Abstract
Rev Bras Ter Intensiva. 2019;31(1):47-56
DOI 10.5935/0103-507X.20190011
To determine the association between the primary site of infection and in-hospital mortality as the main outcome, or the need for admission to the intensive care unit as a secondary outcome, in patients with sepsis admitted to the emergency department.
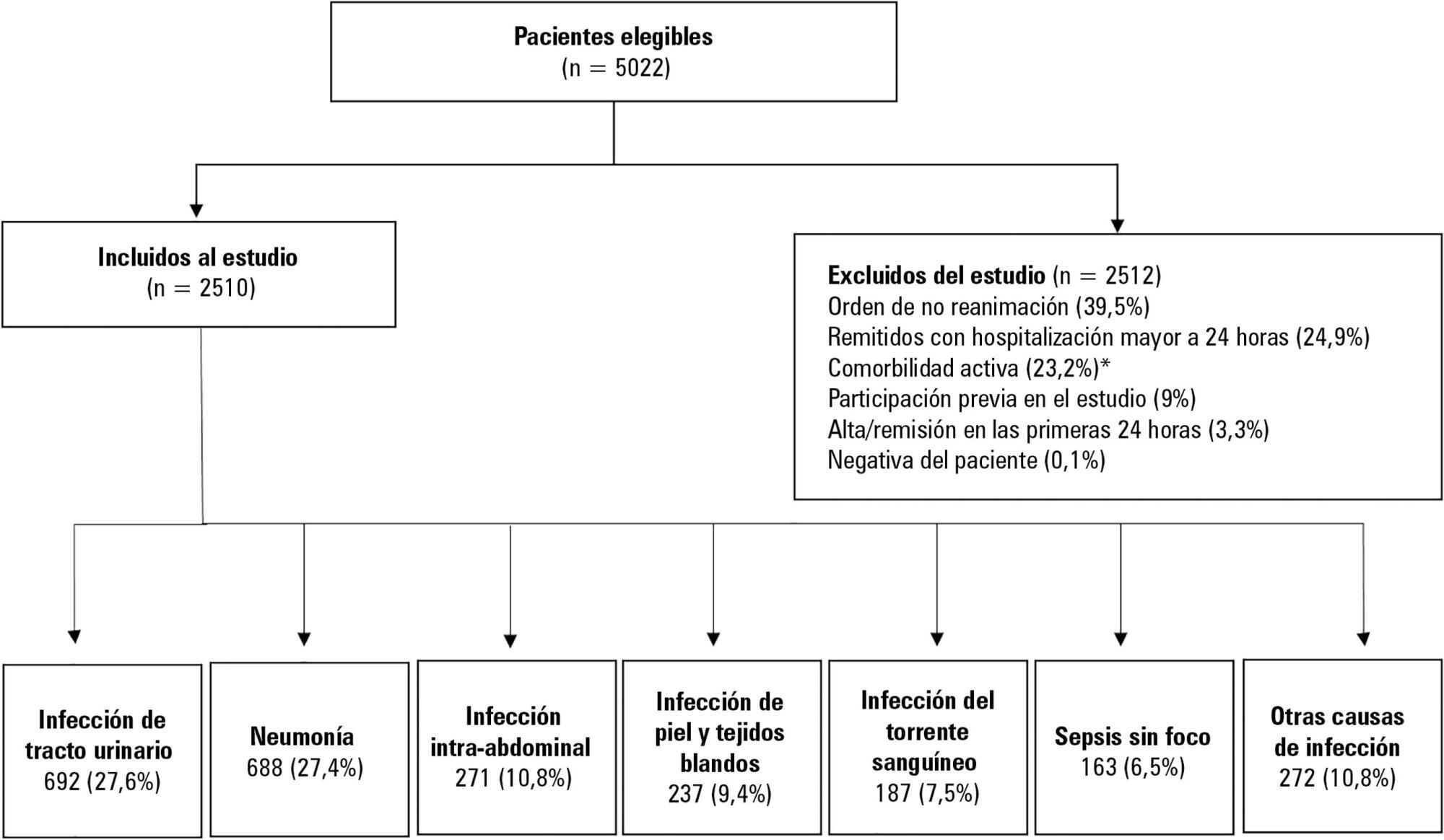
This was a secondary analysis of a multicenter prospective cohort. Patients included in the study were older than 18 years with a diagnosis of severe sepsis or septic shock who were admitted to the emergency departments of three tertiary care hospitals. Of the 5022 eligible participants, 2510 were included. Multiple logistic regression analysis was performed for mortality.
The most common site of infection was the urinary tract, present in 27.8% of the cases, followed by pneumonia (27.5%) and intra-abdominal focus (10.8%). In 5.4% of the cases, no definite site of infection was identified on admission. Logistic regression revealed a significant association between the following sites of infection and in-hospital mortality when using the urinary infection group as a reference: pneumonia (OR 3.4; 95%CI, 2.2 - 5.2; p < 0.001), skin and soft tissues (OR 2.6; 95%CI, 1.4 - 5.0; p = 0.003), bloodstream (OR 2.0; 95%CI, 1.1 - 3.6; p = 0.018), without specific focus (OR 2.0; 95%CI, 1.1 - 3.8; p = 0.028), and intra-abdominal focus (OR 1.9; 95%CI, 1.1 - 3.3; p = 0.024).
There is a significant association between the different sites of infection and in-hospital mortality or the need for admission to an intensive care unit in patients with sepsis or septic shock. Urinary tract infection shows the lowest risk, which should be considered in prognostic models of these conditions.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):317-324
DOI 10.5935/0103-507X.20170047
This study intended to determine whether the systemic inflammatory response syndrome criteria can predict hospital mortality in a Brazilian cohort of critically ill patients.
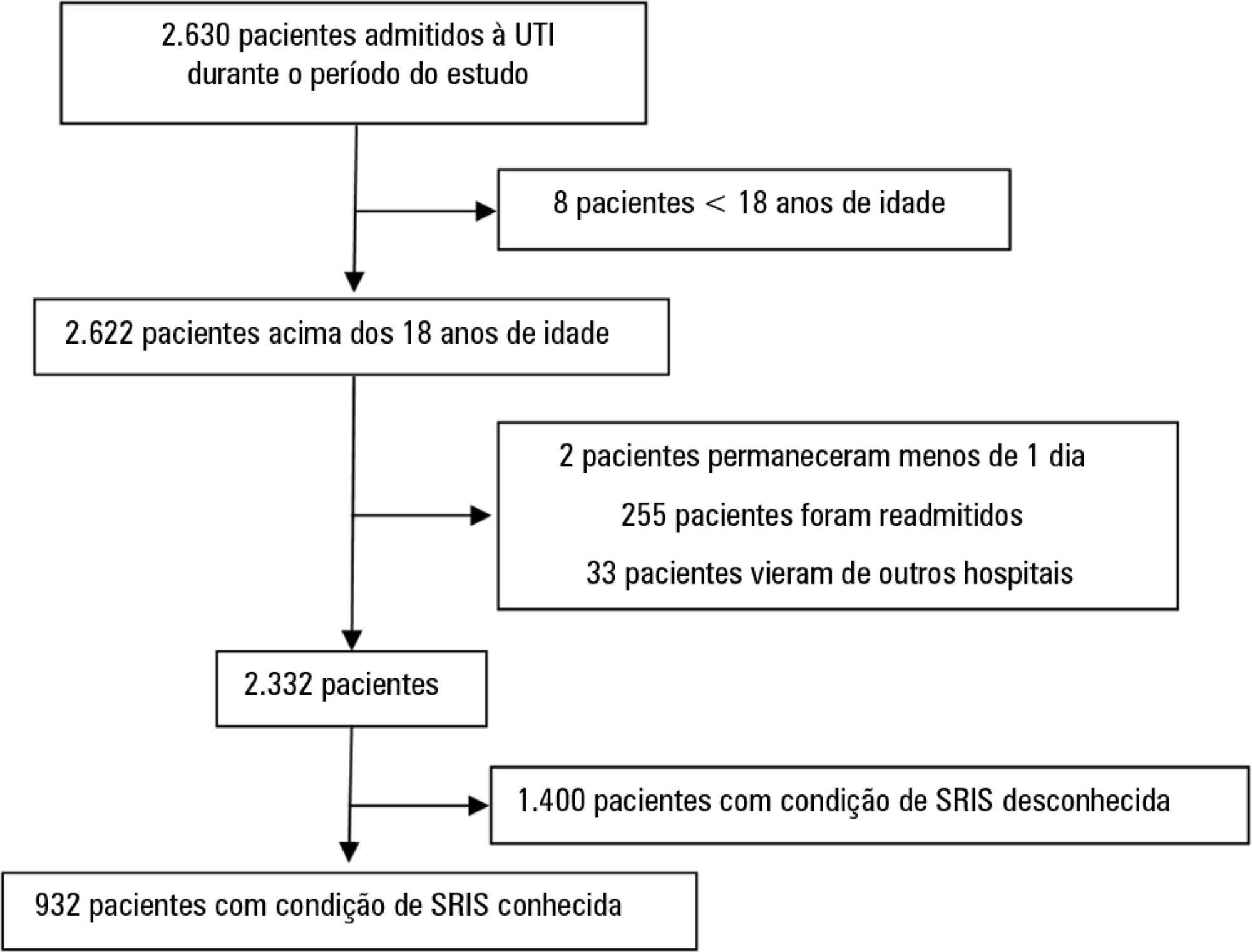
We performed a retrospective cohort study at a private tertiary hospital in São Paulo (SP), Brazil. We extracted information from the adult intensive care unit database (Sistema EpimedTM). We compared the SAPS 3 and the systemic inflammatory response syndrome model as dichotomous (≥ 2 criteria: systemic inflammatory response syndrome -positive versus 0 - 1 criterion: systemic inflammatory response syndrome -negative) and ordinal variables from 0 to 4 (according to the number of systemic inflammatory response syndrome criteria met) in the prediction of hospital mortality at intensive care unit admission. Model discrimination was compared using the area under the receiver operating characteristics (AUROC) curve.
From January to December 2012, we studied 932 patients (60.4% were systemic inflammatory response syndrome -positive). systemic inflammatory response syndrome -positive patients were more critically ill than systemic inflammatory response syndrome -negative patients and had higher hospital mortality (16.9% versus 8.1%, p < 0.001). In the adjusted analysis, being systemic inflammatory response syndrome -positive independently increased the risk of death by 82% (odds ratio 1.82; 95% confidence interval [CI] 1.12 - 2.96, p = 0.016). However, the AUROC curve for the SAPS 3 model was higher (0.81, 95%CI 0.78 - 0.85) compared to the systemic inflammatory response syndrome model with the systemic inflammatory response syndrome criteria as a dichotomous variable (0.60, 95%CI 0.55 - 0.65) and as an ordinal variable (0.62, 95%CI 0.57 - 0.68; p < 0.001) for hospital mortality.
Although systemic inflammatory response syndrome is associated with hospital mortality, the systemic inflammatory response syndrome criteria show low accuracy in the prediction of mortality compared with the SAPS 3.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):179-189
DOI 10.5935/0103-507X.20160019
Lower respiratory tract infections are common and potentially lethal conditions and are a major cause of inadequate antibiotic prescriptions. Characterization of disease severity and prognostic prediction in affected patients can aid disease management and can increase accuracy in determining the need for and place of hospitalization. The inclusion of biomarkers, particularly procalcitonin, in the decision taken process is a promising strategy. This study aims to present a narrative review of the potential applications and limitations of procalcitonin as a prognostic marker in hospitalized patients with lower respiratory tract infections. The studies on this topic are heterogeneous with respect to procalcitonin measurement techniques, cutoff values, clinical settings, and disease severity. The results show that procalcitonin delivers moderate performance for prognostic prediction in patients with lower respiratory tract infections; its predictive performance was not higher than that of classical methods, and knowledge of procalcitonin levels is most useful when interpreted together with other clinical and laboratory results. Overall, repeated measurement of the procalcitonin levels during the first days of treatment provides more prognostic information than a single measurement; however, information on the cost-effectiveness of this procedure in intensive care patients is lacking. The results of studies that evaluated the prognostic value of initial procalcitonin levels in patients with community-acquired pneumonia are more consistent and have greater potential for practical application; in this case, low procalcitonin levels identify those patients with a low risk of adverse outcomes.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):260-265
DOI 10.5935/0103-507X.20150047
>To evaluate the agreement between a new epidemiological surveillance method of the Center for Disease Control and Prevention and the clinical pulmonary infection score for mechanical ventilator-associated pneumonia detection.
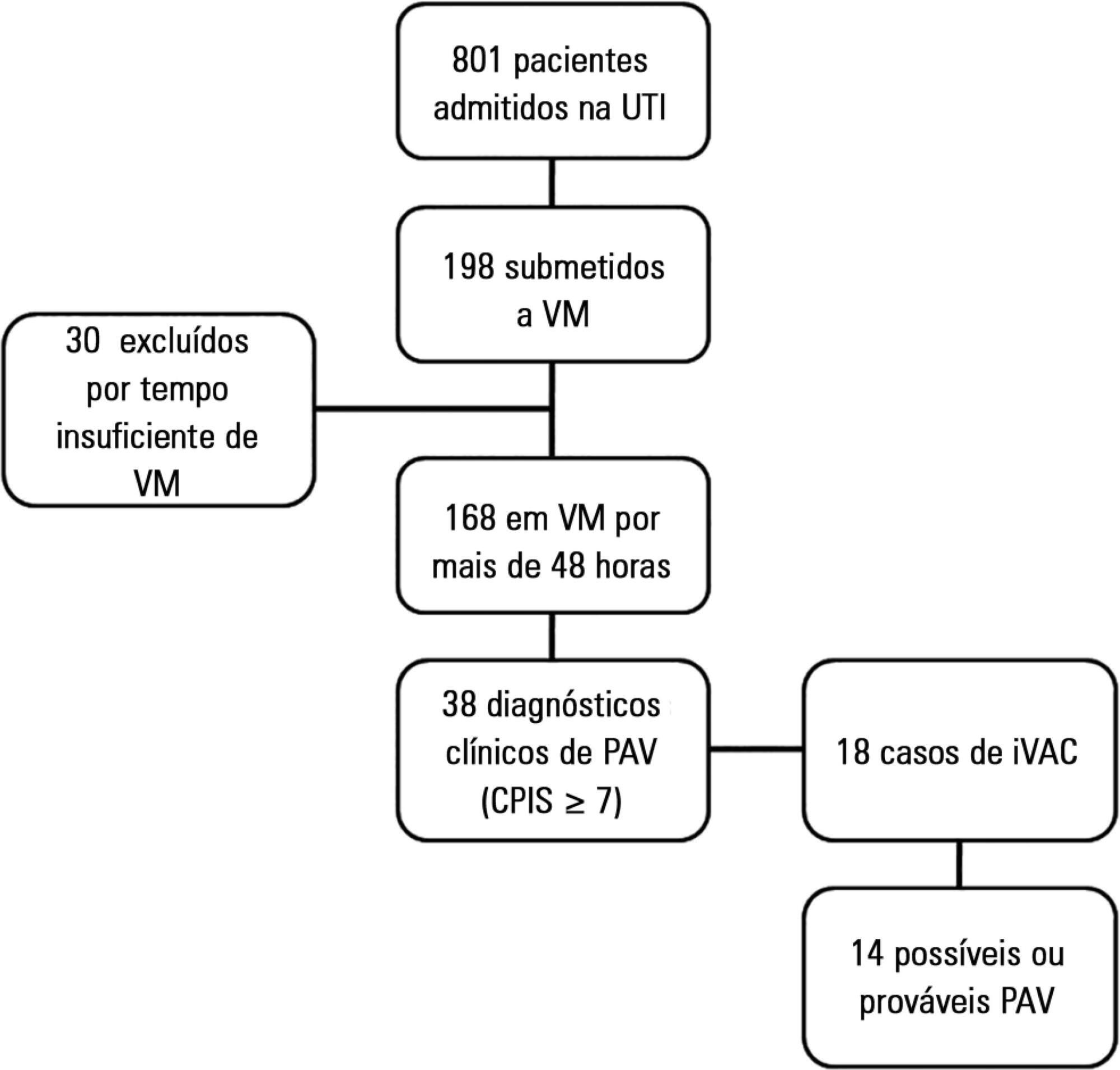
This was a prospective cohort study that evaluated patients in the intensive care units of two hospitals who were intubated for more than 48 hours between August 2013 and June 2014. Patients were evaluated daily by physical therapist using the clinical pulmonary infection score. A nurse independently applied the new surveillance method proposed by the Center for Disease Control and Prevention. The diagnostic agreement between the methods was evaluated. A clinical pulmonary infection score of ≥ 7 indicated a clinical diagnosis of mechanical ventilator-associated pneumonia, and the association of a clinical pulmonary infection score ≥ 7 with an isolated semiquantitative culture consisting of ≥ 104 colony-forming units indicated a definitive diagnosis.
Of the 801 patients admitted to the intensive care units, 198 required mechanical ventilation. Of these, 168 were intubated for more than 48 hours. A total of 18 (10.7%) cases of mechanical ventilation-associated infectious conditions were identified, 14 (8.3%) of which exhibited possible or probable mechanical ventilatorassociated pneumonia, which represented 35% (14/38) of mechanical ventilator-associated pneumonia cases. The Center for Disease Control and Prevention method identified cases of mechanical ventilator-associated pneumonia with a sensitivity of 0.37, specificity of 1.0, positive predictive value of 1.0, and negative predictive value of 0.84. The differences resulted in discrepancies in the mechanical ventilator-associated pneumonia incidence density (CDC, 5.2/1000 days of mechanical ventilation; clinical pulmonary infection score ≥ 7, 13.1/1000 days of mechanical ventilation).
The Center for Disease Control and Prevention method failed to detect mechanical ventilatorassociated pneumonia cases and may not be satisfactory as a surveillance method.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):68-72
DOI 10.1590/S0103-507X2013000100013
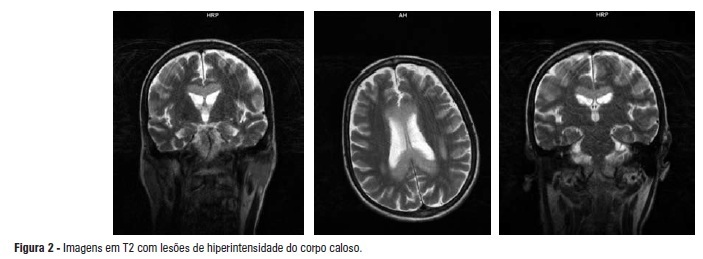
Marchiafava-Bignami disease is a rare affliction characterized by primary degeneration of the corpus callosum associated with chronic consumption of ethanol. The disease may occasionally occur in patients who are not alcoholics but are chronically malnourished. A complex deficiency of group B vitamins is the main etiopathogenic hypothesis, and many patients improve after the administration of these compounds. However, a good response is not always observed. The definitive diagnosis of Marchiafava-Bignami disease can be problematic and is based on features of neuroimaging studies, especially magnetic resonance imaging. Its treatment is still controversial and shows variable results. Because nutritional factors are implicated, as in Wernicke's encephalopathy, some authors claim that replacement of B vitamins is beneficial. The present article is a case report of a severe acute form of Marchiafava-Bignami disease in an alcohol-dependent male patient who improved after the administration of parenteral B vitamins. As a consequence of his neurological and immunologic conditions, he developed multiple pulmonary infections and had a protracted course in the intensive care unit. He eventually died of sepsis associated with an uncommon fungus, Rhodotorula mucilaginosa. The present article reports the clinical and neuroimaging data from this patient and contains a review of Marchiafava-Bignami disease and Rhodotorula infections in the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):270-278
DOI 10.5935/0103-507X.20130047
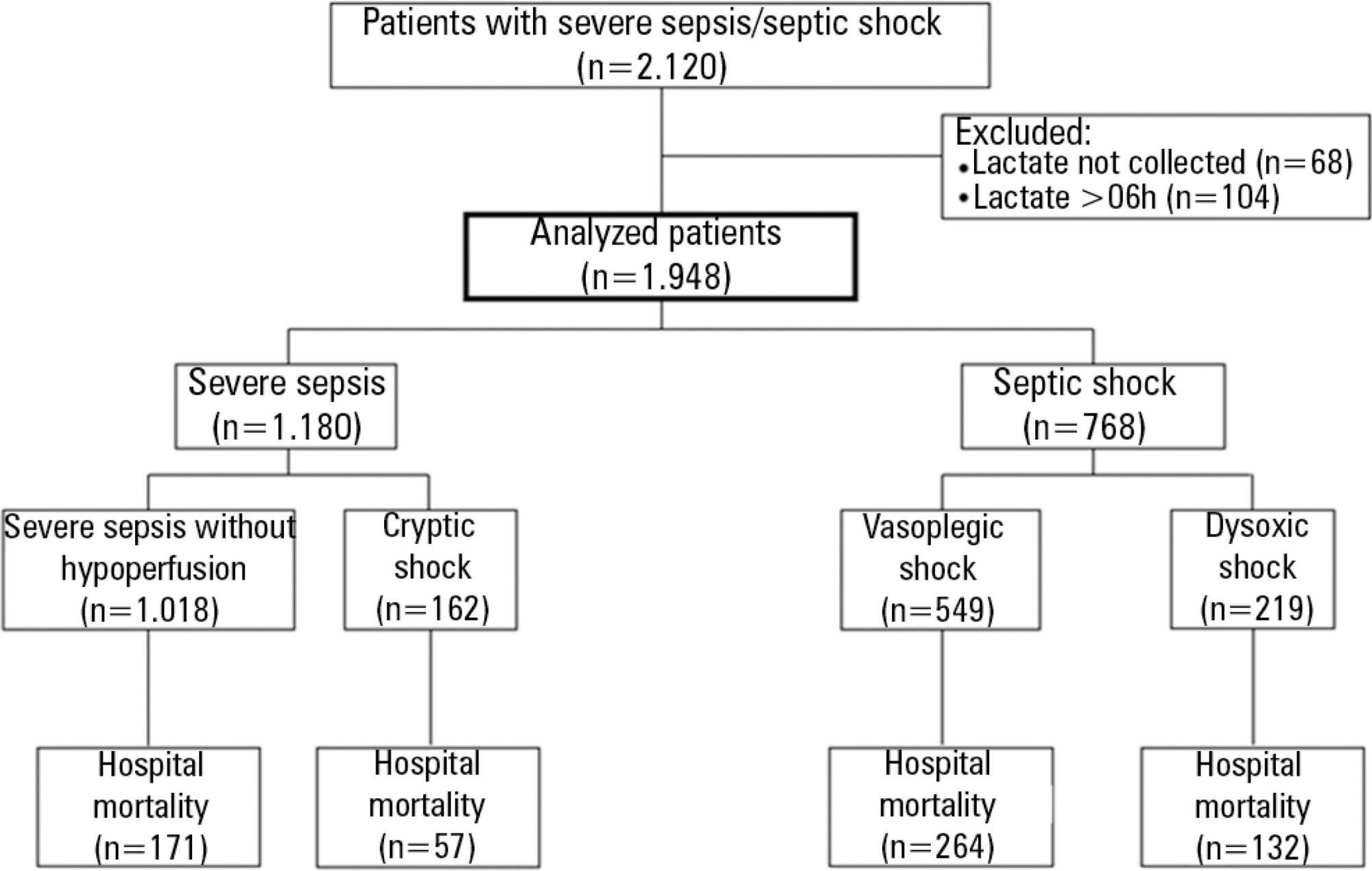
The current definition of severe sepsis and septic shock includes a heterogeneous profile of patients. Although the prognostic value of hyperlactatemia is well established, hyperlactatemia is observed in patients with and without shock. The present study aimed to compare the prognosis of septic patients by stratifying them according to two factors: hyperlactatemia and persistent hypotension.
The present study is a secondary analysis of an observational study conducted in ten hospitals in Brazil (Rede Amil - SP). Septic patients with initial lactate measurements in the first 6 hours of diagnosis were included and divided into 4 groups according to hyperlactatemia (lactate >4mmol/L) and persistent hypotension: (1) severe sepsis (without both criteria); (2) cryptic shock (hyperlactatemia without persistent hypotension); (3) vasoplegic shock (persistent hypotension without hyperlactatemia); and (4) dysoxic shock (both criteria).
In total, 1,948 patients were analyzed, and the sepsis group represented 52% of the patients, followed by 28% with vasoplegic shock, 12% with dysoxic shock and 8% with cryptic shock. Survival at 28 days differed among the groups (p<0.001). Survival was highest among the severe sepsis group (69%, p<0.001 versus others), similar in the cryptic and vasoplegic shock groups (53%, p=0.39), and lowest in the dysoxic shock group (38%, p<0.001 versus others). In the adjusted analysis, the survival at 28 days remained different among the groups (p<0.001) and the dysoxic shock group exhibited the highest hazard ratio (HR=2.99, 95%CI 2.21-4.05).
The definition of sepsis includes four different profiles if we consider the presence of hyperlactatemia. Further studies are needed to better characterize septic patients, to understand the etiology and to design adequate targeted treatments.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):143-150
DOI 10.1590/S0103-507X2012000200008
OBJECTIVE: To determine the prevalence of infections in Brazilian intensive care units and the associated mortality by analyzing the data obtained in the Extended Prevalence of Infection in Intensive Care (EPIC II) study. METHODS: EPIC II was a multicenter, international, cross-sectional prospective study of infection prevalence. It described the demographic, physiological, bacteriological, and therapeutic characteristics, outcome up to the 60th day, prevalence of infection, and mortality of all the patients admitted to the participating ICUs between zero hour and midnight on May 8, 2007. A total of 14,414 patients were included in the original study. Of these 14,414 patients, 1,235 were Brazilian and were hospitalized in 90 Brazilian ICUs. They represent the focus of this study. RESULTS: Among these 1,235 Brazilian patients, 61,6% had an infection on the day of the trial, and the lungs were the main site of infection (71.2%). Half of the patients had positive cultures, predominantly gram-negative bacilli (72%). On the day of the study, the median SOFA score was 5 (3-8) and the median SAPS II score was 36 (26-47). The infected patients had SOFA scores significantly higher than those of the non-infected patients 6 (4-9) and 3 (2-6), respectively). The overall ICU mortality rate was 28.4%: 37.6% in the infected patients, and 13.2% in the non-infected patients (p<0.001). Similarly, the in-hospital mortality rate was 34.2%, with a higher rate in the infected than in the non-infected patients (44.2% vs. 17.7%) (p<0.001). In the multivariate analysis, the main factors associated with infection incidence were emergency surgery (OR 2.89, 95%CI [1.72-4.86], p<0.001), mechanical ventilation (OR 2.06, 95% CI [1.5-2.82], p<0.001), and the SAPS II score (OR 1.04, 95% CI [1.03-1.06], p<0.001). The main factors related to mortality were ICC functional class III/ IV (OR 3.0, 95% CI [1.51-5.98], p<0.01), diabetes mellitus (OR 0.48, 95% CI [0.25-0.95], p<0.03), cirrhosis (OR 4.62, 95% CI [1.47-14,5], p<0.01), male gender (OR 0.68, 95% CI [0.46-1.0], p<0.05), mechanical ventilation (OR 1.87, 95% CI [1.19-2.95], p<0.01), hemodialysis (OR 1.98, 95% CI [1.05-3.75], p<0.03), and the SAPS II score (OR 1.08, 95% CI [1.06-1.10], p<0.001). CONCLUSION: The present study revealed a higher prevalence of infections in Brazilian ICUs than has been previously reported. There was a clear association between infection and mortality.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)