Abstract
Rev Bras Ter Intensiva. 2016;28(2):179-189
DOI 10.5935/0103-507X.20160019
Lower respiratory tract infections are common and potentially lethal conditions and are a major cause of inadequate antibiotic prescriptions. Characterization of disease severity and prognostic prediction in affected patients can aid disease management and can increase accuracy in determining the need for and place of hospitalization. The inclusion of biomarkers, particularly procalcitonin, in the decision taken process is a promising strategy. This study aims to present a narrative review of the potential applications and limitations of procalcitonin as a prognostic marker in hospitalized patients with lower respiratory tract infections. The studies on this topic are heterogeneous with respect to procalcitonin measurement techniques, cutoff values, clinical settings, and disease severity. The results show that procalcitonin delivers moderate performance for prognostic prediction in patients with lower respiratory tract infections; its predictive performance was not higher than that of classical methods, and knowledge of procalcitonin levels is most useful when interpreted together with other clinical and laboratory results. Overall, repeated measurement of the procalcitonin levels during the first days of treatment provides more prognostic information than a single measurement; however, information on the cost-effectiveness of this procedure in intensive care patients is lacking. The results of studies that evaluated the prognostic value of initial procalcitonin levels in patients with community-acquired pneumonia are more consistent and have greater potential for practical application; in this case, low procalcitonin levels identify those patients with a low risk of adverse outcomes.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):58-63
DOI 10.1590/S0103-507X2012000100009
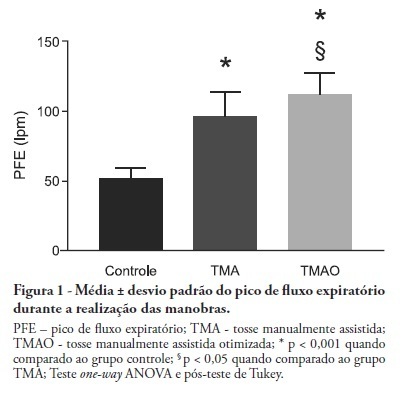
OBJECTIVE: Mechanical ventilation is associated with retained airway secretions. Manually assisted cough contributes to the displacement of bronchial mucus, whereas positive end-expiratory pressure increases collateral ventilation and maintains airway patency. This study aimed to assess the effects of manually assisted cough, either alone or added to increased positive end-expiratory pressure and inspiratory time (optimized manually assisted cough), on the expiratory peak flow and respiratory system mechanics in mechanically ventilated patients. METHODS: In this controlled and randomized clinical trial, respiratory mechanics and expiratory peak flow were assessed in male and female patients undergoing either tracheal suctioning alone, manually assisted cough followed by tracheal suctioning or optimized manually assisted cough followed by tracheal suctioning. RESULTS: Thirty-five patients completed the trial. Respiratory system resistance was significantly reduced after optimized manually assisted cough (16.0 ± 3.6 versus 12.4 ± 3.1 cmH2O/L/s; p = 0.04). The expiratory peak flow during optimized manually assisted cough was significantly higher in comparison with the values observed during manually assisted cough (112.3 ± 15.6 versus 95.8 ± 18.3 Lpm; p < 0.05). Both values were significantly higher than the values observed in the group undergoing tracheal suctioning alone (52.0 ± 7.6 Lpm; p < 0.001). CONCLUSION: Optimized manually assisted cough increases the expiratory peak flow in comparison with manually assisted cough; in addition, this procedure reduces respiratory system resistance.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)