Abstract
Rev Bras Ter Intensiva. 2021;33(2):206-218
DOI 10.5935/0103-507X.20210028
To describe fluid resuscitation practices in Brazilian intensive care units and to compare them with those of other countries participating in the Fluid-TRIPS.
This was a prospective, international, cross-sectional, observational study in a convenience sample of intensive care units in 27 countries (including Brazil) using the Fluid-TRIPS database compiled in 2014. We described the patterns of fluid resuscitation use in Brazil compared with those in other countries and identified the factors associated with fluid choice.
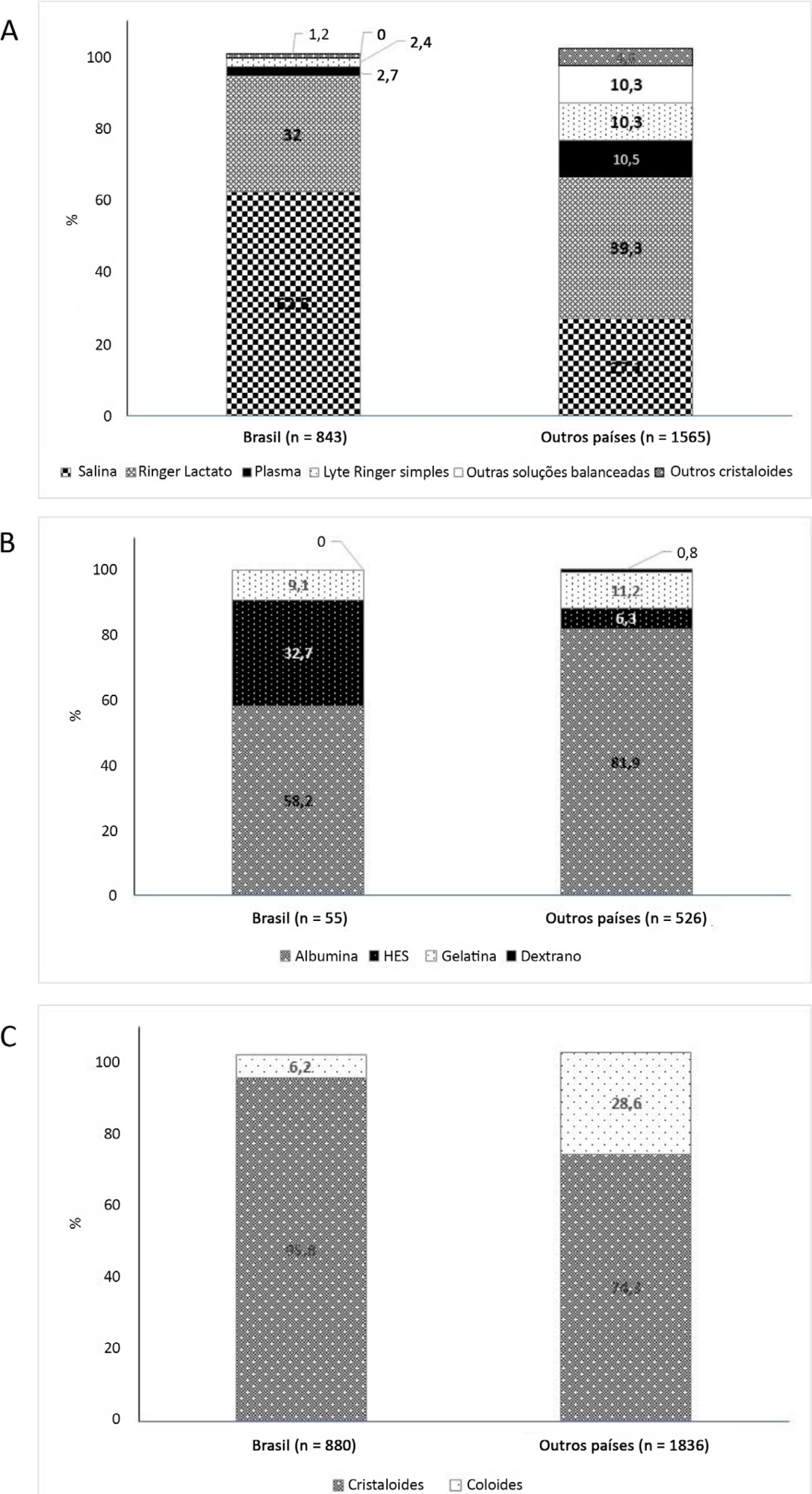
On the study day, 3,214 patients in Brazil and 3,493 patients in other countries were included, of whom 16.1% and 26.8% (p < 0.001) received fluids, respectively. The main indication for fluid resuscitation was impaired perfusion and/or low cardiac output (Brazil: 71.7% versus other countries: 56.4%, p < 0.001). In Brazil, the percentage of patients receiving crystalloid solutions was higher (97.7% versus 76.8%, p < 0.001), and 0.9% sodium chloride was the most commonly used crystalloid (62.5% versus 27.1%, p < 0.001). The multivariable analysis suggested that the albumin levels were associated with the use of both crystalloids and colloids, whereas the type of fluid prescriber was associated with crystalloid use only.
Our results suggest that crystalloids are more frequently used than colloids for fluid resuscitation in Brazil, and this discrepancy in frequencies is higher than that in other countries. Sodium chloride (0.9%) was the crystalloid most commonly prescribed. Serum albumin levels and the type of fluid prescriber were the factors associated with the choice of crystalloids or colloids for fluid resuscitation.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):99-107
DOI 10.5935/0103-507X.20200015
To assess whether fluid overload in fluid therapy is a prognostic factor for patients with septic shock when adjusted for lactate clearance goals.
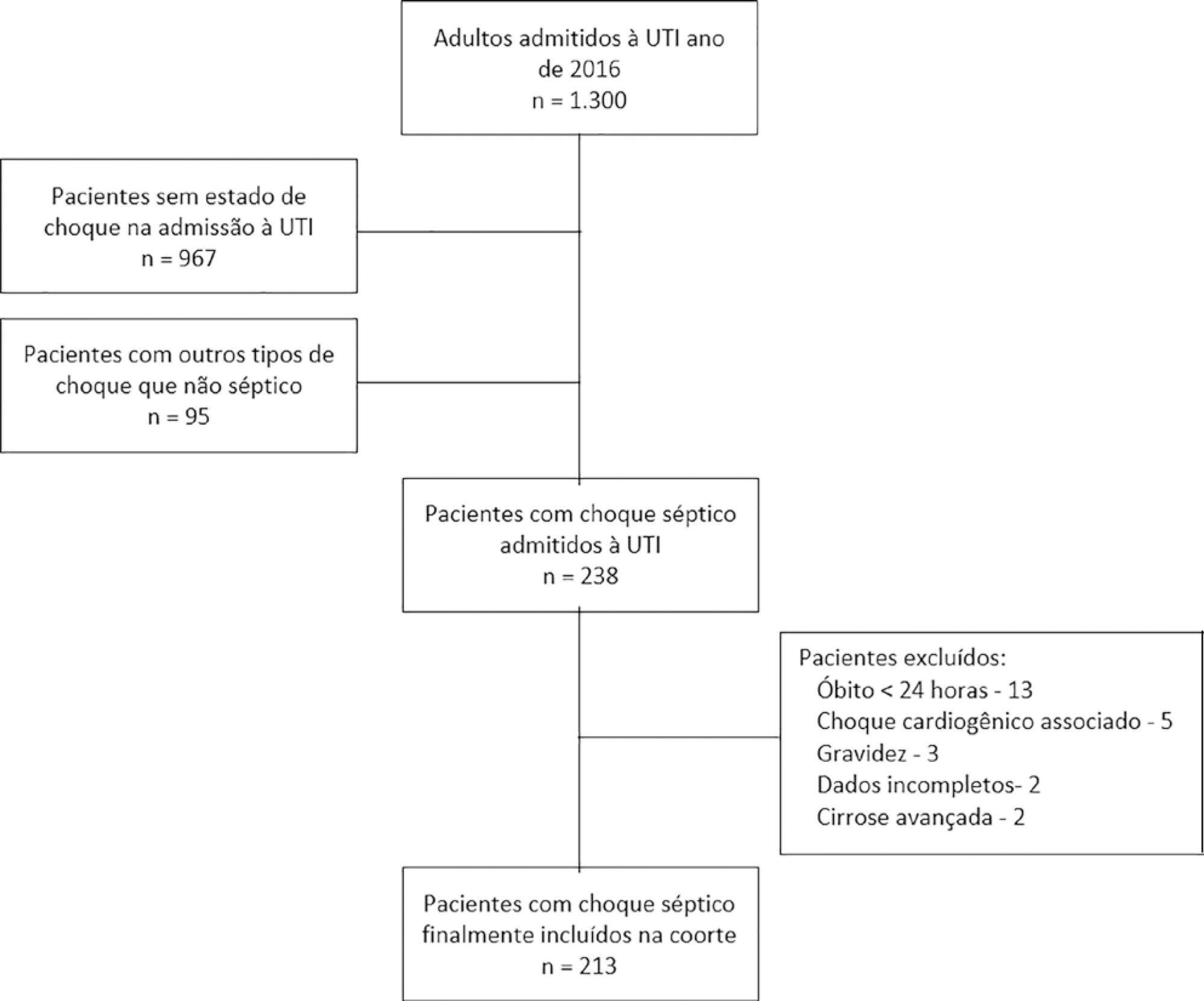
This was a retrospective cohort study conducted at a level IV care hospital in Bogotá, Colombia. A cohort of patients with septic shock was assembled. Their characteristics and fluid balance were documented. The patients were stratified by exposure levels according to the magnitude of fluid overload by body weight after 24 hours of therapy. Mortality was determined at 30 days, and an unconditional logistic regression model was created, adjusting for confounders. The statistical significance was established at p ≤ 0.05.
There were 213 patients with septic shock, and 60.8% had a lactate clearance ≥ 50% after treatment. Ninety-seven (46%) patients developed fluid overload ≥ 5%, and only 30 (13%) developed overload ≥ 10%. Patients exhibiting fluid overload ≥ 5% received an average of 6227mL of crystalloids (SD ± 5838mL) in 24 hours, compared to 3978mL (SD ± 3728mL) among unexposed patients (p = 0.000). The patients who developed fluid overload were treated with mechanical ventilation (70.7% versus 50.8%) (p = 0.003), albumin (74.7% versus 55.2%) (p = 0.003) and corticosteroids (53.5% versus 35.0%) (p = 0.006) more frequently than those who did not develop fluid overload. In the multivariable analysis, cumulative fluid balance was not associated with mortality (OR 1.03; 95%CI 0.89 - 1.20).
Adjusting for the severity of the condition and adequate lactate clearance, cumulative fluid balance was not associated with increased mortality in this Latin American cohort of septic patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):340-346
DOI 10.5935/0103-507X.20190049
To identify the underlying factors that affect fluid resuscitation in septic patients.
The present study was a case-control study of 181 consecutive patients admitted to a Medical Intensive Care Unit between 2012 and 2016 with a diagnosis of sepsis. Demographic, clinical, radiological and laboratory data were analyzed.
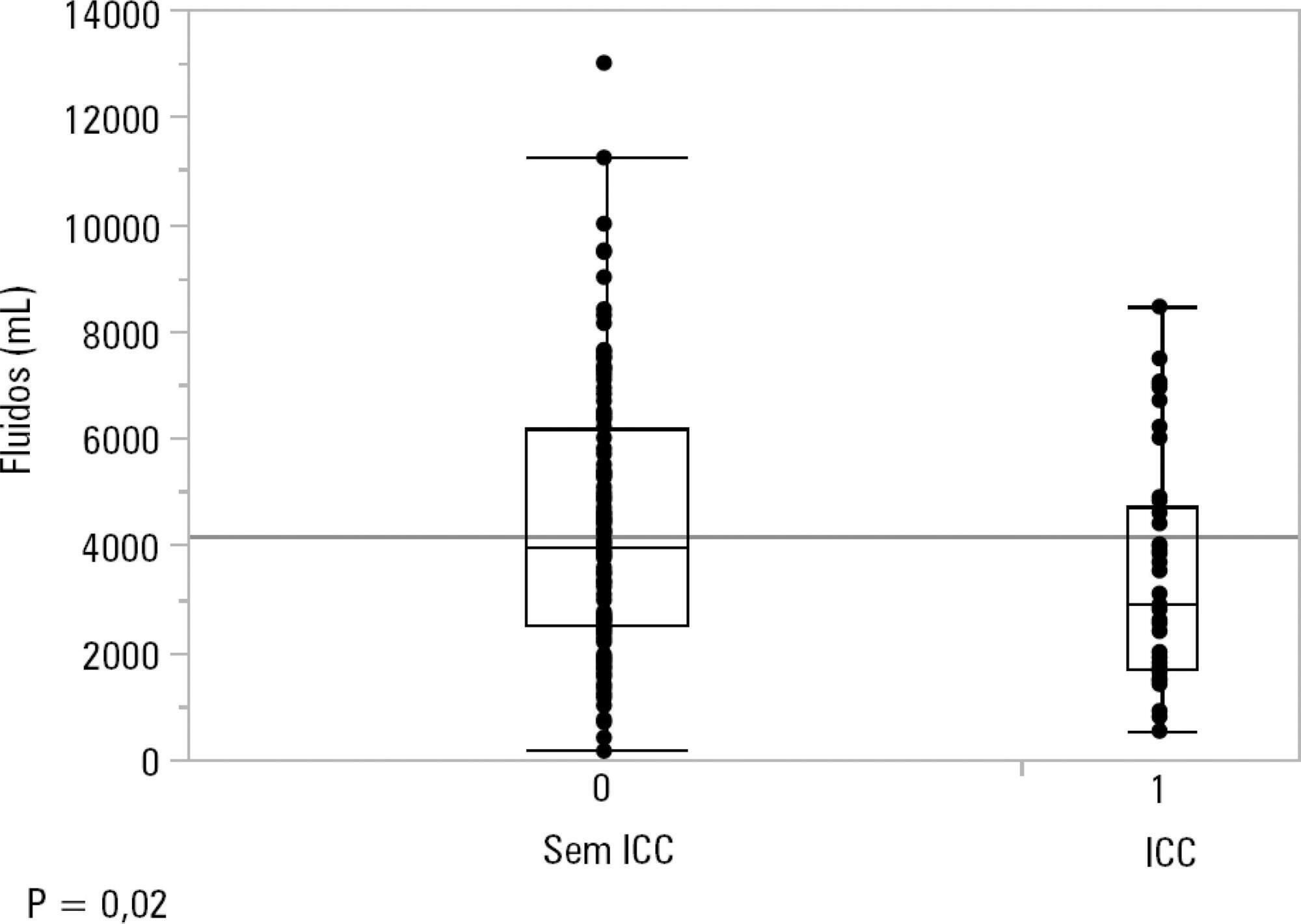
One hundred-thirty patients (72%) received ≥ 30mL/kg of IV fluids on admission. On univariate analyses, a past history of coronary artery disease and heart failure was associated with less fluid therapy. On multivariate analyses, a history of heart failure (OR = 2.31; 95%CI 1.04 - 5.14) remained significantly associated with receiving less IV fluids. Left ventricular ejection fraction, systolic/diastolic function, left ventricular hypertrophy and pulmonary hypertension were not associated with IV fluids. The amount of IV fluids was not associated with differences in mortality. During the first 24 hours, patients with a past history of heart failure received 2,900mLof IV fluids [1,688 - 4,714mL] versus 3,977mL [2,500 - 6,200mL] received by those without a history of heart failure, p = 0.02.
Septic patients with a past history of heart failure received 1L less IV fluids in the first 24 hours with no difference in mortality.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):240-247
DOI 10.5935/0103-507X.20190039
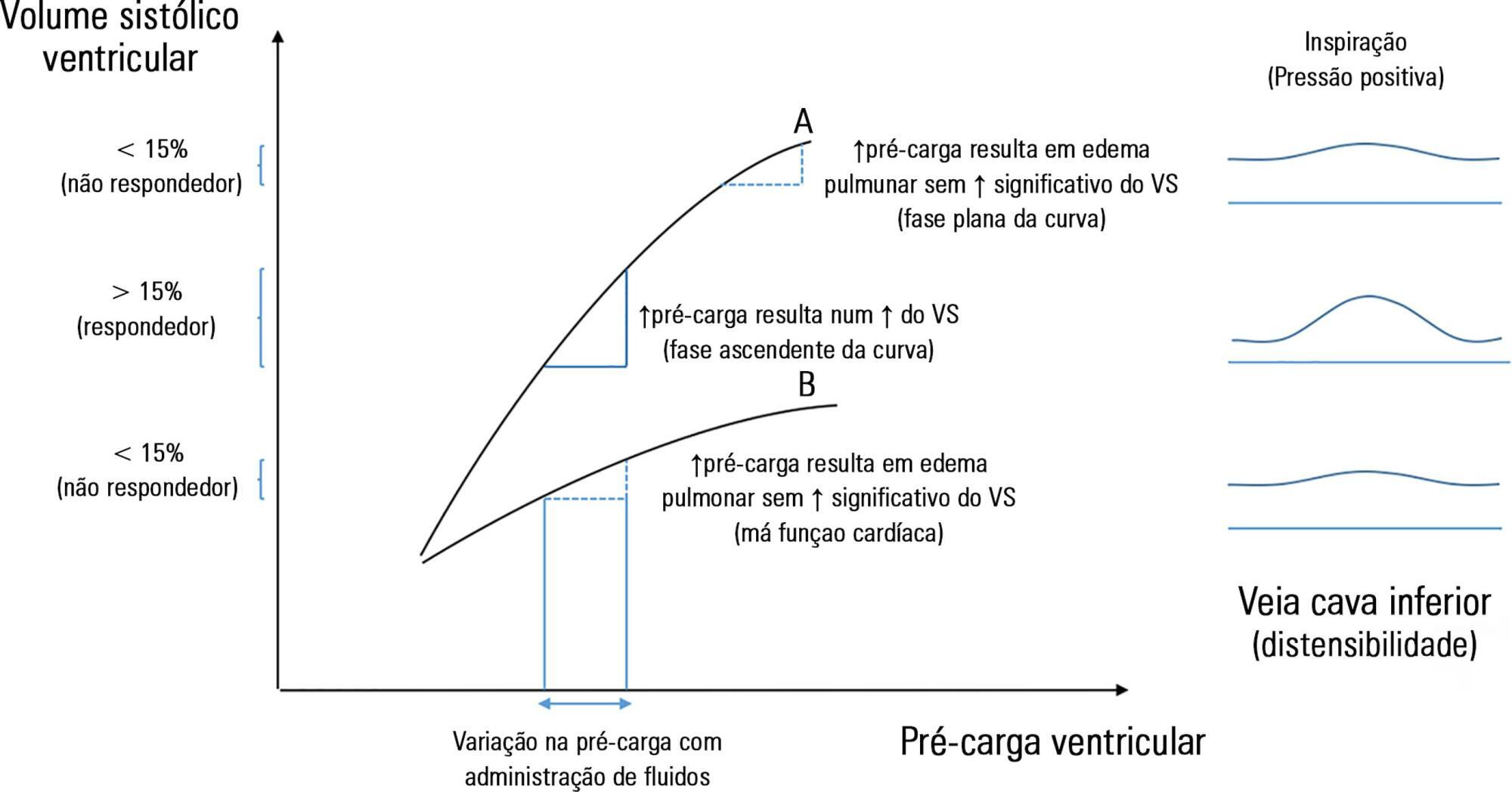
The fluid resuscitation of patients with acute circulatory failure aims to increase systolic volume and consequently improve cardiac output for better tissue oxygenation. However, this effect does not always occur because approximately half of patients do not respond to fluids. The evaluation of fluid responsiveness before their administration may help to identify patients who would benefit from fluid resuscitation and avoid the risk of fluid overload in the others. The dynamic parameters of fluid responsiveness evaluation are promising predictive factors. Of these, the echocardiographic measurement of the respiratory variation in the inferior vena cava diameter is easy to apply and has been used in the hemodynamic evaluation of intensive care unit patients. However, the applicability of this technique has many limitations, and the present studies are heterogeneous and inconsistent across specific groups of patients. We review the use of the inferior vena cava diameter respiratory variation, measured via transthoracic echocardiography, to decide whether to administer fluids to patients with acute circulatory failure in the intensive care unit. We explore the benefits and limitations of this technique, its current use, and the existing evidence.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):346-353
DOI 10.5935/0103-507X.20170045
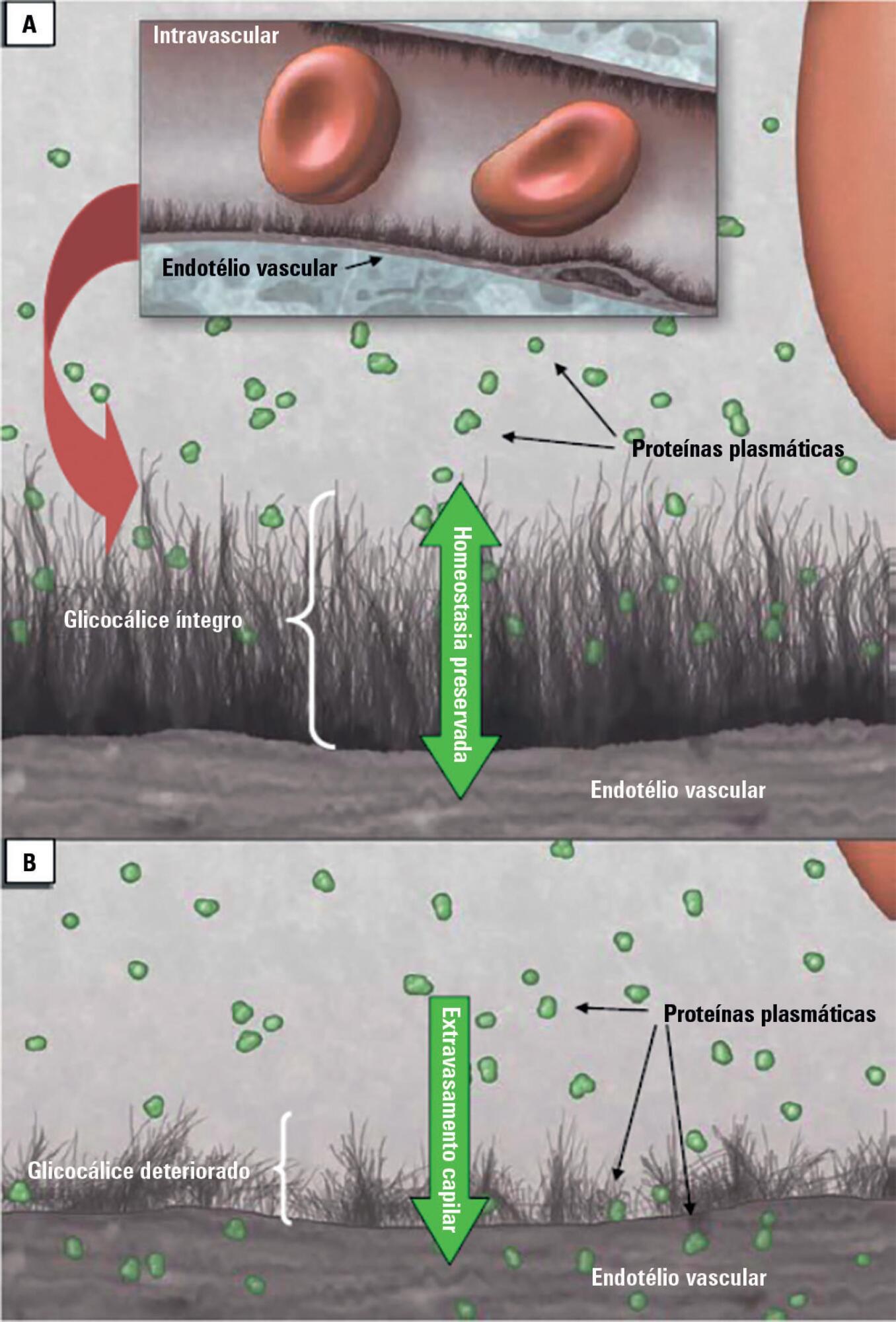
Patients admitted to an intensive care unit are prone to cumulated fluid overload and receive intravenous volumes through the aggressive resuscitation recommended for septic shock treatment, as well as other fluid sources related to medications and nutritional support. The liberal liquid supply strategy has been associated with higher morbidity and mortality. Although there are few prospective pediatric studies, new strategies are being proposed. This non-systematic review discusses the pathophysiology of fluid overload, its consequences, and the available therapeutic strategies. During systemic inflammatory response syndrome, the endothelial glycocalyx is damaged, favoring fluid extravasation and resulting in interstitial edema. Extravasation to the third space results in longer mechanical ventilation, a greater need for renal replacement therapy, and longer intensive care unit and hospital stays, among other changes. Proper hemodynamic monitoring, as well as cautious infusion of fluids, can minimize these damages. Once cumulative fluid overload is established, treatment with long-term use of loop diuretics may lead to resistance to these medications. Strategies that can reduce intensive care unit morbidity and mortality include the early use of vasopressors (norepinephrine) to improve cardiac output and renal perfusion, the use of a combination of diuretics and aminophylline to induce diuresis, and the use of sedation and early mobilization protocols.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):70-76
DOI 10.5935/0103-507X.20170011
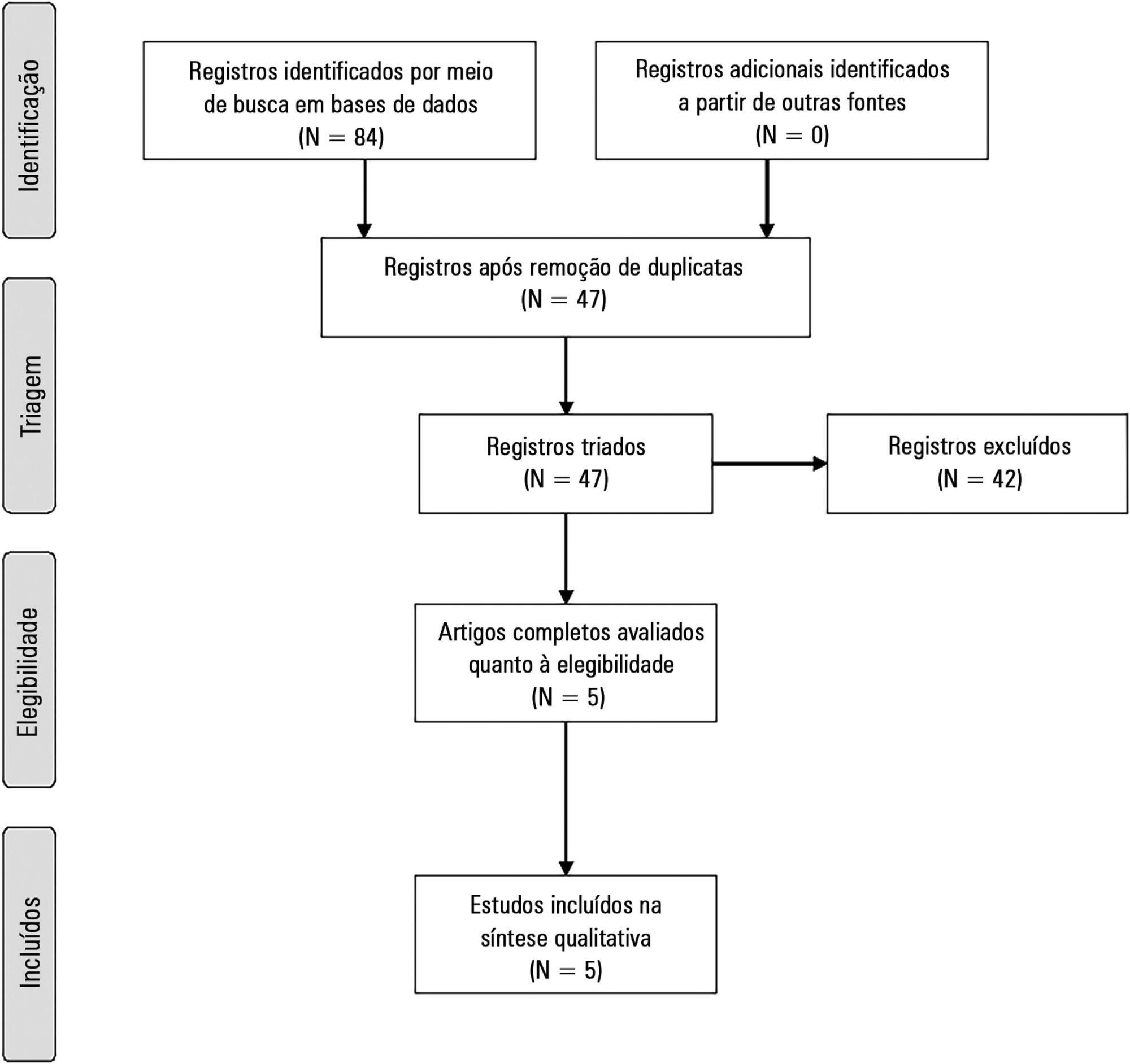
The present systematic review searched for published data on the prevalence of required conditions for proper assessment in critically ill patients.
The Medline, Scopus and Web of Science databases were searched to identify studies that evaluated the prevalence of validated conditions for the fluid responsiveness assessment using respiratory variations in the stroke volume or another surrogate in adult critically ill patients. The primary outcome was the suitability of the fluid responsiveness evaluation. The secondary objectives were the type and prevalence of pre-requisites evaluated to define the suitability.
Five studies were included (14,804 patients). High clinical and statistical heterogeneity was observed (I2 = 98.6%), which prevented us from pooling the results into a meaningful summary conclusion. The most frequent limitation identified is the absence of invasive mechanical ventilation with a tidal volume ≥ 8mL/kg. The final suitability for the fluid responsiveness assessment was low (in four studies, it varied between 1.9 to 8.3%, in one study, it was 42.4%).
Applicability of the dynamic indices of preload responsiveness requiring heart-lung interactions might be limited in daily practice.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):205-211
DOI 10.5935/0103-507X.20150042
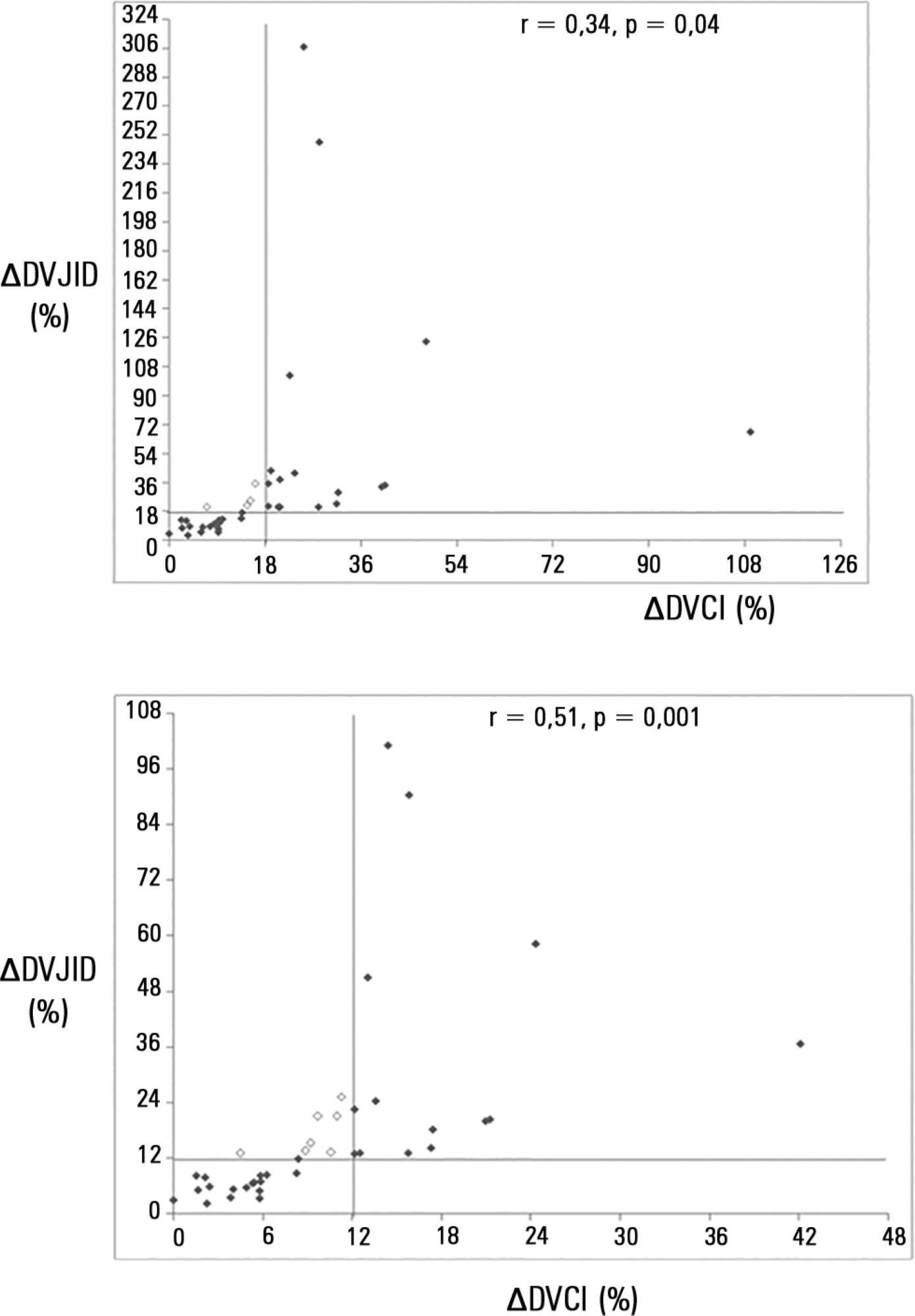
To investigate whether the respiratory variation of the inferior vena cava diameter (∆DIVC) and right internal jugular vein diameter (∆DRIJ) are correlated in mechanically ventilated patients.
This study was a prospective clinical analysis in an intensive care unit at a university hospital. Thirty-nine mechanically ventilated patients with hemodynamic instability were included. ∆DIVC and ∆DRIJ were assessed by echography. Vein distensibility was calculated as the ratio of (A) Dmax - Dmin/Dmin and (B) Dmax - Dmin/ mean of Dmax - Dmin and expressed as a percentage.
∆DIVC and ∆DRIJ were correlated by both methods: (A) r = 0.34, p = 0.04 and (B) r = 0.51, p = 0.001. Using 18% for ∆DIVC, indicating fluid responsiveness by method (A), 16 patients were responders and 35 measurements showed agreement (weighted Kappa = 0.80). The area under the ROC curve was 0.951 (95%CI 0.830 - 0.993; cutoff = 18.92). Using 12% for ∆DIVC, indicating fluid responsiveness by method (B), 14 patients were responders and 32 measurements showed agreement (weighted Kappa = 0.65). The area under the ROC curve was 0.903 (95%CI 0.765 - 0.973; cut-off value = 11.86).
The respiratory variation of the inferior vena cava and the right internal jugular veins are correlated and showed significant agreement. Evaluation of right internal jugular vein distensibility appears to be a surrogate marker for inferior vena cava vein distensibility for evaluating fluid responsiveness.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):10-17
DOI 10.5935/0103-507X.20150004
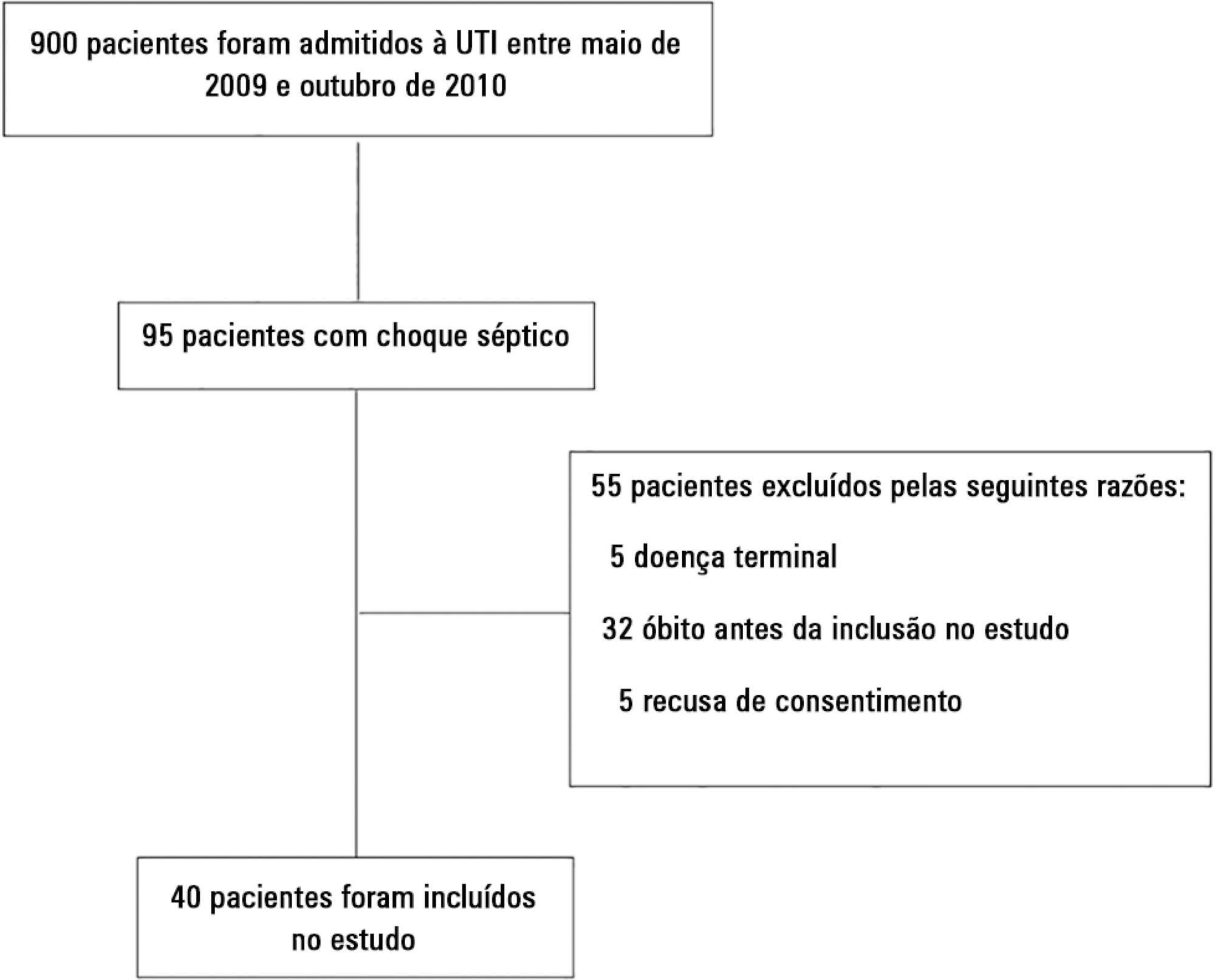
We aimed to evaluate the cumulative fluid balance during the period of shock and determine what happens to fluid balance in the 7 days following recovery from shock.
A prospective and observational study in septic shock patients. Patients with a mean arterial pressure ≥ 65mmHg and lactate < 2.0mEq/L were included < 12 hours after weaning from vasopressor, and this day was considered day 1. The daily fluid balance was registered during and for seven days after recovery from shock. Patients were divided into two groups according to the full cohort’s median cumulative fluid balance during the period of shock: Group 1 ≤ 4.4L (n = 20) and Group 2 > 4.4L (n = 20).
We enrolled 40 patients in the study. On study day 1, the cumulative fluid balance was 1.1 [0.6 - 3.4] L in Group 1 and 9.0 [6.7 - 13.8] L in Group 2. On study day 7, the cumulative fluid balance was 8.0 [4.5 - 12.4] L in Group 1 and 14.7 [12.7 - 20.6] L in Group 2 (p < 0.001 for both). Afterwards, recovery of shock fluid balance continued to increase in both groups. Group 2 had a more prolonged length of stay in the intensive care unit and hospital compared to Group 1.
In conclusion, positive fluid balances are frequently seen in patients with septic shock and may be related to worse outcomes. During the shock period, even though the fluid balance was previously positive, it becomes more positive. After recovery from shock, the fluid balance continues to increase. The group with a more positive fluid balance group spent more time in the intensive care unit and hospital.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)