You searched for:"Leandro Utino Taniguchi"
We found (12) results for your search.-
Original Article
Comparison of the accuracy of residents, senior physicians and surrogate decision-makers for predicting hospital mortality of critically ill patients
Rev Bras Ter Intensiva. 2022;34(2):220-226
Abstract
Original ArticleComparison of the accuracy of residents, senior physicians and surrogate decision-makers for predicting hospital mortality of critically ill patients
Rev Bras Ter Intensiva. 2022;34(2):220-226
DOI 10.5935/0103-507X.20220019-en
Views2ABSTRACT
Objective:
To compare the predictive performance of residents, senior intensive care unit physicians and surrogates early during intensive care unit stays and to evaluate whether different presentations of prognostic data (probability of survival versus probability of death) influenced their performance.
Methods:
We questioned surrogates and physicians in charge of critically ill patients during the first 48 hours of intensive care unit admission on the patient’s probability of hospital outcome. The question framing (i.e., probability of survival versus probability of death during hospitalization) was randomized. To evaluate the predictive performance, we compared the areas under the ROC curves (AUCs) for hospital outcome between surrogates and physicians’ categories. We also stratified the results according to randomized question framing.
Results:
We interviewed surrogates and physicians on the hospital outcomes of 118 patients. The predictive performance of surrogate decisionmakers was significantly lower than that of physicians (AUC of 0.63 for surrogates, 0.82 for residents, 0.80 for intensive care unit fellows and 0.81 for intensive care unit senior physicians). There was no increase in predictive performance related to physicians’ experience (i.e., senior physicians did not predict outcomes better than junior physicians). Surrogate decisionmakers worsened their prediction performance when they were asked about probability of death instead of probability of survival, but there was no difference for physicians.
Conclusion:
Different predictive performance was observed when comparing surrogate decision-makers and physicians, with no effect of experience on health care professionals’ prediction. Question framing affected the predictive performance of surrogates but not of physicians.
Keywords:Critical illnessDecision MakingDelivery of health careHospitalizationIntensive care unitsInternship and residencyMortalityPrognosisSee more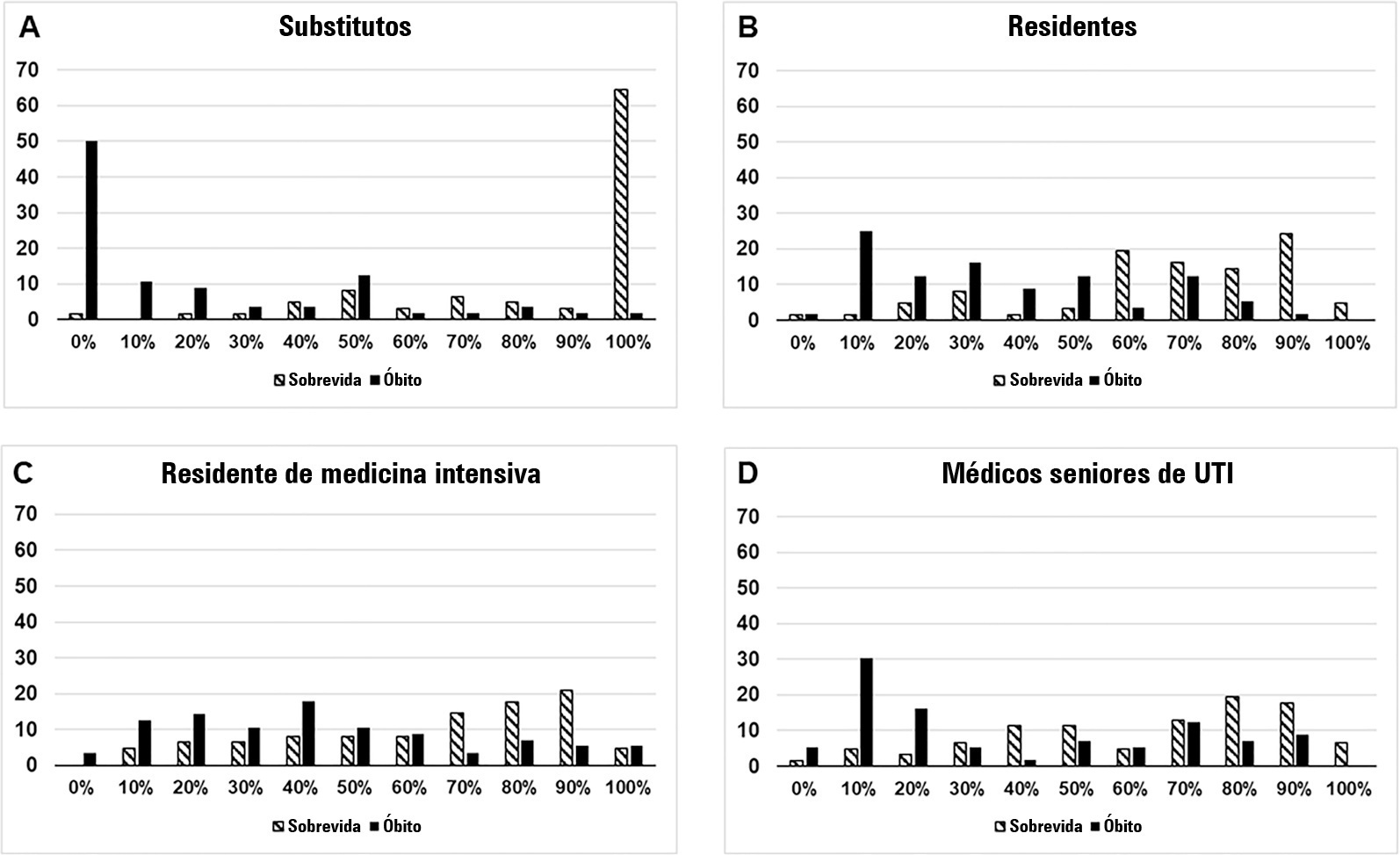
-
Letter to the Editor
Endotracheal intubation in COVID-19 patients in Brazil: a nationwide survey
Rev Bras Ter Intensiva. 2022;34(1):202-204
Abstract
Letter to the EditorEndotracheal intubation in COVID-19 patients in Brazil: a nationwide survey
Rev Bras Ter Intensiva. 2022;34(1):202-204
DOI 10.5935/0103-507X.20220015-en
Views2To the Editor Endotracheal intubation is a life-saving procedure in acute respiratory distress syndrome. However, complications such as hypoxia, hypotension and cardiovascular collapse may occur in almost 40% of the procedures in the intensive care unit (ICU).() Evidence regarding the best practice of endotracheal intubation in this context is scarce, and most data have been […]See more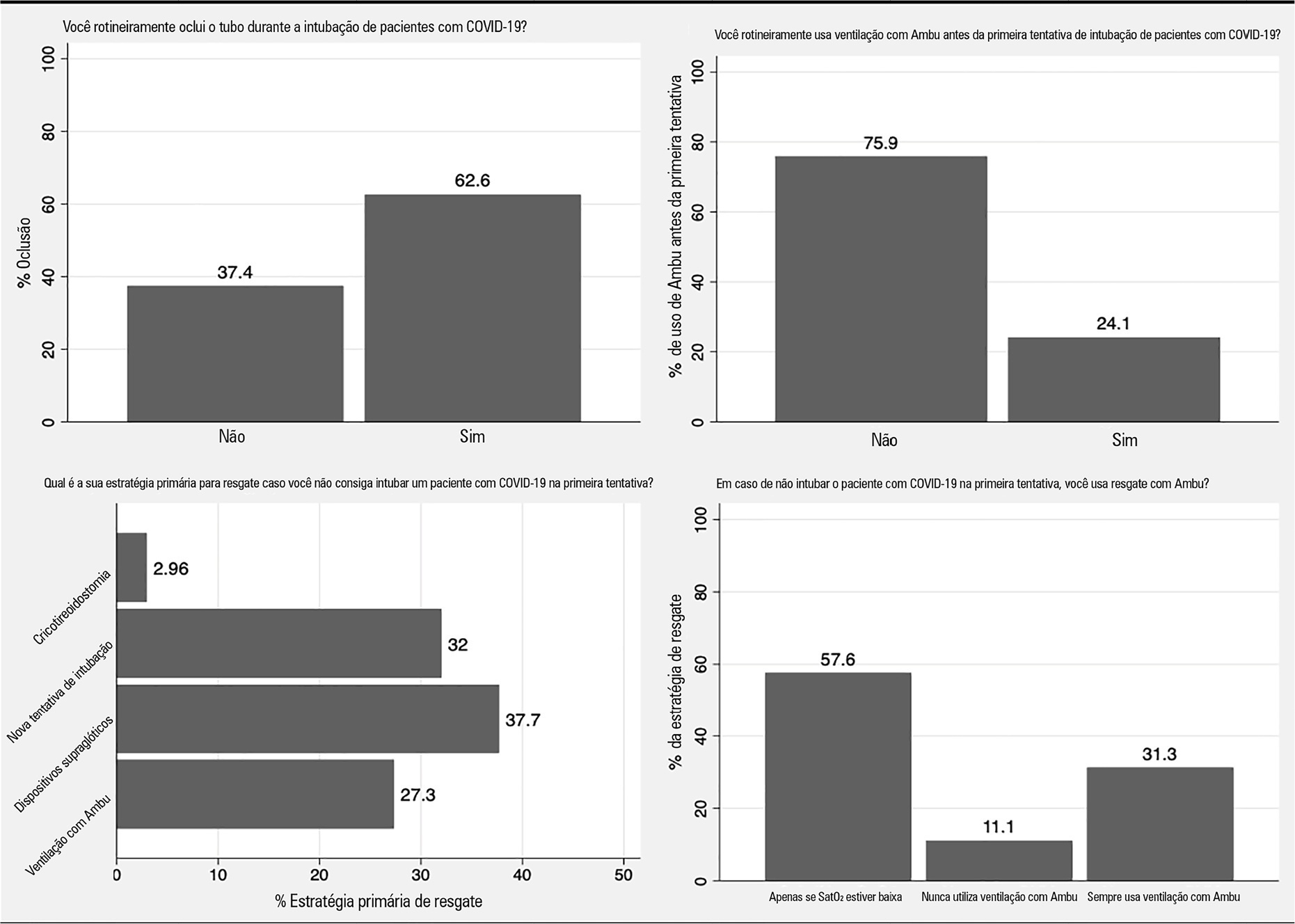
-
Original Article
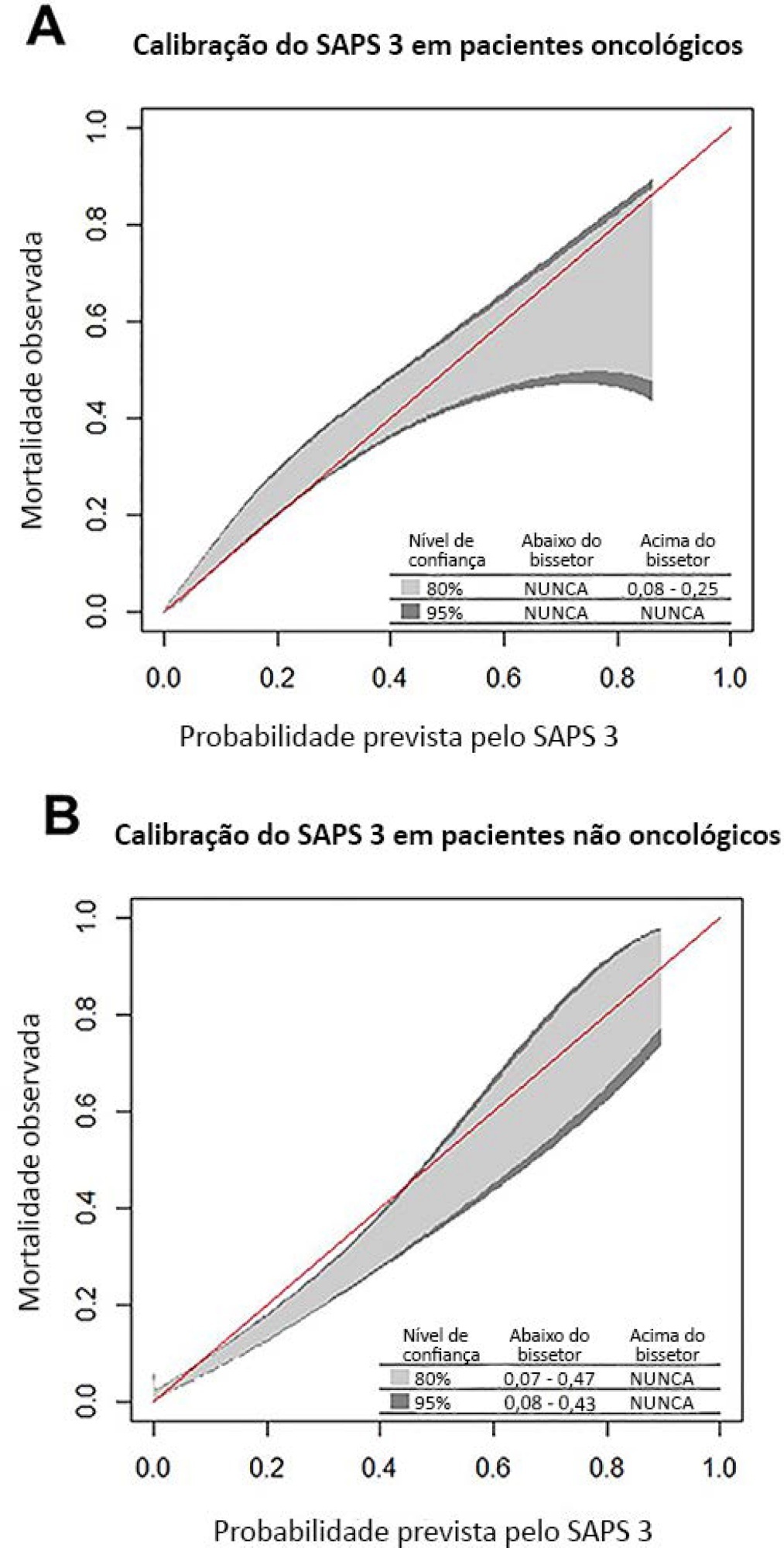
Comparison of SAPS 3 performance in patients with and without solid tumor admitted to an intensive care unit in Brazil: a retrospective cohort study
Rev Bras Ter Intensiva. 2020;32(4):521-527
Abstract
Original ArticleComparison of SAPS 3 performance in patients with and without solid tumor admitted to an intensive care unit in Brazil: a retrospective cohort study
Rev Bras Ter Intensiva. 2020;32(4):521-527
DOI 10.5935/0103-507X.20200089
Views1See moreABSTRACT
Objective:
To compare the performance of the Simplified Acute Physiology Score 3 (SAPS 3) in patients with and without solid cancer who were admitted to the intensive care unit of a comprehensive oncological hospital in Brazil.
Methods:
We performed a retrospective cohort analysis of our administrative database of the first admission of adult patients to the intensive care unit from 2012 to 2016. The patients were categorized according to the presence of solid cancer. We evaluated discrimination using the area under the Receiver Operating Characteristic curve (AUROC) and calibration using the calibration belt approach.
Results:
We included 7,254 patients (41.5% had cancer, and 12.1% died during hospitalization). Oncological patients had higher hospital mortality than nononcological patients (14.1% versus 10.6%, respectively; p < 0.001). SAPS 3 discrimination was better for oncological patients (AUROC = 0.85) than for nononcological patients (AUROC = 0.79) (p < 0.001). After we applied the calibration belt in oncological patients, the SAPS 3 matched the average observed rates with a confidence level of 95%. In nononcological patients, the SAPS 3 overestimated mortality in those with a low-middle risk. Calibration was affected by the time period only for nononcological patients.
Conclusion:
SAPS 3 performed differently between oncological and nononcological patients in our single-center cohort, and variation over time (mainly calibration) was observed. This finding should be taken into account when evaluating severity-of-illness score performance.
-
Original Article
Neuromuscular blockade and airway management during endotracheal intubation in Brazilian intensive care units: a national survey
Rev Bras Ter Intensiva. 2020;32(3):433-438
Abstract
Original ArticleNeuromuscular blockade and airway management during endotracheal intubation in Brazilian intensive care units: a national survey
Rev Bras Ter Intensiva. 2020;32(3):433-438
DOI 10.5935/0103-507X.20200073
Views0Abstract
Objective:
To describe the use of neuromuscular blockade as well as other practices among Brazilian physicians in adult intensive care units.
Methods:
An online national survey was designed and administered to Brazilian intensivists. Questions were selected using the Delphi method and assessed physicians’ demographic data, intensive care unit characteristics, practices regarding airway management, use of neuromuscular blockade and sedation during endotracheal intubation in the intensive care unit. As a secondary outcome, we applied a multivariate analysis to evaluate factors associated with the use of neuromuscular blockade.
Results:
Five hundred sixty-five intensivists from all Brazilian regions responded to the questionnaire. The majority of respondents were male (65%), with a mean age of 38 ( 8.4 years, and 58.5% had a board certification in critical care. Only 40.7% of the intensivists reported the use of neuromuscular blockade during all or in more than 75% of endotracheal intubations. In the multivariate analysis, the number of intubations performed monthly and physician specialization in anesthesiology were directly associated with frequent use of neuromuscular blockade. Etomidate and ketamine were more commonly used in the clinical situation of hypotension and shock, while propofol and midazolam were more commonly prescribed in the situation of clinical stability.
Conclusion:
The reported use of neuromuscular blockade was low among intensivists, and sedative drugs were chosen in accordance with patient hemodynamic stability. These results may help the design of future studies regarding airway management in Brazil.
Keywords:Airway managementBrazilHypnotics and sedativesIntensive care unitsIntubationNeuromuscular blockadeSee more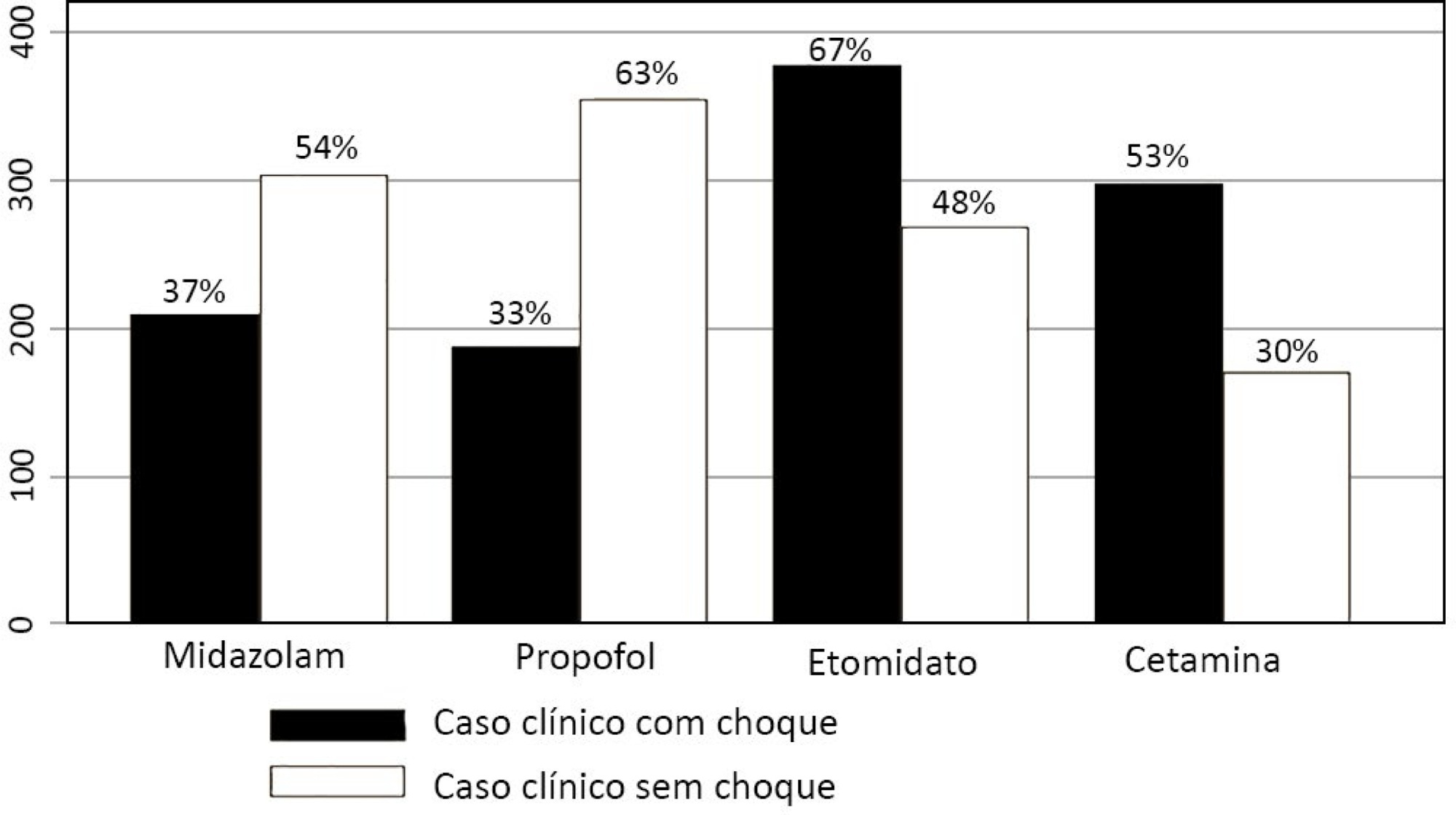
-
Original Article
Practices for promoting sleep in intensive care units in Brazil: a national survey
Rev Bras Ter Intensiva. 2020;32(2):268-276
Abstract
Original ArticlePractices for promoting sleep in intensive care units in Brazil: a national survey
Rev Bras Ter Intensiva. 2020;32(2):268-276
DOI 10.5935/0103-507X.20200043
Views0See moreABSTRACT
Objective:
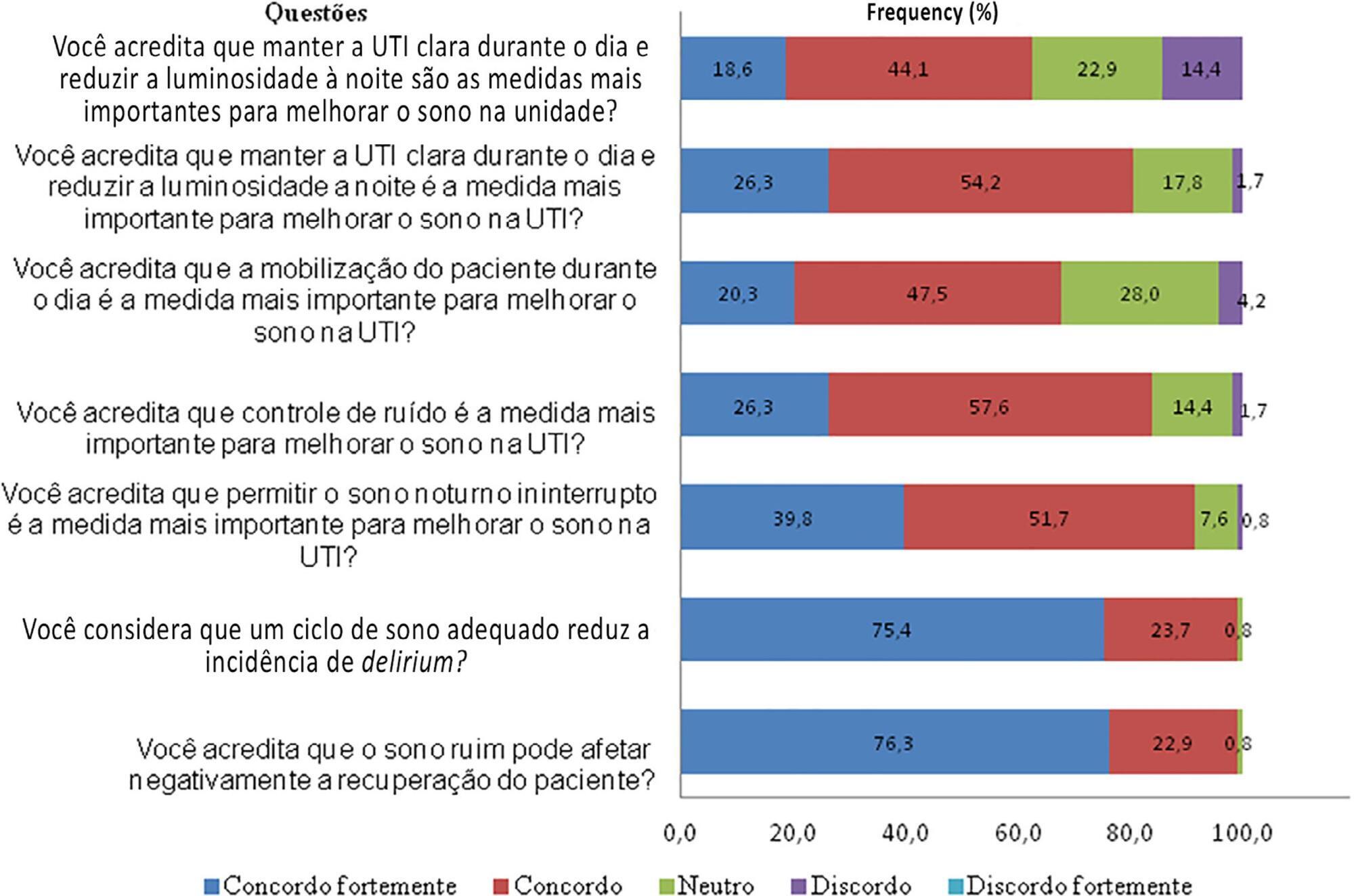
To conduct a national survey of intensive care professionals to identify the practices for promoting sleep in adult intensive care units in Brazil and describe the professionals’ perceptions of the importance of sleep for patients.
Methods:
An electronic questionnaire was distributed by the clinical research cooperation network of the Associação de Medicina Intensiva Brasileira and by the Brazilian Research in Intensive Care Network to physicians and nurses registered with the association. The questionnaire evaluated the profile of the respondents, the profile of their intensive care units, whether protocols for promoting sleep were present, the pharmacological and nonpharmacological measures typically employed in the unit, and the professionals’ perceptions regarding sleep in critically ill patients.
Results:
A total of 118 questionnaires were evaluated. The Southeast region of the country was the most represented (50 questionnaires, 42.4%). The majority of units had a clinical-surgical profile (93 questionnaires; 78.8%), and 26 had a continuous visitation policy (22.0%). Only 18 intensive care units (15.3%) reported having protocols for promoting sleep. The most cited measure for sleep promotion was reducing light during the night (95 questionnaires; 80.5%), which was more often performed in private intensive care units. Almost all of the responders (99%) believed that poor-quality sleep has a negative impact on patient recovery.
Conclusion:
The responses to this Brazilian survey revealed that few intensive care units had a program for promoting sleep, although almost all participants recognized the importance of sleep in patient recovery.
-
Original Article
Adherence to a stress ulcer prophylaxis protocol by critically ill patients: a prospective cohort study
Rev Bras Ter Intensiva. 2020;32(1):37-42
Abstract
Original ArticleAdherence to a stress ulcer prophylaxis protocol by critically ill patients: a prospective cohort study
Rev Bras Ter Intensiva. 2020;32(1):37-42
DOI 10.5935/0103-507X.20200007
Views0ABSTRACT
Objective:
To evaluate adherence to the stress ulcer prophylaxis protocol in critically ill patients at a tertiary university hospital.
Methods:
In this prospective cohort study, we included all adult patients admitted to the medical and surgical intensive care units of an academic tertiary hospital. Our sole exclusion criterion was upper gastrointestinal bleeding at intensive care unit admission. We collected baseline variables and stress ulcer prophylaxis indications according to the institutional protocol and use of prophylaxis. Our primary outcome was adherence to the stress ulcer prophylaxis protocol. Secondary outcomes were appropriate use of stress ulcer prophylaxis, upper gastrointestinal bleeding incidence and factors associated with appropriate use of stress ulcer prophylaxis.
Results:
Two hundred thirty-four patients were enrolled from July 2nd through July 31st, 2018. Patients were 52 ± 20 years old, 125 (53%) were surgical patients, and the mean SAPS 3 was 52 ± 20. In the longitudinal follow-up, 1499 patient-days were studied; 1069 patient-days had stress ulcer prophylaxis indications, and 777 patient-days contained prophylaxis use (73% stress ulcer prophylaxis protocol adherence). Of the 430 patient-days without stress ulcer prophylaxis indications, 242 involved prophylaxis (56% inappropriate stress ulcer prophylaxis use). The overall appropriate use of stress ulcer prophylaxis was 64%. Factors associated with proper stress ulcer prophylaxis prescription were mechanical ventilation OR 2.13 (95%CI 1.64 – 2.75) and coagulopathy OR 2.77 (95%CI 1.66 – 4.60). The upper gastrointestinal bleeding incidence was 12.8%.
Conclusion:
Adherence to the stress ulcer prophylaxis protocol was low and inappropriate use of stress ulcer prophylaxis was frequent in this cohort of critically ill patients.
Keywords:Anti-ulcer agentsCritical careCritical illnessGastrointestinal hemorrhagePeptic ulcerTherapeutic adherence complianceSee more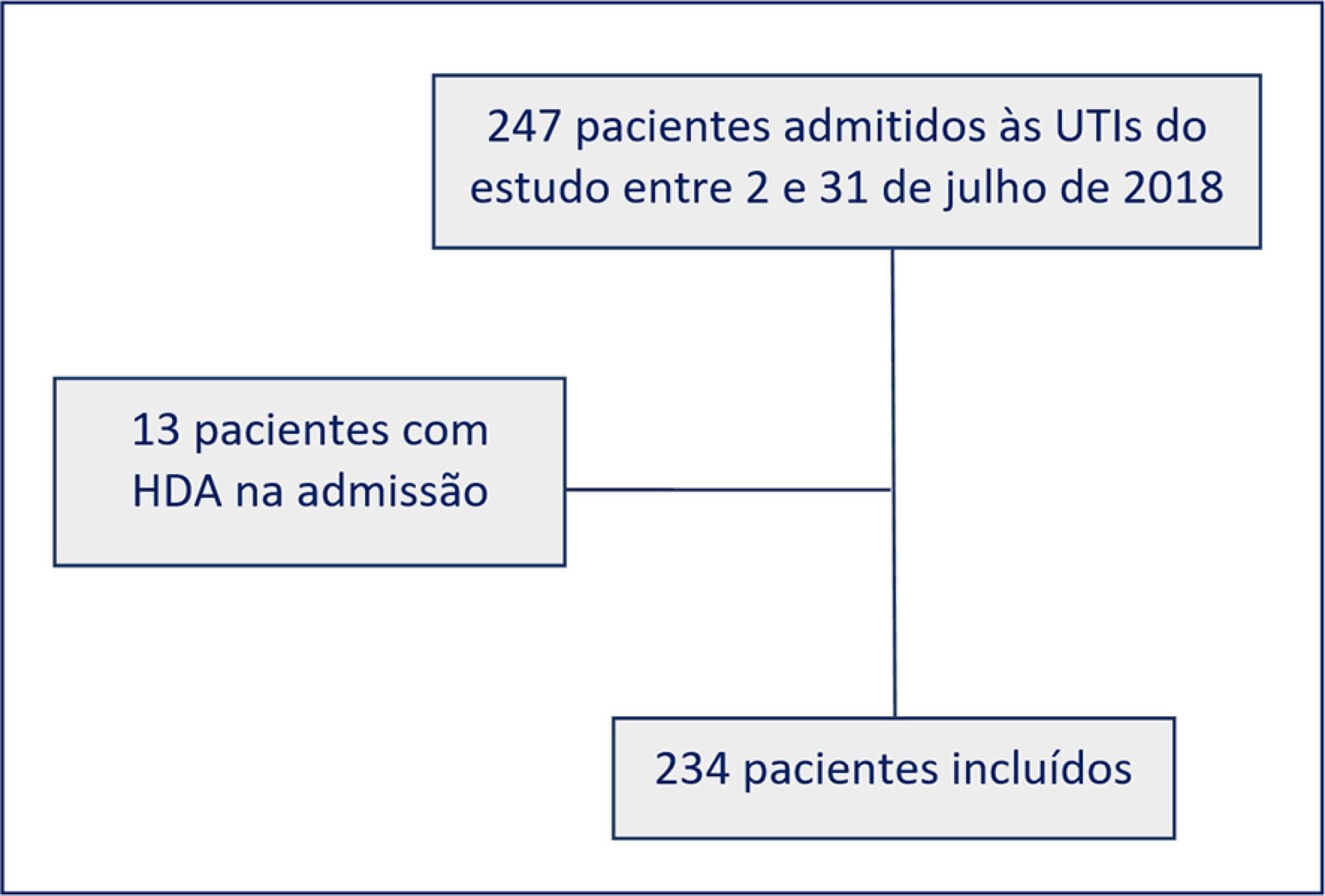
-
Original Article
Availability of resources to treat sepsis in Brazil: a random sample of Brazilian institutions
Rev Bras Ter Intensiva. 2019;31(2):193-201
Abstract
Original ArticleAvailability of resources to treat sepsis in Brazil: a random sample of Brazilian institutions
Rev Bras Ter Intensiva. 2019;31(2):193-201
DOI 10.5935/0103-507X.20190033
Views1ABSTRACT
Objective:
To characterize resource availability from a nationally representative random sample of intensive care units in Brazil.
Methods:
A structured online survey of participating units in the Sepsis PREvalence Assessment Database (SPREAD) study, a nationwide 1-day point prevalence survey to assess the burden of sepsis in Brazil, was sent to the medical director of each unit.
Results:
A representative sample of 277 of the 317 invited units responded to the resources survey. Most of the hospitals had fewer than 500 beds (94.6%) with a median of 14 beds in the intensive care unit. Providing care for public-insured patients was the main source of income in two-thirds of the surveyed units. Own microbiology laboratory was not available for 26.8% of the surveyed intensive care units, and 10.5% did not always have access to blood cultures. Broad spectrum antibiotics were not always available in 10.5% of surveyed units, and 21.3% could not always measure lactate within three hours. Those institutions with a high resource availability (158 units, 57%) were usually larger and preferentially served patients from the private health system compared to institutions without high resource availability. Otherwise, those without high resource availability did not always have broad-spectrum antibiotics (24.4%), vasopressors (4.2%) or crystalloids (7.6%).
Conclusion:
Our study indicates that a relevant number of units cannot perform basic monitoring and therapeutic interventions in septic patients. Our results highlight major opportunities for improvement to adhere to simple but effective interventions in Brazil.
Keywords:Brazil/epidemiologyCritical careDeveloping countriesEpidemiological monitoringHealth resourcesIntensive care unitsSepsis/epidemiologyTherapeuticsSee more -
Articles
Systemic inflammatory response syndrome criteria and the prediction of hospital mortality in critically ill patients: a retrospective cohort study
Rev Bras Ter Intensiva. 2017;29(3):317-324
Abstract
ArticlesSystemic inflammatory response syndrome criteria and the prediction of hospital mortality in critically ill patients: a retrospective cohort study
Rev Bras Ter Intensiva. 2017;29(3):317-324
DOI 10.5935/0103-507X.20170047
Views1See moreABSTRACT
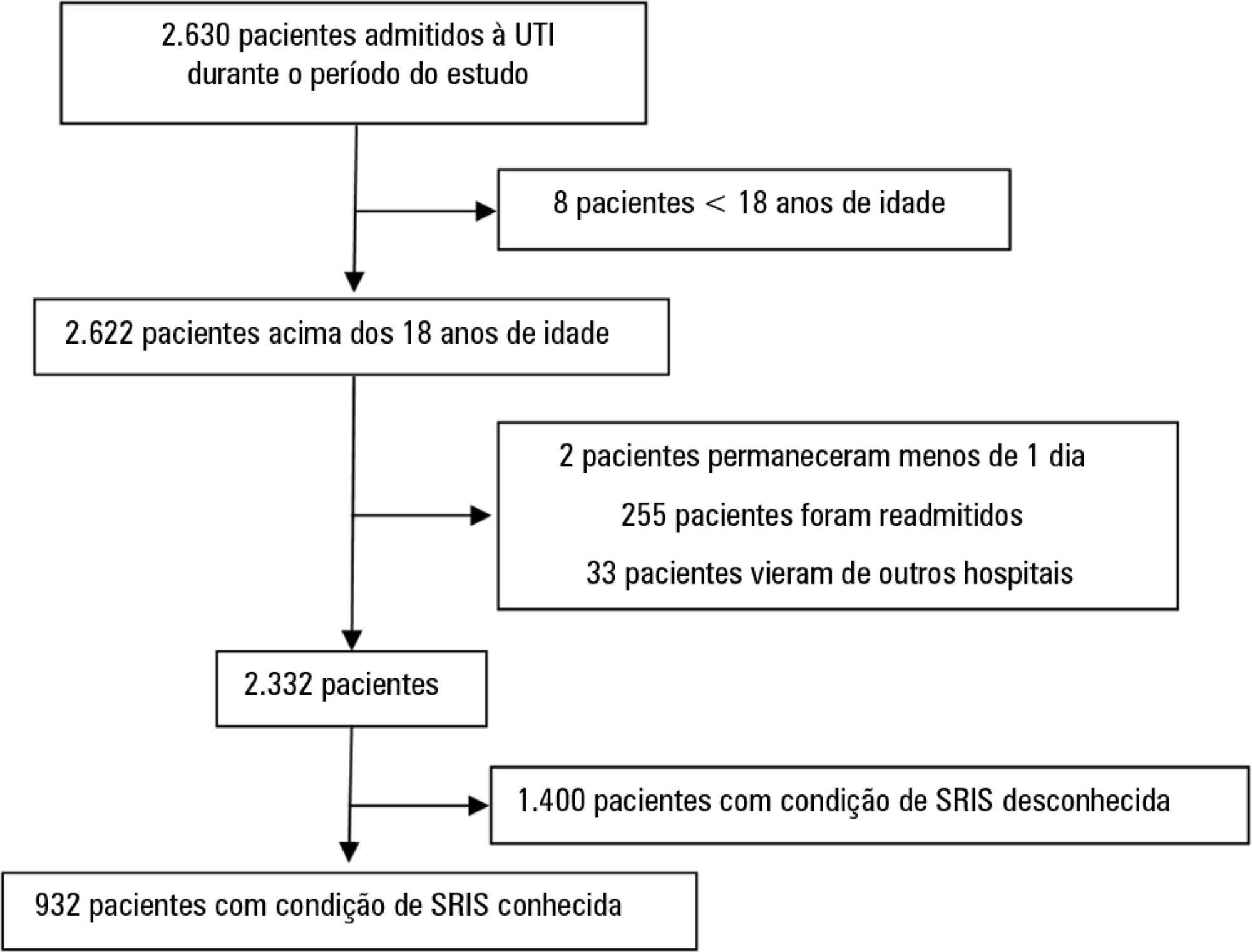
Objective:
This study intended to determine whether the systemic inflammatory response syndrome criteria can predict hospital mortality in a Brazilian cohort of critically ill patients.
Methods:
We performed a retrospective cohort study at a private tertiary hospital in São Paulo (SP), Brazil. We extracted information from the adult intensive care unit database (Sistema EpimedTM). We compared the SAPS 3 and the systemic inflammatory response syndrome model as dichotomous (≥ 2 criteria: systemic inflammatory response syndrome -positive versus 0 – 1 criterion: systemic inflammatory response syndrome -negative) and ordinal variables from 0 to 4 (according to the number of systemic inflammatory response syndrome criteria met) in the prediction of hospital mortality at intensive care unit admission. Model discrimination was compared using the area under the receiver operating characteristics (AUROC) curve.
Results:
From January to December 2012, we studied 932 patients (60.4% were systemic inflammatory response syndrome -positive). systemic inflammatory response syndrome -positive patients were more critically ill than systemic inflammatory response syndrome -negative patients and had higher hospital mortality (16.9% versus 8.1%, p < 0.001). In the adjusted analysis, being systemic inflammatory response syndrome -positive independently increased the risk of death by 82% (odds ratio 1.82; 95% confidence interval [CI] 1.12 - 2.96, p = 0.016). However, the AUROC curve for the SAPS 3 model was higher (0.81, 95%CI 0.78 - 0.85) compared to the systemic inflammatory response syndrome model with the systemic inflammatory response syndrome criteria as a dichotomous variable (0.60, 95%CI 0.55 - 0.65) and as an ordinal variable (0.62, 95%CI 0.57 - 0.68; p < 0.001) for hospital mortality.
Conclusion:
Although systemic inflammatory response syndrome is associated with hospital mortality, the systemic inflammatory response syndrome criteria show low accuracy in the prediction of mortality compared with the SAPS 3.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




