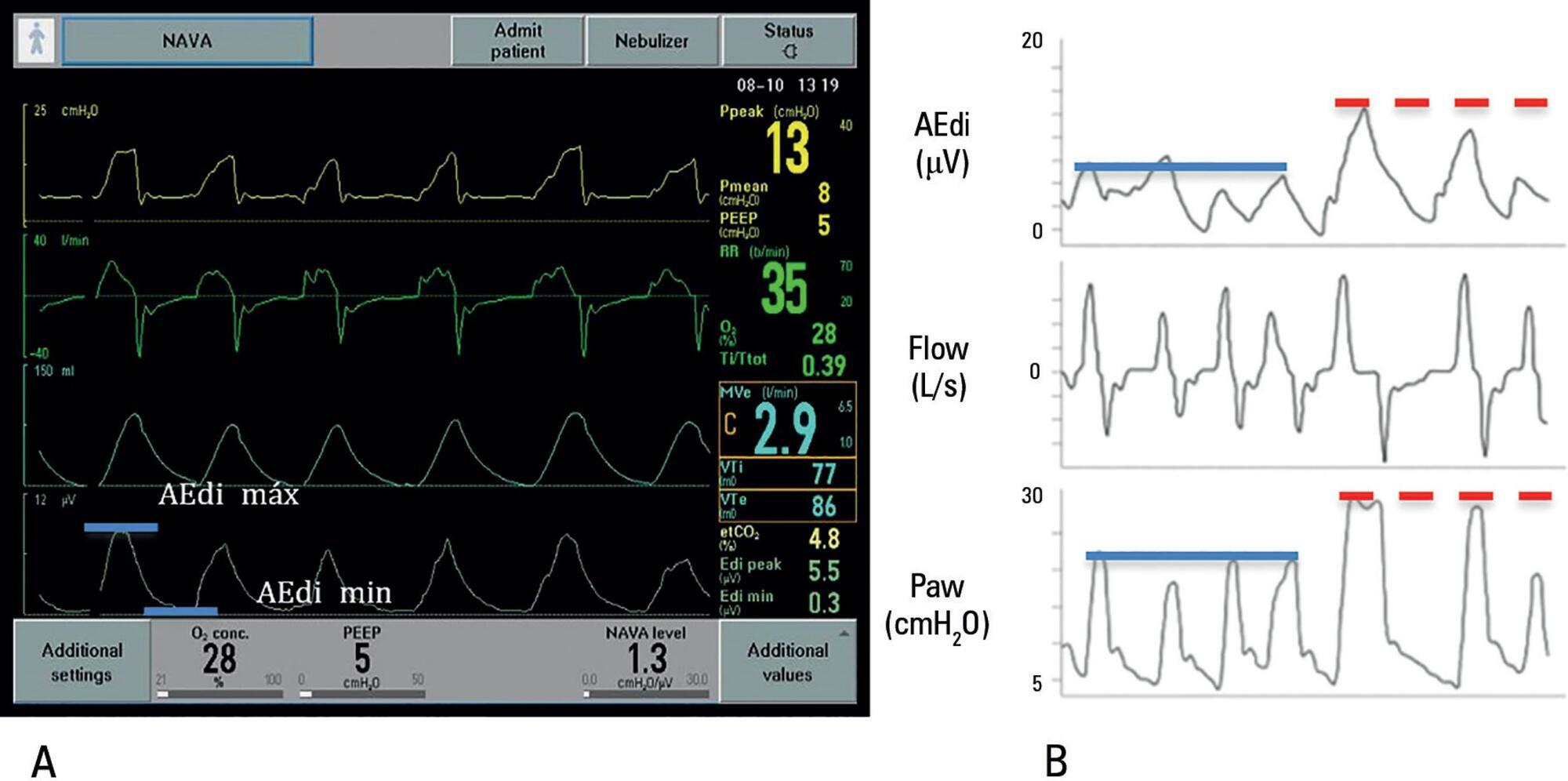
-
Review Articles
Fluid overload in children undergoing mechanical ventilation
Rev Bras Ter Intensiva. 2017;29(3):346-353
Abstract
Review ArticlesFluid overload in children undergoing mechanical ventilation
Rev Bras Ter Intensiva. 2017;29(3):346-353
DOI 10.5935/0103-507X.20170045
Views0ABSTRACT
Patients admitted to an intensive care unit are prone to cumulated fluid overload and receive intravenous volumes through the aggressive resuscitation recommended for septic shock treatment, as well as other fluid sources related to medications and nutritional support. The liberal liquid supply strategy has been associated with higher morbidity and mortality. Although there are few prospective pediatric studies, new strategies are being proposed. This non-systematic review discusses the pathophysiology of fluid overload, its consequences, and the available therapeutic strategies. During systemic inflammatory response syndrome, the endothelial glycocalyx is damaged, favoring fluid extravasation and resulting in interstitial edema. Extravasation to the third space results in longer mechanical ventilation, a greater need for renal replacement therapy, and longer intensive care unit and hospital stays, among other changes. Proper hemodynamic monitoring, as well as cautious infusion of fluids, can minimize these damages. Once cumulative fluid overload is established, treatment with long-term use of loop diuretics may lead to resistance to these medications. Strategies that can reduce intensive care unit morbidity and mortality include the early use of vasopressors (norepinephrine) to improve cardiac output and renal perfusion, the use of a combination of diuretics and aminophylline to induce diuresis, and the use of sedation and early mobilization protocols.
Keywords:Fluid therapyHemodynamicsRenal insufficiencyRespiration, artificialWater-electrolyte imbalanceSee more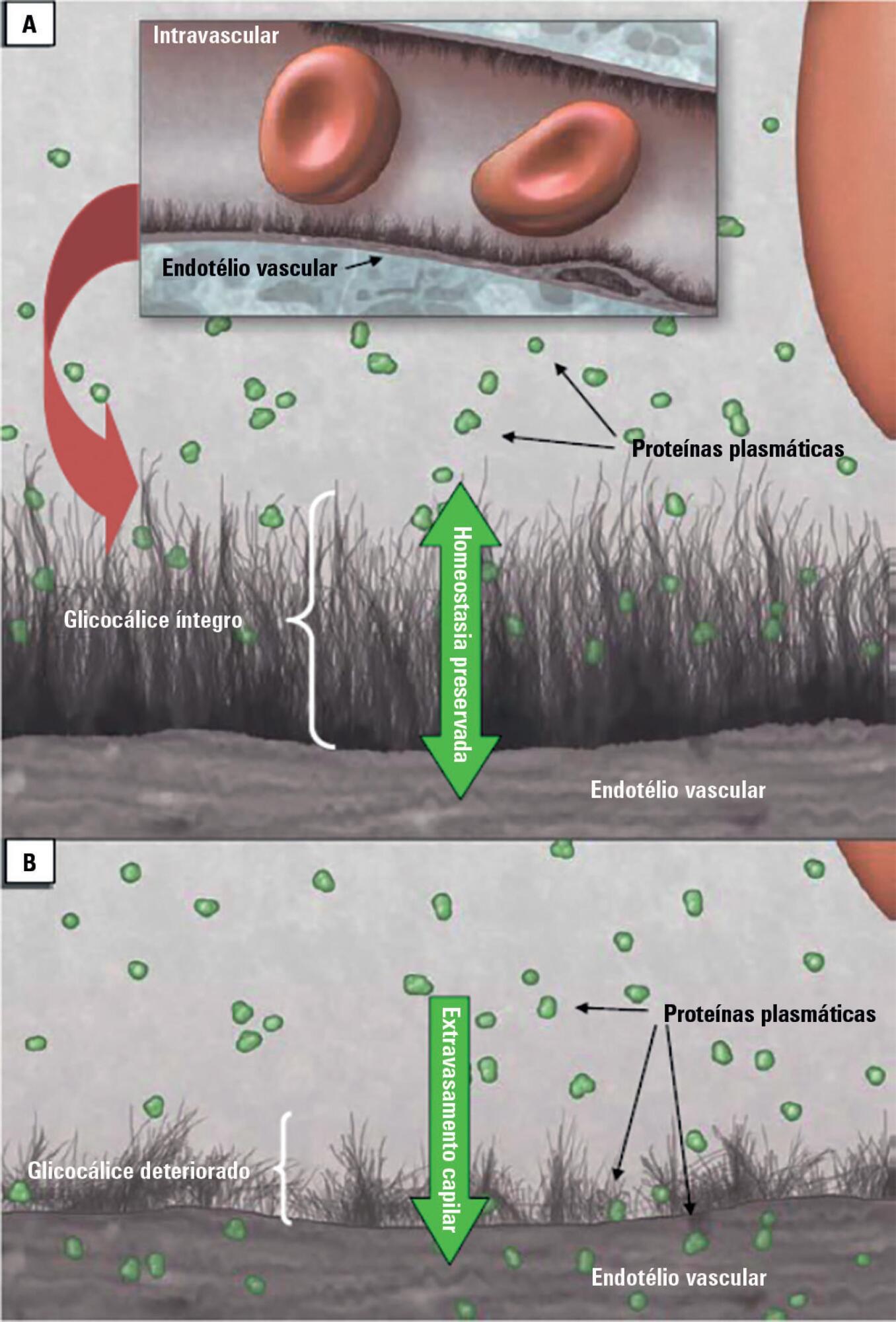
-
Original Articles
Characteristics and progression of children with acute viral bronchiolitis subjected to mechanical ventilation
Rev Bras Ter Intensiva. 2016;28(1):55-61
Abstract
Original ArticlesCharacteristics and progression of children with acute viral bronchiolitis subjected to mechanical ventilation
Rev Bras Ter Intensiva. 2016;28(1):55-61
DOI 10.5935/0103-507X.20160003
Views0ABSTRACT
Objective:
To analyze the characteristics of children with acute viral bronchiolitis subjected to mechanical ventilation for three consecutive years and to correlate their progression with mechanical ventilation parameters and fluid balance.
Methods:
Longitudinal study of a series of infants (< one year old) subjected to mechanical ventilation for acute viral bronchitis from January 2012 to September 2014 in the pediatric intensive care unit. The children's clinical records were reviewed, and their anthropometric data, mechanical ventilation parameters, fluid balance, clinical progression, and major complications were recorded.
Results:
Sixty-six infants (3.0 ± 2.0 months old and with an average weight of 4.7 ± 1.4kg) were included, of whom 62% were boys; a virus was identified in 86%. The average duration of mechanical ventilation was 6.5 ± 2.9 days, and the average length of stay in the pediatric intensive care unit was 9.1 ± 3.5 days; the mortality rate was 1.5% (1/66). The peak inspiratory pressure remained at 30cmH2O during the first four days of mechanical ventilation and then decreased before extubation (25 cmH2O; p < 0.05). Pneumothorax occurred in 10% of the sample and extubation failure in 9%, which was due to upper airway obstruction in half of the cases. The cumulative fluid balance on mechanical ventilation day four was 402 ± 254mL, which corresponds to an increase of 9.0 ± 5.9% in body weight. Thirty-seven patients (56%) exhibited a weight gain of 10% or more, which was not significantly associated with the ventilation parameters on mechanical ventilation day four, extubation failure, duration of mechanical ventilation or length of stay in the pediatric intensive care unit.
Conclusion:
The rate of mechanical ventilation for acute viral bronchiolitis remains constant, being associated with low mortality, few adverse effects, and positive cumulative fluid balance during the first days. Better fluid control might reduce the duration of mechanical ventilation.
Keywords:BronchiolitisChildEdemaIntensive care unitsRespiration, artificialRespiratory syncytial virusesSee more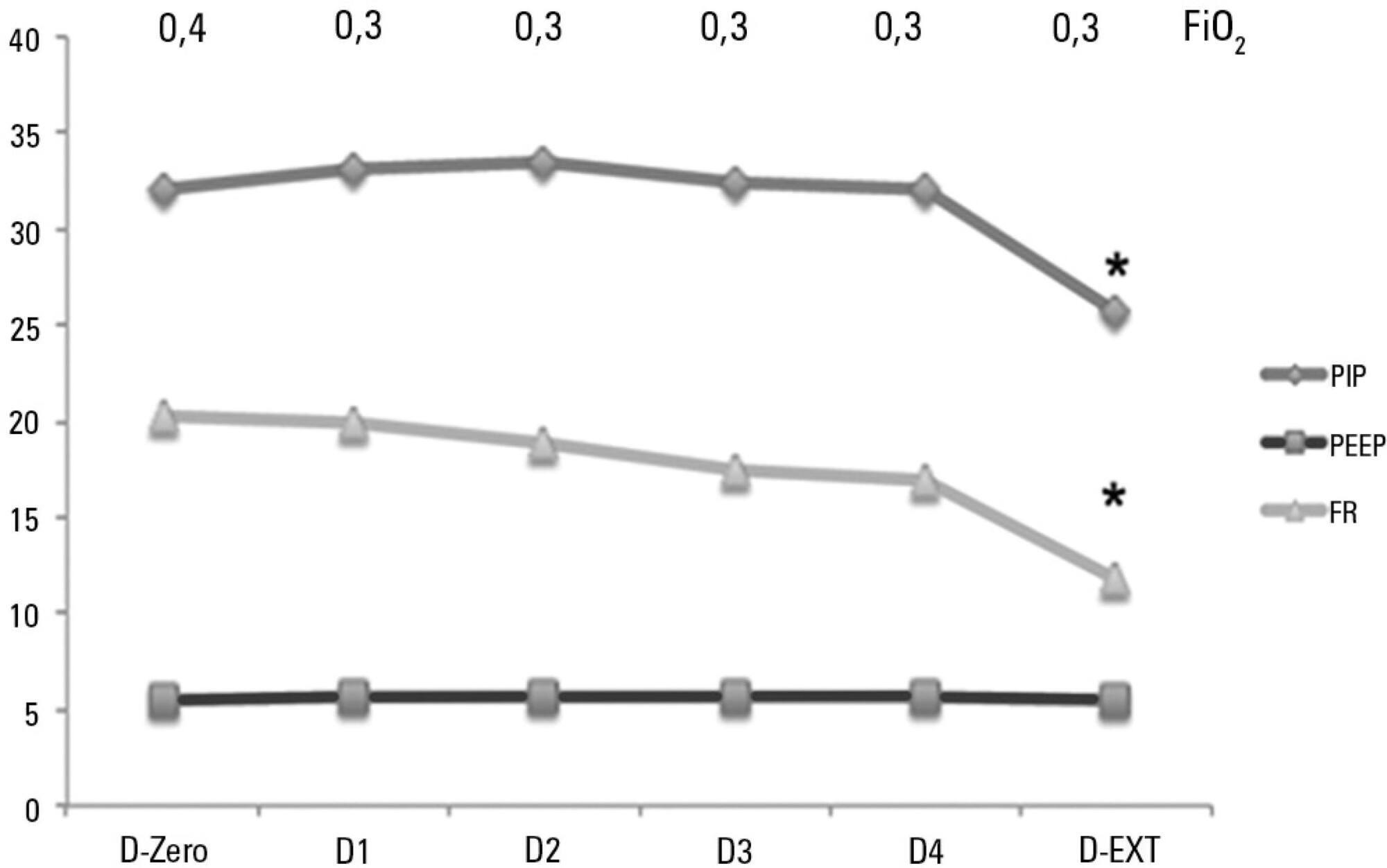
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




