Abstract
Rev Bras Ter Intensiva. 2022;34(1):176-184
DOI 10.5935/0103-507X.20220012-en
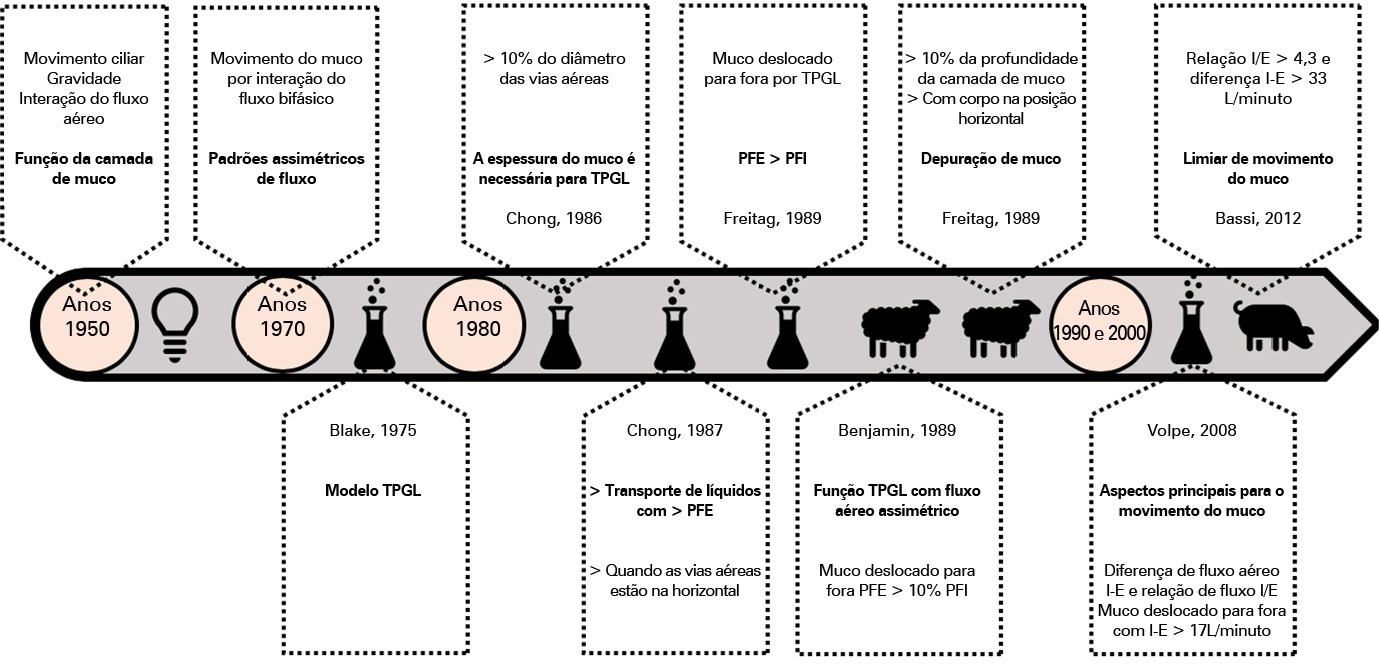
Defective management of secretions is one of the most frequent complications in invasive mechanically ventilated patients. Clearance of secretions through chest physiotherapy is a critical aspect of the treatment of these patients. Manual rib cage compression is one of the most practiced chest physiotherapy techniques in ventilated patients; however, its impact on clinical outcomes remains controversial due to methodological issues and poor understanding of its action. In this review, we present a detailed analysis of the physical principles involved in rib cage compression technique performance, as well as the physiological effects observed in experimental and clinical studies, which show that the use of brief and vigorous rib cage compression, based on increased expiratory flows (expiratory-inspiratory airflow difference of > 33L/minute), can improve mucus movement toward the glottis. On the other hand, the use of soft and gradual rib cage compression throughout the whole expiratory phase does not impact the expiratory flows, resulting in ineffective or undesired effects in some cases. More physiological studies are needed to understand the principles of the rib cage compression technique in ventilated humans. However, according to the evidence, rib cage compression has more potential benefits than risks, so its implementation should be promoted.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):616-623
DOI 10.5935/0103-507X.20210071
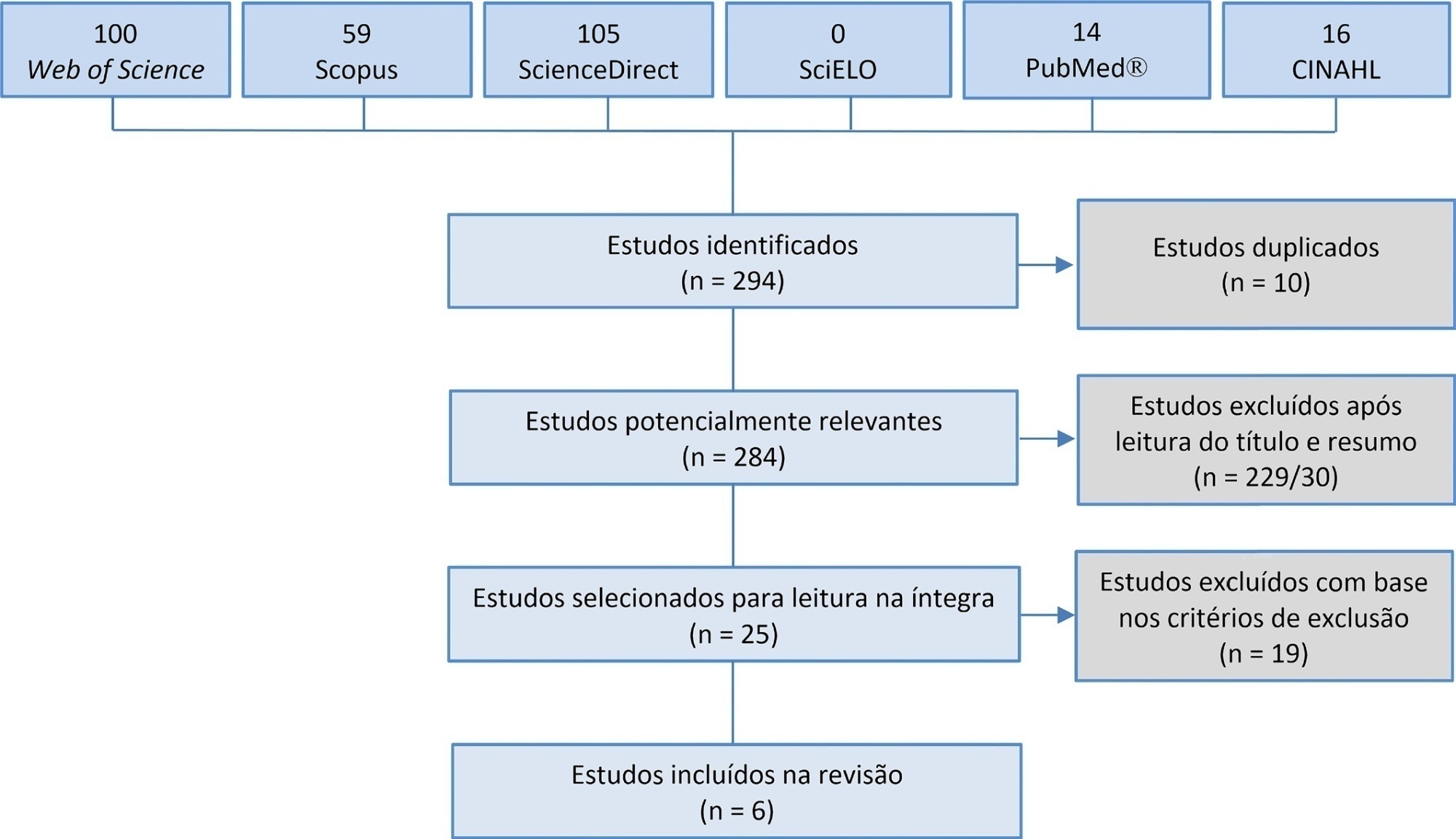
Manual hyperinflation is used in neonatal and pediatric intensive care units to promote expiratory flow bias, but there is no consensus on the benefits of the technique. Thus, a review that presents supporting evidence is necessary. This study aims to review the literature on the manual hyperinflation maneuver in neonatal and pediatric intensive care units to analyze the evidence for this technique in terms of the forms of application (associated with other techniques or not), its safety, the performance of manual resuscitators and the influence of the physical therapist’s experience, in addition to evaluating the methodological quality of the identified articles. A search was performed in the following databases: Web of Science, ScienceDirect, PubMedⓇ, Scopus, CINAHL and SciELO. Two researchers independently selected the articles. Duplicate studies were assessed, evaluated by title and abstract and then read in full. The quality of the articles was analyzed using the PEDro scale. Six articles were included, two of which had high methodological quality. The main results provided information on the contribution of the positive end-expiratory pressure valve to increasing lung volumes and the use of chest compressions to optimize expiratory flow bias, the negative influence of operator experience on the increase in peak inspiratory flow, the performance of different manual resuscitators when used with the technique and the safety of application in terms of maintaining hemodynamic stability and increasing peripheral oxygen saturation. The available studies point to a positive effect of the manual hyperinflation maneuver in children who are admitted to intensive care units.
Registration PROSPERO: CRD42018108056.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):445-456
DOI 10.5935/0103-507X.20210060
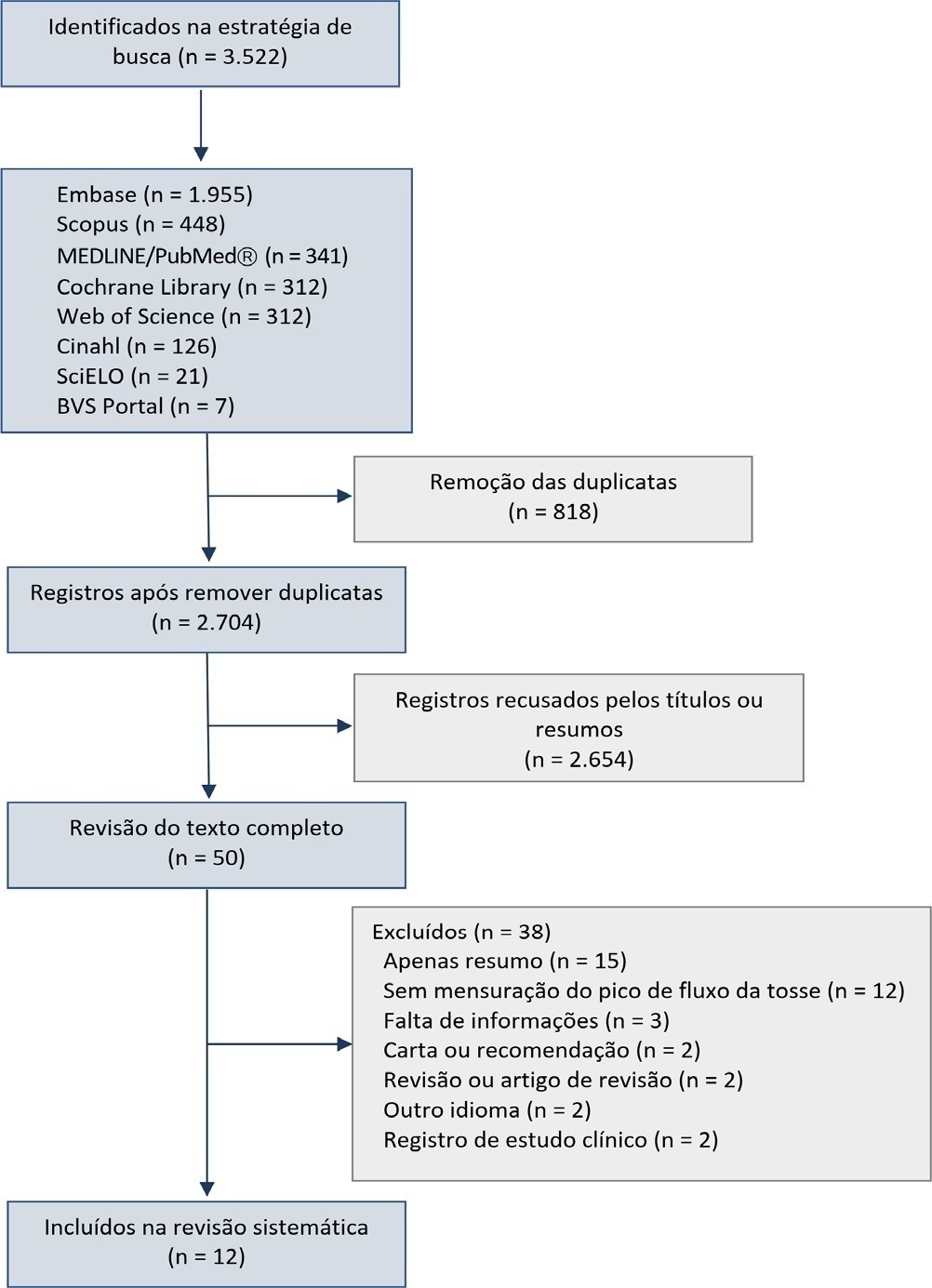
This systematic review was designed to assess the usefulness of cough peak flow to predict the extubation outcome in subjects who passed a spontaneous breathing trial.
The search covered the scientific databases MEDLINE, Lilacs, Ibecs, Cinahl, SciELO, Cochrane, Scopus, Web of Science and gray literature. The Quality Assessment of Diagnostic Accuracy Studies was used to assess the methodological quality and risk of study bias. The statistical heterogeneity of the likelihood (LR) and diagnostic odds ratios were evaluated using forest plots and Cochran’s Q statistic, and a crosshair summary Receiver Operating Characteristic plot using the multiple cutoffs model was calculated.
We initially retrieved 3,522 references from the databases; among these, 12 studies including 1,757 subjects were selected for the qualitative analysis. Many studies presented an unclear risk of bias in the “patient selection” and “flow and time” criteria. Among the 12 included studies, seven presented “high risk” and five “unclear risk” for the item “reference standard.” The diagnostic performance of the cough peak flow for the extubation outcome was low to moderate when we considered the results from all included studies, with a +LR of 1.360 (95%CI 1.240 - 1.530), -LR of 0.218 (95%CI 0.159 - 0.293) and a diagnostic odds ratio of 6.450 (95%CI 4.490 - 9.090). A subgroup analysis including only the studies with a cutoff between 55 and 65 L/minute showed a slightly better, although still moderate, performance.
A cough peak flow assessment considering a cutoff between 55 and 65L/minute may be useful as a complementary measurement prior to extubation. Additional well-designed studies are necessary to identify the best method and equipment to record the cough peak flow as well as the best cutoff.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):14-22
DOI 10.5935/0103-507X.20170004
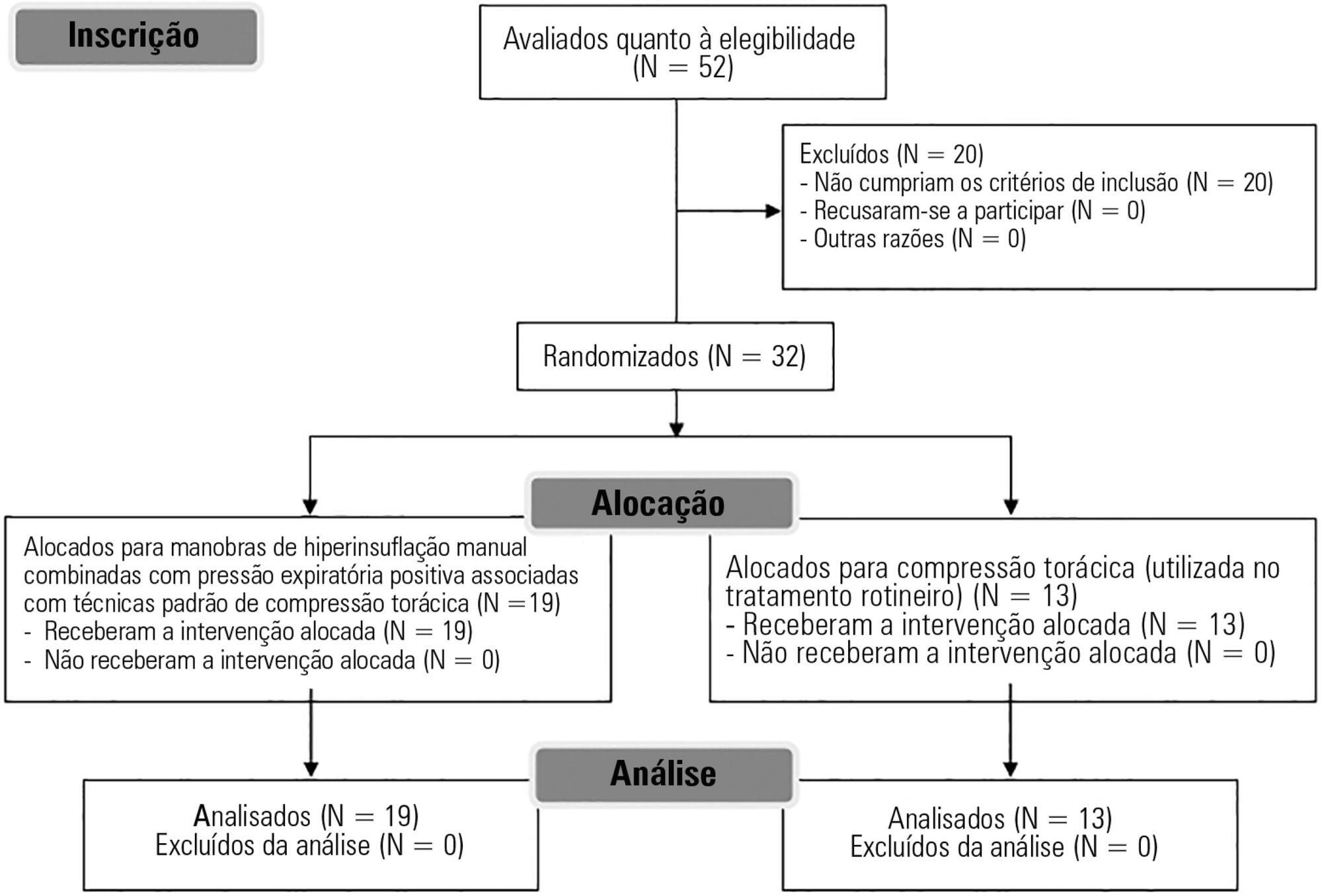
To evaluate the effects of bag-valve breathing maneuvers combined with standard manual chest compression techniques on safety, hemodynamics and oxygenation in stable septic shock patients.
A parallel, assessor-blinded, randomized trial of two groups. A computer-generated list of random numbers was prepared by an independent researcher to allocate treatments.
The Intensive Care Unit at Hospital São Lucas, Pontifícia Universidade Católica do Rio Grande do Sul.
Fifty-two subjects were assessed for eligibility, and 32 were included. All included subjects (n = 32) received the allocated intervention (n = 19 for the Experimental Group and n = 13 for the Control Group).
Twenty minutes of bag-valve breathing maneuvers combined with manual chest compression techniques (Experimental Group) or chest compression, as routinely used at our intensive care unit (Control Group). Follow-up was performed immediately after and at 30 minutes after the intervention.
Mean artery pressure.
All included subjects completed the trial (N = 32). We found no relevant effects on mean artery pressure (p = 0.17), heart rate (p = 0.50) or mean pulmonary artery pressure (p = 0.89) after adjusting for subject age and weight. Both groups were identical regarding oxygen consumption after the data adjustment (p = 0.84). Peripheral oxygen saturation tended to increase over time in both groups (p = 0.05), and there was no significant association between cardiac output and venous oxygen saturation (p = 0.813). No clinical deterioration was observed.
A single session of bag-valve breathing maneuvers combined with manual chest compression is hemodynamically safe for stable septic-shocked subjects over the short-term.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):96-104
DOI 10.5935/0103-507X.20170014
To review the literature on the effects of expiratory rib cage compression on ventilatory mechanics, airway clearance, and oxygen and hemodynamic indices in mechanically ventilated adults.
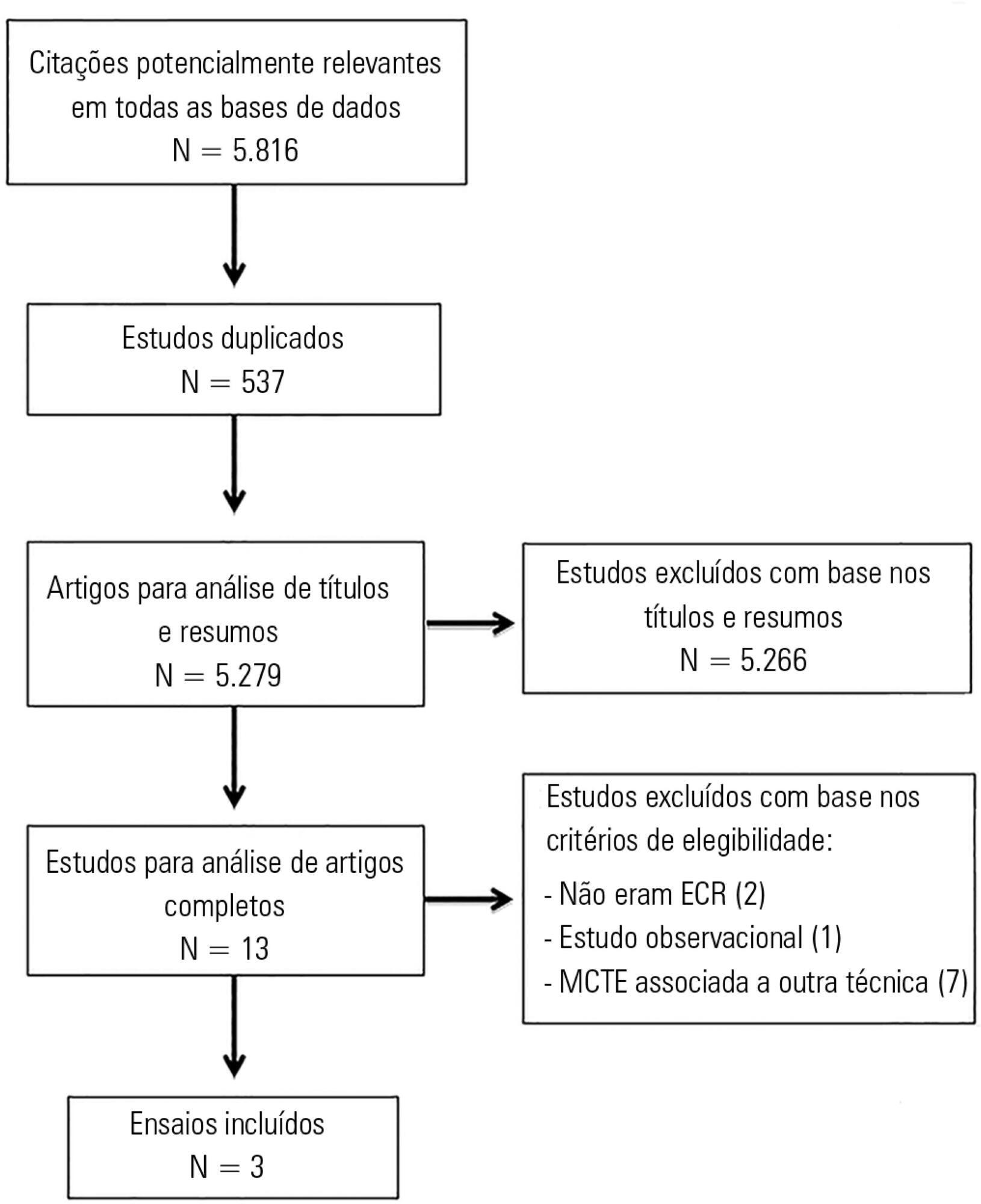
Systematic review with meta-analysis of randomized clinical trials in the databases MEDLINE (via PubMed), EMBASE, Cochrane CENTRAL, PEDro, and LILACS. Studies on adult patients hospitalized in intensive care units and under mechanical ventilation that analyzed the effects of expiratory rib cage compression with respect to a control group (without expiratory rib cage compression) and evaluated the outcomes static and dynamic compliance, sputum volume, systolic blood pressure, diastolic blood pressure, mean arterial pressure, heart rate, peripheral oxygen saturation, and ratio of arterial oxygen partial pressure to fraction of inspired oxygen were included. Experimental studies with animals and those with incomplete data were excluded.
The search strategy produced 5,816 studies, of which only three randomized crossover trials were included, totaling 93 patients. With respect to the outcome of heart rate, values were reduced in the expiratory rib cage compression group compared with the control group [-2.81 bpm (95% confidence interval [95%CI]: -4.73 to 0.89; I2: 0%)]. Regarding dynamic compliance, there was no significant difference between groups [-0.58mL/cmH2O (95%CI: -2.98 to 1.82; I2: 1%)]. Regarding the variables systolic blood pressure and diastolic blood pressure, significant differences were found after descriptive evaluation. However, there was no difference between groups regarding the variables secretion volume, static compliance, ratio of arterial oxygen partial pressure to fraction of inspired oxygen, and peripheral oxygen saturation.
There is a lack of evidence to support the use of expiratory rib cage compression in routine care, given that the literature on this topic offers low methodological quality and is inconclusive.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):341-347
DOI 10.5935/0103-507X.20160058
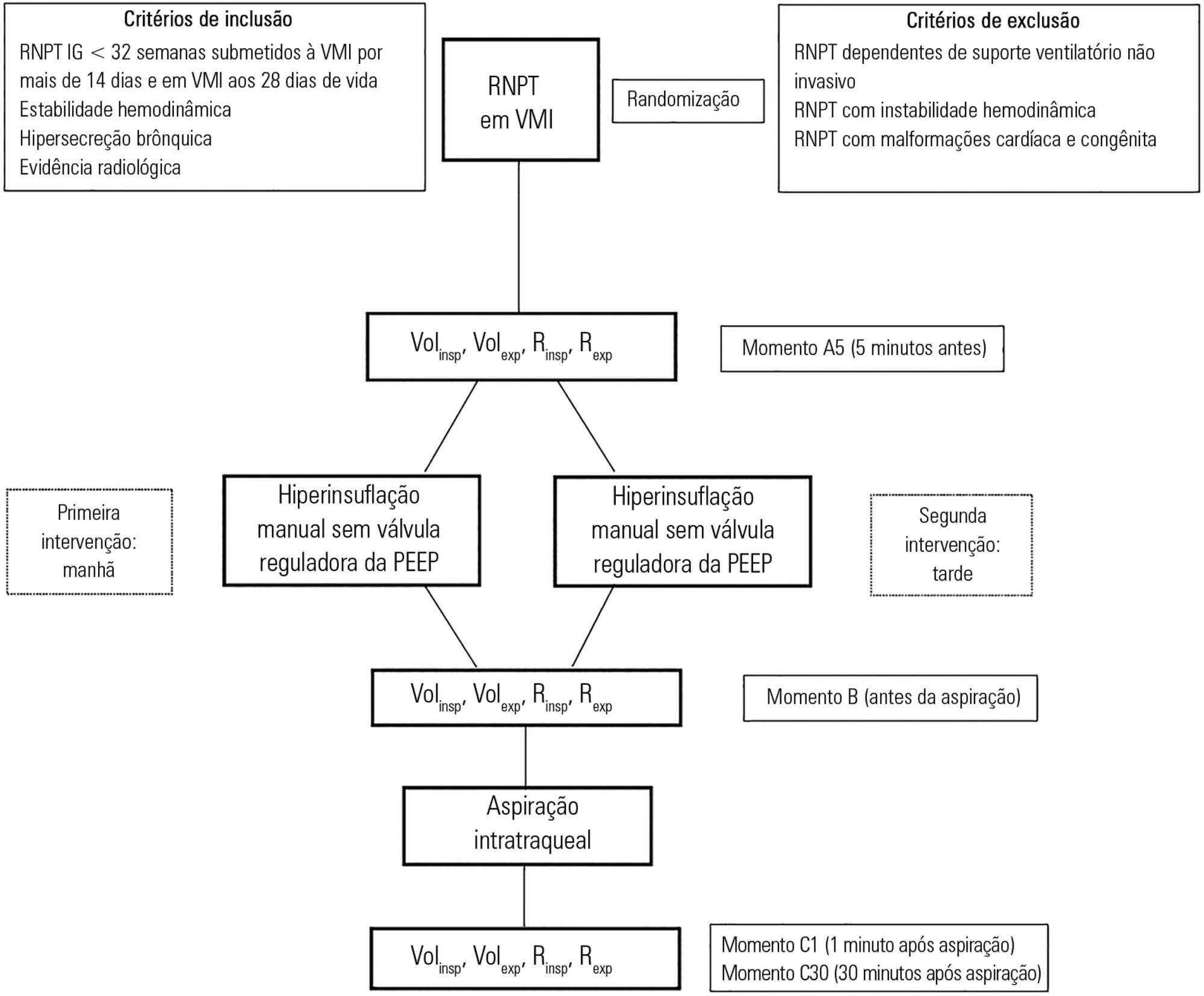
To assess the effects of manual hyperinflation, performed with a manual resuscitator with and without the positive end-expiratory pressure valve, on the respiratory function of preterm newborns under mechanical ventilation.
Cross-sectional study of hemodynamically stable preterm newborns with gestational age of less than 32 weeks, under mechanical ventilation and dependent on it at 28 days of life. Manual hyperinflation was applied randomly, alternating the use or not of the positive end-expiratory pressure valve, followed by tracheal aspiration for ending the maneuver. For nominal data, the two-tailed Wilcoxon test was applied at the 5% significance level and 80% power.
Twenty-eight preterm newborns, with an average birth weight of 1,005.71 ± 372.16g, an average gestational age of 28.90 ± 1.79 weeks, an average corrected age of 33.26 ± 1.78 weeks, and an average mechanical ventilation time of 29.5 (15 - 53) days, were studied. Increases in inspiratory and expiratory volumes occurred between time-points A5 (before the maneuver) and C1 (immediately after tracheal aspiration) in both the maneuver with the valve (p = 0.001 and p = 0.009) and without the valve (p = 0.026 and p = 0.001), respectively. There was also an increase in expiratory resistance between time-points A5 and C1 (p = 0.044).
Lung volumes increased when performing the maneuver with and without the valve, with a significant difference in the first minute after aspiration. There was a significant difference in expiratory resistance between the time-points A5 (before the maneuver) and C1 (immediately after tracheal aspiration) in the first minute after aspiration within each maneuver.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):155-160
DOI 10.5935/0103-507X.20150027
To evaluate the changes in ventilatory mechanics and hemodynamics that occur in patients dependent on mechanical ventilation who are subjected to a standard respiratory therapy protocol.
This experimental and prospective study was performed in two intensive care units, in which patients dependent on mechanical ventilation for more than 48 hours were consecutively enrolled and subjected to an established respiratory physiotherapy protocol. Ventilatory variables (dynamic lung compliance, respiratory system resistance, tidal volume, peak inspiratory pressure, respiratory rate, and oxygen saturation) and hemodynamic variables (heart rate) were measured one hour before (T-1), immediately after (T0) and one hour after (T+1) applying the respiratory physiotherapy protocol.
During the period of data collection, 104 patients were included in the study. Regarding the ventilatory variables, an increase in dynamic lung compliance (T-1 = 52.3 ± 16.1mL/cmH2O versus T0 = 65.1 ± 19.1mL/cmH2O; p < 0.001), tidal volume (T-1 = 550 ± 134mL versus T0 = 698 ± 155mL; p < 0.001), and peripheral oxygen saturation (T-1 = 96.5 ± 2.29% versus T0 = 98.2 ± 1.62%; p < 0.001) were observed, in addition to a reduction of respiratory system resistance (T-1 = 14.2 ± 4.63cmH2O/L/s versus T0 = 11.0 ± 3.43cmH2O/L/s; p < 0.001), after applying the respiratory physiotherapy protocol. All changes were present in the assessment performed one hour (T+1) after the application of the respiratory physiotherapy protocol. Regarding the hemodynamic variables, an immediate increase in the heart rate after application of the protocol was observed, but that increase was not maintained (T-1 = 88.9 ± 18.7 bpm versus T0 = 93.7 ± 19.2bpm versus T+1 = 88.5 ± 17.1bpm; p < 0.001).
Respiratory therapy leads to immediate changes in the lung mechanics and hemodynamics of mechanical ventilation-dependent patients, and ventilatory changes are likely to remain for at least one hour.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):7-13
DOI 10.5935/0103-507X.20140002
To evaluate the role of quality indicators and adverse events registering in the quality assessment of intensive care physiotherapy and to evaluate the impact of implementing protocolized care and professional training in the quality improvement process.
A prospective before-after study was designed to assess 15 indicators of the quality of care. Baseline compliance and adverse events were collected before and after the implementation of treatment protocols and staff training.
Eighty-nine patients admitted, being 48 in the pre-intervention period and 41 in the post-intervention period with a total of 1246 and 1191 observations respectively. Among the indicators related to the global population, there was a significant improvement in chest x-ray control, multidisciplinary rounds and shift changes as well as in compliance with these decisions. Indicators related to the population under mechanical ventilation, obtained by direct observation at bedside, showed a significant improvement in the compliance with the tidal volume of 6-8mL/Kg, plateau pressure <30cmH2O, adequate mechanical ventilation alarm setting, mechanical ventilation humidification control, adequate humidification line exchange and orotracheal tube position. Among the mechanical ventilation indicators collected through the physiotherapy records, there was significantly improved compliance with the predicted tidal volume registry and cuff pressure registry. There was a significant reduction in the number of adverse events. There was no impact on intensive care unit mortality, length of stay, duration of mechanical ventilation and ventilator-free days.
It is possible to measure the quality of physiotherapy care using indicators of quality control. The implementation of care protocols and training of the professionals can improve team performance.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)