Abstract
Rev Bras Ter Intensiva. 2017;29(1):70-76
DOI 10.5935/0103-507X.20170011
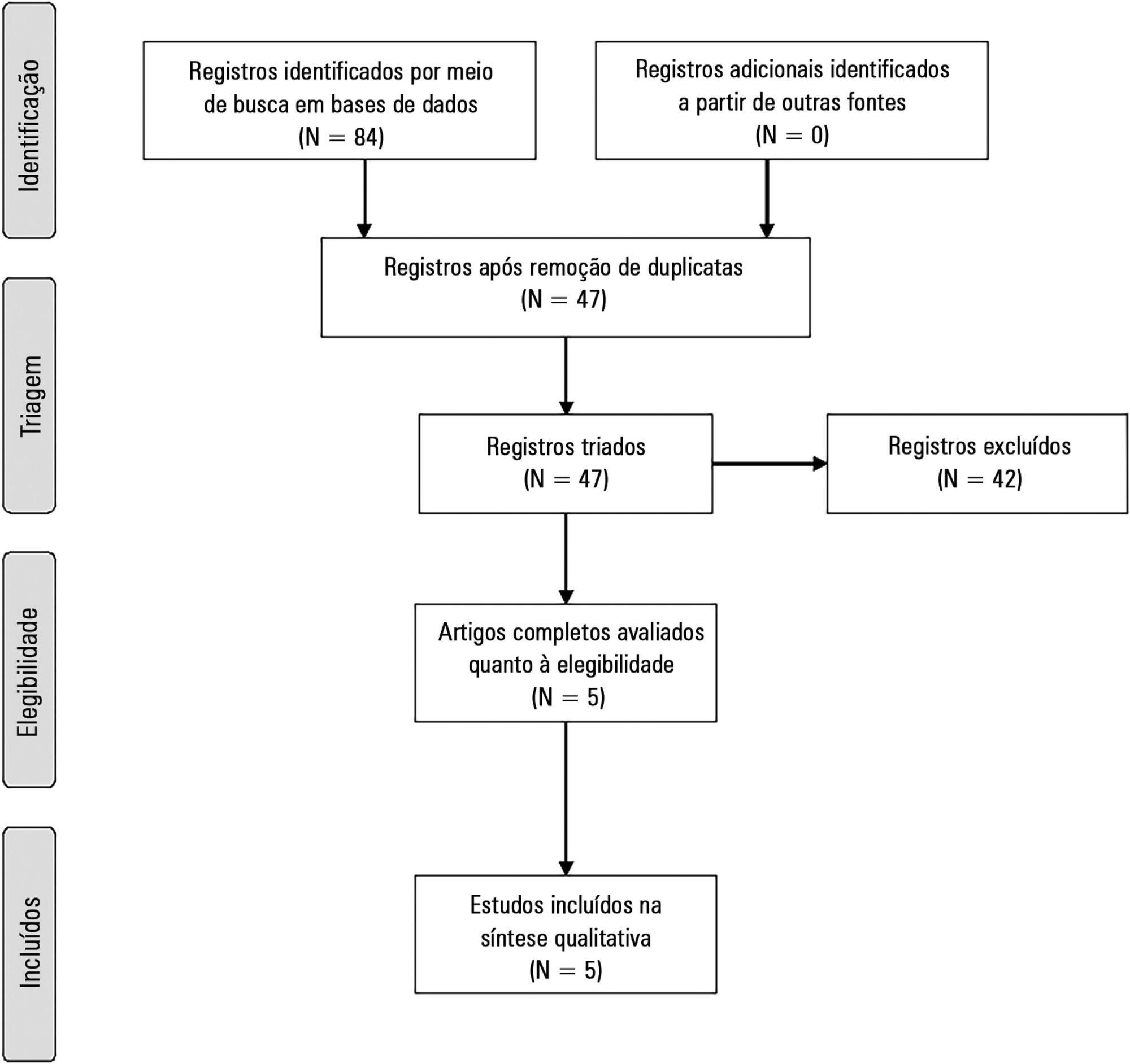
The present systematic review searched for published data on the prevalence of required conditions for proper assessment in critically ill patients.
The Medline, Scopus and Web of Science databases were searched to identify studies that evaluated the prevalence of validated conditions for the fluid responsiveness assessment using respiratory variations in the stroke volume or another surrogate in adult critically ill patients. The primary outcome was the suitability of the fluid responsiveness evaluation. The secondary objectives were the type and prevalence of pre-requisites evaluated to define the suitability.
Five studies were included (14,804 patients). High clinical and statistical heterogeneity was observed (I2 = 98.6%), which prevented us from pooling the results into a meaningful summary conclusion. The most frequent limitation identified is the absence of invasive mechanical ventilation with a tidal volume ≥ 8mL/kg. The final suitability for the fluid responsiveness assessment was low (in four studies, it varied between 1.9 to 8.3%, in one study, it was 42.4%).
Applicability of the dynamic indices of preload responsiveness requiring heart-lung interactions might be limited in daily practice.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):406-411
DOI 10.5935/0103-507X.20150068
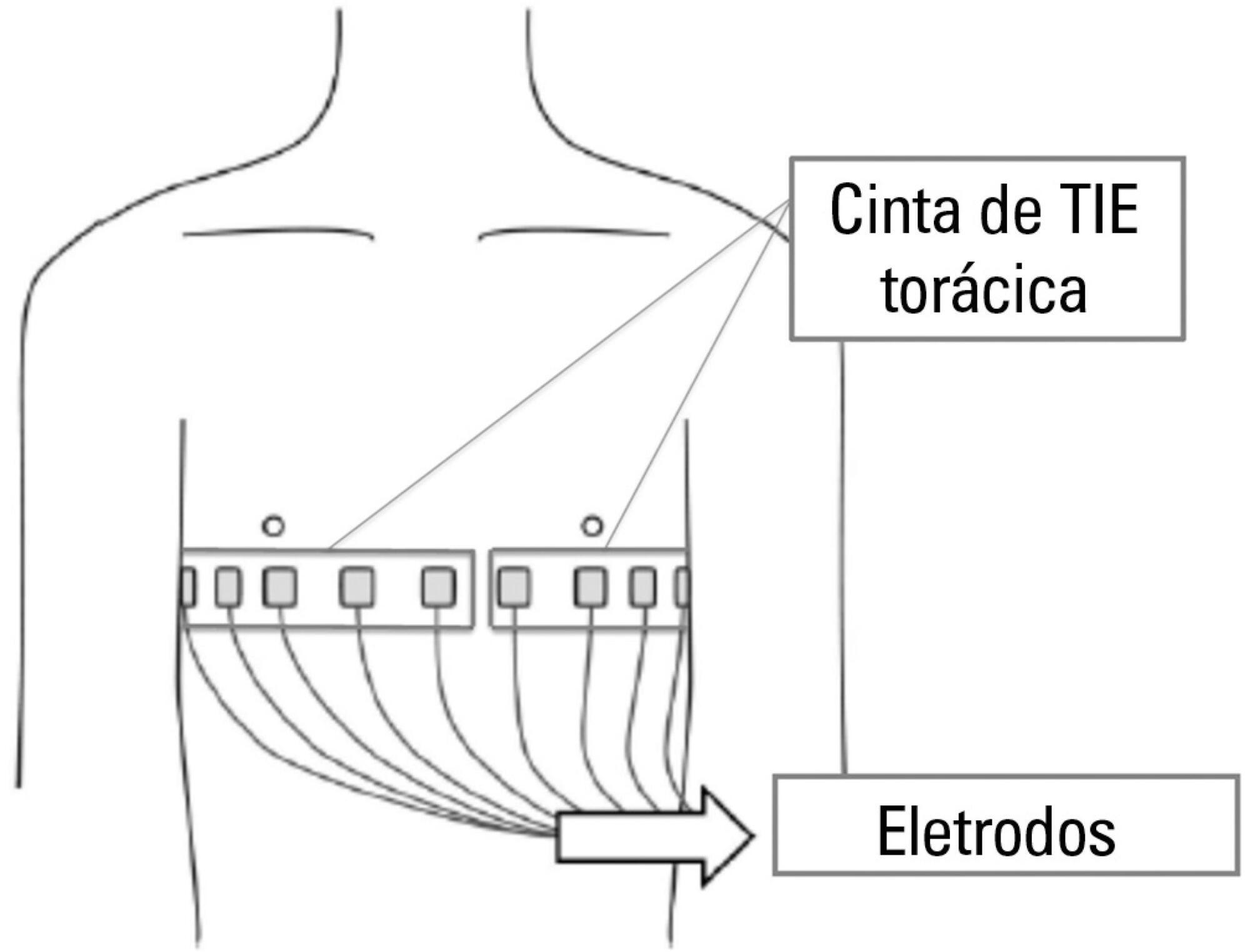
Thoracic electrical impedance tomography is a real-time, noninvasive monitoring tool of the regional pulmonary ventilation distribution. Its bedside use in patients with acute respiratory distress syndrome has the potential to aid in alveolar recruitment maneuvers, which are often necessary in cases of refractory hypoxemia. In this case report, we describe the monitoring results and interpretation of thoracic electrical impedance tomography used during alveolar recruitment maneuvers in a patient with acute respiratory distress syndrome, with transient application of high alveolar pressures and optimal positive end-expiratory pressure titration. Furthermore, we provide a brief literature review regarding the use of alveolar recruitment maneuvers and monitoring using thoracic electrical impedance tomography in patients with acute respiratory distress syndrome.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):360-366
DOI 10.5935/0103-507X.20140055
In Brazil, there are no data on the preferences of intensivists regarding hemodynamic monitoring methods. The present study aimed to identify the methods used by national intensivists, the hemodynamic variables they consider important, the regional differences, the reasons for choosing a particular method, and the use of protocols and continued training.
National intensivists were invited to answer an electronic questionnaire during three intensive care events and later, through the Associação de Medicina Intensiva Brasileira portal, between March and October 2009. Demographic data and aspects related to the respondent preferences regarding hemodynamic monitoring were researched.
In total, 211 professionals answered the questionnaire. Private hospitals showed higher availability of resources for hemodynamic monitoring than did public institutions. The pulmonary artery catheter was considered the most trusted by 56.9% of the respondents, followed by echocardiograms, at 22.3%. Cardiac output was considered the most important variable. Other variables also considered relevant were mixed/central venous oxygen saturation, pulmonary artery occlusion pressure, and right ventricular end-diastolic volume. Echocardiography was the most used method (64.5%), followed by pulmonary artery catheter (49.3%). Only half of respondents used treatment protocols, and 25% worked in continuing education programs in hemodynamic monitoring.
Hemodynamic monitoring has a greater availability in intensive care units of private institutions in Brazil. Echocardiography was the most used monitoring method, but the pulmonary artery catheter remains the most reliable. The implementation of treatment protocols and continuing education programs in hemodynamic monitoring in Brazil is still insufficient.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):236-245
DOI 10.1590/S0103-507X2012000300006
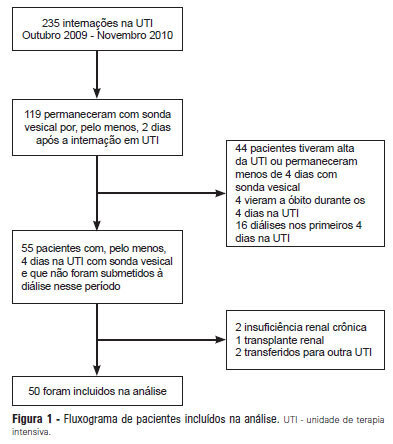
OBJECTIVE: Intensive care unit survivors and non-survivors have distinct acid-base profiles. The kidney's regulation of urinary electrolytes and the urinary strong ion difference plays a major role in acid-base homeostasis. The aim of this study was to evaluate the potential utility of daily spot urinary electrolyte measurement in acid-base and renal function monitoring. METHODS: We prospectively recorded daily plasma acid-base parameters and traditional markers of renal function in parallel with spot urinary electrolyte measurements in patients with urinary catheters admitted to our intensive care unit. Patients who remained in the intensive care unit for at least 4 days with a urinary catheter were included in the study. RESULTS: Of the 50 patients included in the study, 22% died during their intensive care unit stay. The incidence of acute kidney injury was significantly higher in non-survivors during the 4-day observation period (64% vs. 18% in survivors). Urinary chloride and sodium were lower and urinary strong ion difference was higher on day 1 in patients who developed acute kidney injury among both survivors and non-survivors. Both groups had similar urine output, although non-survivors had persistently higher urinary strong ion difference on all days. Survivors had a progressive improvement in metabolic acid-base profile due to increases in the plasma strong ion difference and decreases in weak acids. These changes were concomitant with decreases in urinary strong ion difference. In non-survivors, acid-base parameters did not significantly change during follow-up. CONCLUSIONS: Daily assessment of spot urinary electrolytes and strong ion difference are useful components of acid-base and renal function evaluations in critically ill patients, having distinct profiles between intensive care unit survivors and non-survivors.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):325-330
DOI 10.1590/S0103-507X2008000400002
OBJECTIVES: Sedation scores are important tools for use in pediatric intensive care units. The Comfort-Behavior scale is a valid method for the assessment of children although it is considered an extensive scale. The motor activity assessment scale is validated for an adult population. We considered it simpler then the one above and suitable for application in children. None of these scores had been translated into Portuguese. Our objective was to apply both scales in Portuguese to a pediatric population under mechanical ventilation. Secondary objectives were to evaluate the sedation level of children on mechanical ventilation in tertiary pediatric intensive care units and to compare the Comfort- Behavior and motor activity assessment scales in this population. METHODS: After translating the scales into Portuguese, both were simultaneously applied to 26 patients by 2 pediatricians. Each scale was applied 116 times in total. RESULTS: The intraclass correlation coefficient was 0.90 (0.85 - 0.93 CI 95%) for the Comfort-Behavior and 0.94 (0.92 - 0.96 CI 95%) for the motor activity assessment scale. When applying the Comfort-Behavior scale, the Crombach's alpha was 0.81 for observer A and 0.92 for observer B. The Spearman coefficient was 0.86 for observer A and 0.91 for observer B. These patients were found to be deeply sedated, showing low values in both scales. CONCLUSIONS: The scales were successfully translated into Portuguese and both were adequate to assess pain and sedation in the pediatric population under mechanical ventilation. Sedation level was high in this sample of applications.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):344-348
DOI 10.1590/S0103-507X2008000400005
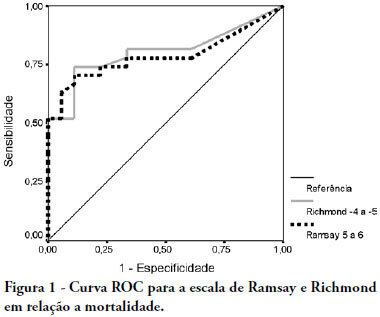
OBJECTIVE: The main purpose of this study was to compare performance of the Ramsay and Richmond sedation scores on mechanically ventilated critically ill patients, in a university-affiliated hospital. METHODS: This was a 4-month prospective study, which included a total of 45 patients mechanically ventilated, with at least 48 hours stay in the intensive care unit. Each patient was assessed daily for sedation mode, sedative and analgesic doses and sedation level using the Ramsay and Richmond scores. Statistical analysis was made using Student's t-test, Pearson's and Spearman's correlation, and constructing ROC-curves. RESULTS: A high general mortality of 60% was observed. The length of sedation and daily dose of medication did not correlate with mortality. Deep sedation (Ramsay > 4 or Richmond < -3) was positively correlated with probability of death with an AUC > 0.78. An adequate level of sedation (Ramsay 2 to 4 or Richmond 0 to -3) was sensitively correlated with probability of survival with an AUC > 0.80. A low level of sedation was observed in 63 days evaluated (8.64%), and no correlation was found between occurrence of agitation and unfavorable outcomes. Correlation between Ramsay and Richmond scores (Pearson's > 0.810 - p<0.0001) was good. CONCLUSION: In this study, Ramsay and Richmond sedation scores were similar for the assessment of deep, insufficient and adequate sedation. Both have good correlation with mortality in over sedated patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)