Abstract
Crit Care Sci. 2023;35(3):320-327
DOI 10.5935/2965-2774.20230165-pt
To translate and cross-culturally adapt the Cornell Assessment of Pediatric Delirium anchor points from English to Brazilian Portuguese.
For the translation and cross-cultural adaptation of the anchor points, all steps recommended internationally were followed after authorization for use by the lead author. The stages were as follows: translation of the original version into Portuguese by two bilingual translators who were native speakers of the target language, synthesis of the versions, reverse translation by two translators who were native speakers of the source language, review and synthesis of the back-translation, review by a committee of experts and preparation of the final version.
The translation and cross-cultural adaptation of the anchor points was conducted in accordance with recommendations. The linguistic and semantic issues that arose were discussed by a committee of judges, with 91.8% agreement, as determined using a Likert scale, after changes by consensus. After reanalysis by the authors, there were no changes, resulting in the final version, which was easy to understand and administer.
The translation and cross-cultural adaptation of the anchor points of the Cornell Assessment of Pediatric Delirium scale into Portuguese spoken in Brazil were successful, maintaining the linguistic and semantic properties of the original instrument. The table of anchor points is easy to understand and will be helpful during the assessment of children younger than 24 months using the Cornell Assessment of Pediatric Delirium scale.
Abstract
Crit Care Sci. 2023;35(3):266-272
DOI 10.5935/2965-2774.20230223-pt
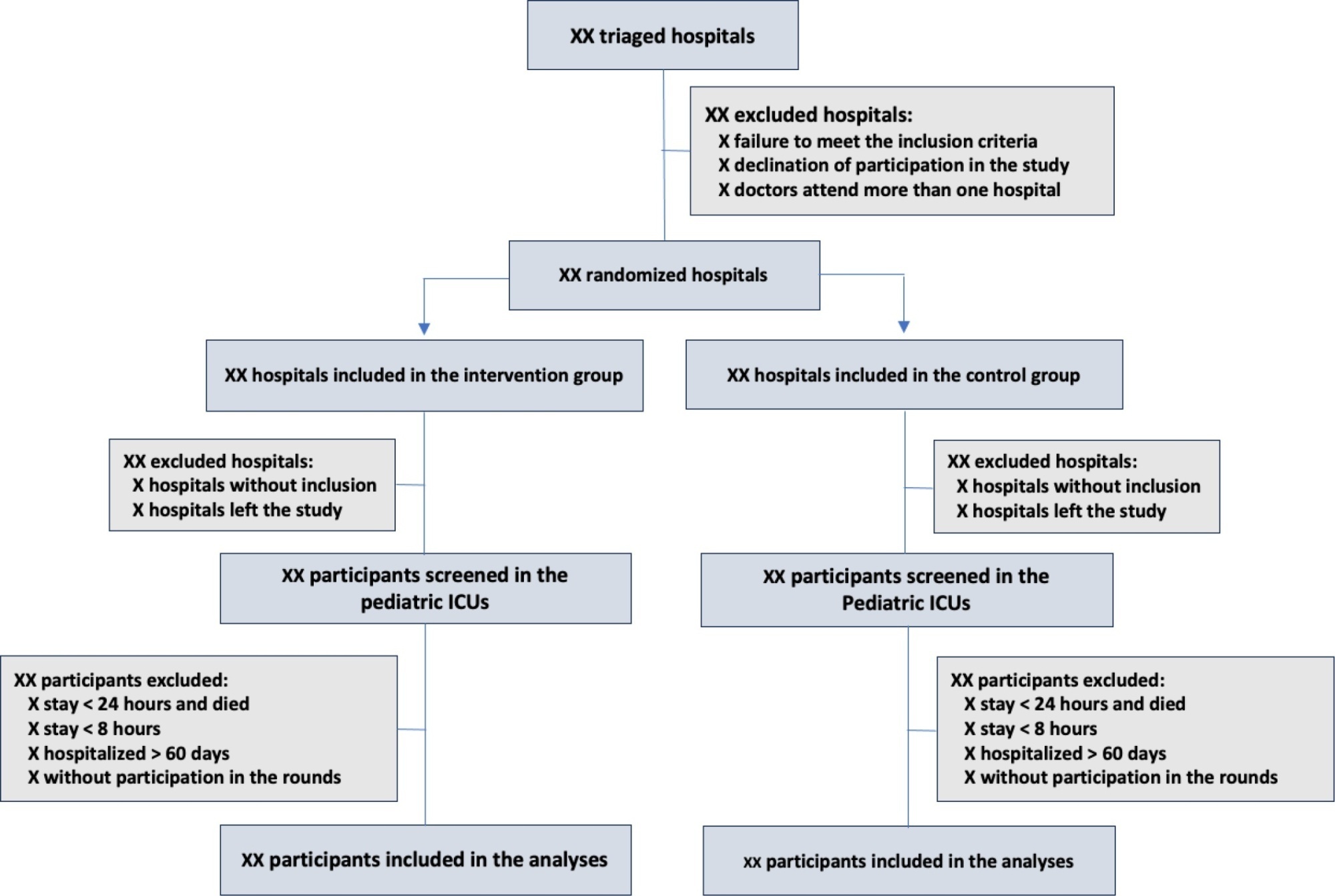
The objective of this study is to present the protocol of a cluster randomized clinical trial to be conducted through the TeleICU project - Qualification of Intensive Care by Telemedicine. The study will consist of a cluster randomized clinical trial, open label, in pediatric intensive care units, with an allocation ratio of 1:1, to compare the intervention group (support of Telemedicine for patients admitted to the pediatric intensive care unit) with a control group (pediatric intensive care unit usual care). The study proposed to select 16 pediatric intensive care units, including 100 participants per site, with a total of 1,600 participants. The intervention group will receive telerounds from Monday to Friday and will have specialists and continuing education activities available. The primary outcome measure will be the length of stay in the pediatric intensive care unit, defined as the difference between the date of discharge of the participant and the date of admission to the intensive care unit. The secondary outcomes will be mortality rate, invasive mechanical ventilation-free days, days using antibiotics, days using vasoactive drugs and days using sedoanalgesia. This study will be conducted in accordance with Resolution 466/12 of the National Health Council, with approval by the Research Ethics Committee of the institutions involved. The present study has the potential to reproduce studies on Telemedicine in intensive care and may make important contributions to care in intensive care units in Brazil and other settings. If Telemedicine shows positive clinical care results compared to conventional treatment, more pediatric patients may benefit.
ClinicalTrials.gov registry: NCT05260710
Abstract
Crit Care Sci. 2023;35(3):290-301
DOI 10.5935/2965-2774.20230388-pt
To determine the prevalence and factors associated with the physical rehabilitation of critically ill children in Brazilian pediatric intensive care units.
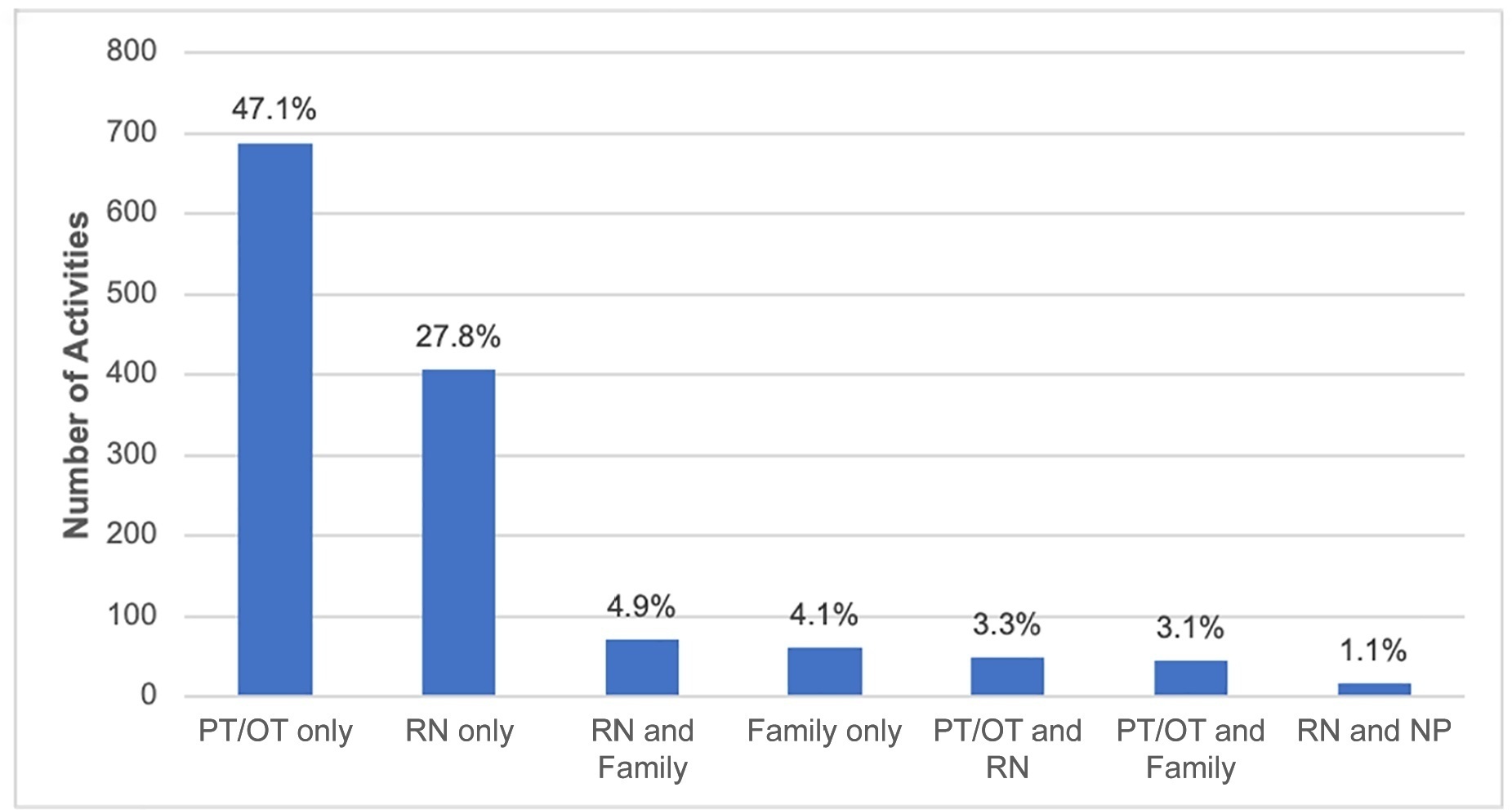
A 2-day, cross-sectional, multicenter point prevalence study comprising 27 pediatric intensive care units (out of 738) was conducted in Brazil in April and June 2019. This Brazilian study was part of a large multinational study called Prevalence of Acute Rehabilitation for Kids in the PICU (PARK-PICU). The primary outcome was the prevalence of mobility provided by physical therapy or occupational therapy. Clinical data on patient mobility, potential mobility safety events, and mobilization barriers were prospectively collected in patients admitted for ≥ 72 hours.
Children under the age of 3 years comprised 68% of the patient population. The prevalence of therapist-provided mobility was 74%, or 277 out of the 375 patient-days. Out-of-bed mobility was most positively associated with family presence (adjusted odds ratios 3.31;95%CI 1.70 - 6.43) and most negatively associated with arterial lines (adjusted odds ratios 0.16; 95%CI 0.05 - 0.57). Barriers to mobilization were reported on 27% of patient-days, the most common being lack of physician order (n = 18). Potential safety events occurred in 3% of all mobilization events.
Therapist-provided mobility in Brazilian pediatric intensive care units is frequent. Family presence was high and positively associated with out-of-bed mobility. The presence of physiotherapists 24 hours a day in Brazilian pediatric intensive care units may have a substantial impact on the mobilization of critically ill children.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):469-476
DOI 10.5935/0103-507X.20220429-en
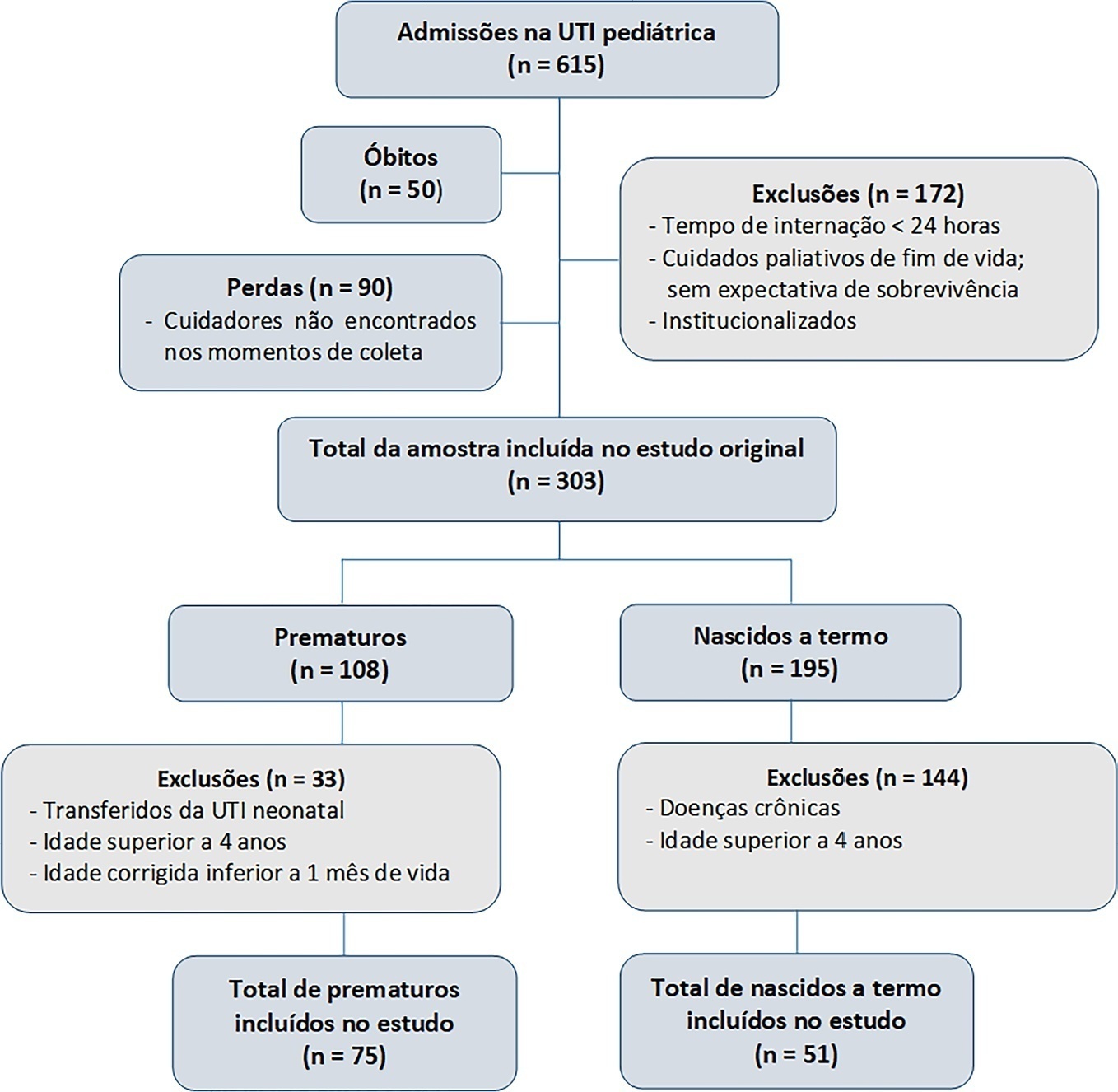
To evaluate the effects of critical illness on the functional status of children aged zero to 4 years with or without a history of prematurity after discharge from the pediatric intensive care unit.
This was a secondary cross-sectional study nested in an observational cohort of survivors from a pediatric intensive care unit. Functional assessment was performed using the Functional Status Scale within 48 hours after discharge from the pediatric intensive care unit.
A total of 126 patients participated in the study, 75 of whom were premature, and 51 of whom were born at term. Comparing the baseline and functional status at pediatric intensive care unit discharge, both groups showed significant differences (p < 0.001). Preterm patients exhibited greater functional decline at discharge from the pediatric intensive care unit (61%). Among patients born at term, there was a significant correlation between the Pediatric Index of Mortality, duration of sedation, duration of mechanical ventilation and length of hospital stay with the functional outcomes (p = 0.05).
Most patients showed a functional decline at discharge from the pediatric intensive care unit. Although preterm patients had a greater functional decline at discharge, sedation and mechanical ventilation duration influenced functional status among patients born at term.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):507-518
DOI 10.5935/0103-507X.20220145-en
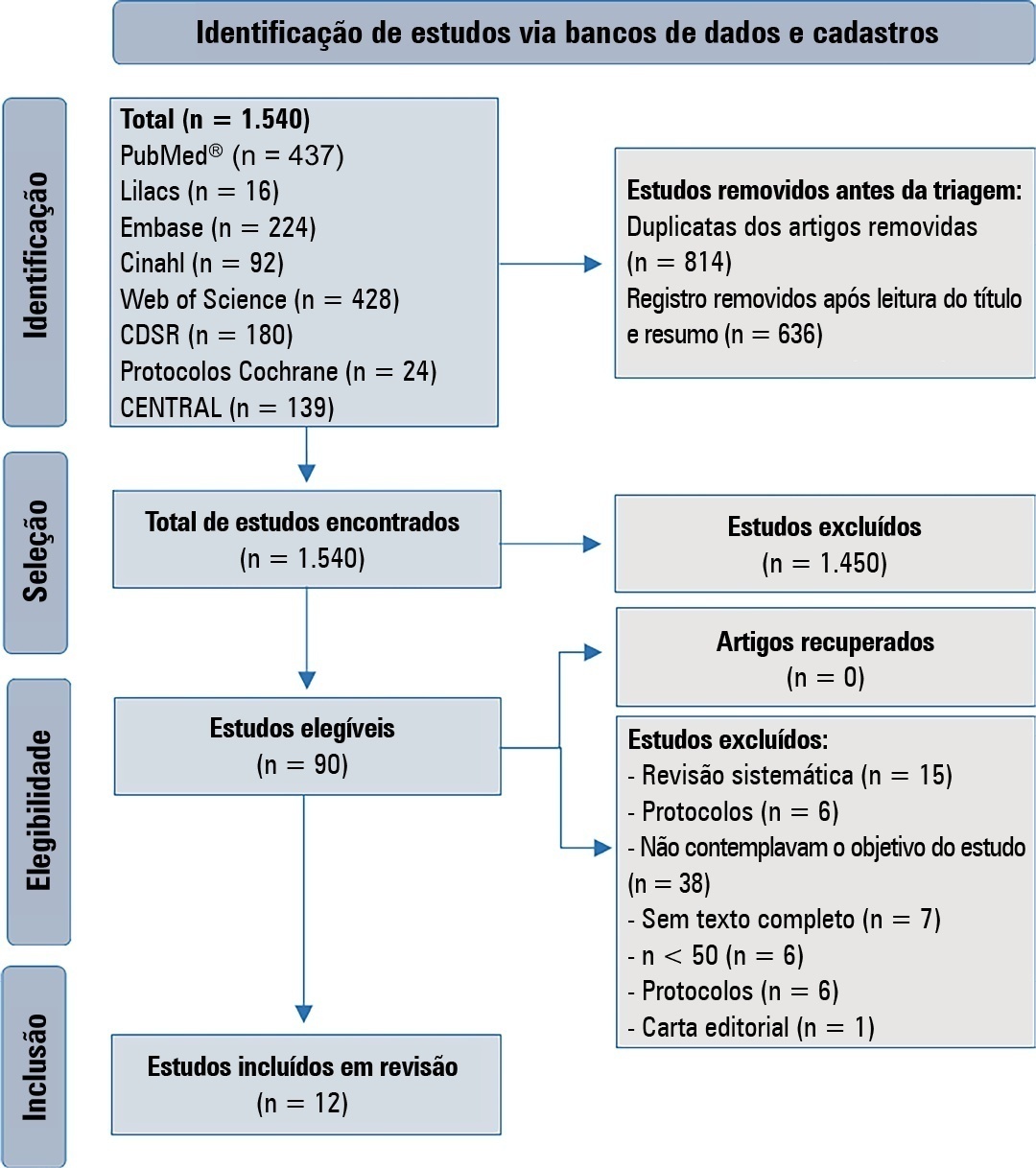
To verify strategies for the prevention and treatment of abstinence syndrome in a pediatric intensive care unit.
This is a systematic review in the PubMed database®, Lilacs, Embase, Web of Science, Cochrane, Cinahl, Cochrane Database Systematic Review and CENTRAL. A three-step search strategy was used for this review, and the protocol was approved in PROSPERO (CRD42021274670).
Twelve articles were included in the analysis. There was great heterogeneity among the studies included, especially regarding the therapeutic regimens used for sedation and analgesia. Midazolam doses ranged from 0.05mg/kg/hour to 0.3mg/kg/hour. Morphine also varied considerably, from 10mcg/kg/hour to 30mcg/kg/hour, between studies. Among the 12 selected studies, the most commonly used scale for the identification of withdrawal symptoms was the Sophia Observational Withdrawal Symptoms Scale. In three studies, there was a statistically significant difference in the prevention and management of the withdrawal syndrome due to the implementation of different protocols (p < 0.01 and p < 0.001).
There was great variation in the sedoanalgesia regimen used by the studies and the method of weaning and evaluation of withdrawal syndrome. More studies are needed to provide more robust evidence about the most appropriate treatment for the prevention and reduction of withdrawal signs and symptoms in critically ill children.
CRD 42021274670
Abstract
Rev Bras Ter Intensiva. 2022;34(2):295-299
DOI 10.5935/0103-507X.20220028-en
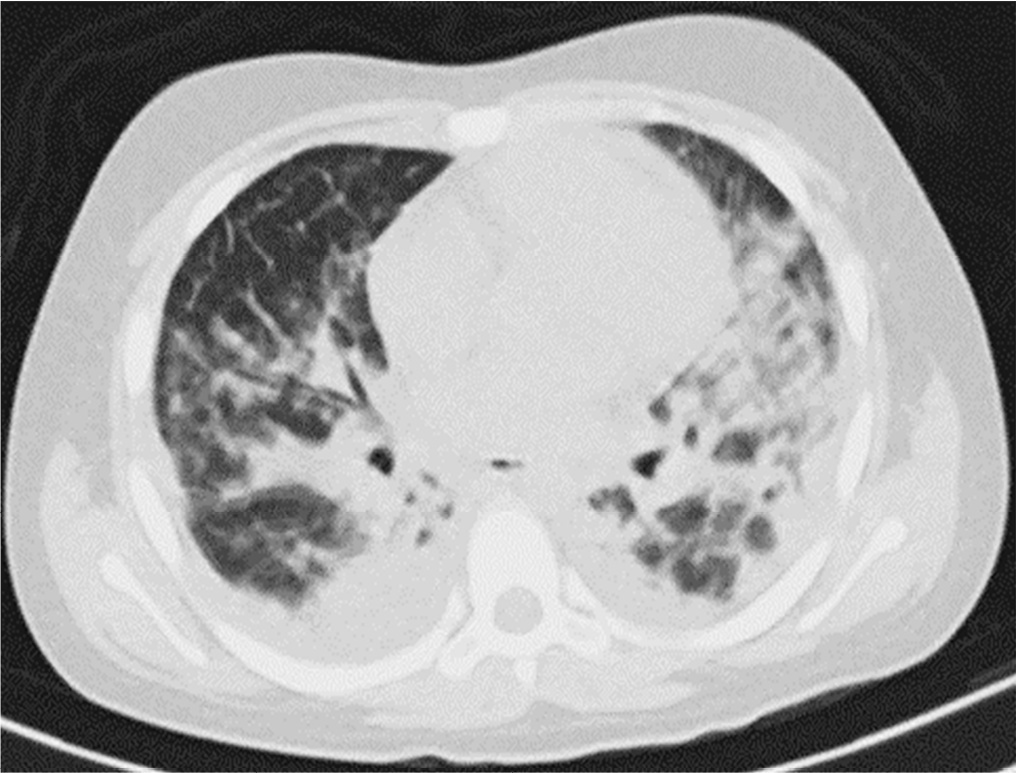
Posterior reversible encephalopathy syndrome is a rare clinical and radiological syndrome characterized by vasogenic edema of the white matter of the occipital and parietal lobes, which are usually symmetrical, resulting from a secondary manifestation of acute dysfunction of the posterior cerebrovascular system. We describe a case of posterior reversible encephalopathy syndrome secondary to SARS-CoV-2 infection in a 9-year-old boy who developed acute hypoxemic respiratory failure and required assisted mechanical ventilation. The child developed multisystem inflammatory syndrome, and he was monitored in the pediatric intensive care unit and was provided mechanical ventilation and vasoactive agents for hemodynamic support. Additionally, he developed pulmonary and extrapulmonary clinical manifestations along with neuropsychiatric manifestations that required close follow-up and were verified using brain magnetic resonance imaging for timely intervention. Currently, there are few reports of children with posterior reversible encephalopathy syndrome associated with multisystem inflammatory syndrome.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):592-599
DOI 10.5935/0103-507X.20210086
To translate and culturally adapt the Pediatric Intensive Care Unit-Quality of Dying and Death questionnaire into Brazilian Portuguese.
This was a cross-cultural adaptation process including conceptual, cultural, and semantic equivalence steps comprising three stages. Stage 1 involved authorization to perform the translation and cultural adaptation. Stage 2 entailed independent translation from English into Brazilian Portuguese, a synthesis of the translation, back-translation, and an expert panel. Stage 3 involved a pretest conducted with family caregivers and a multidisciplinary team.
The evaluation by the expert panel resulted in an average agreement of 0.8 in relation to semantic, cultural, and conceptual equivalence. The pretests of both versions of the questionnaire showed that the participants had adequate comprehension regarding the ease of understanding the items and response options.
After going through the process of translation and cultural adaptation, the Pediatric Intensive Care Unit-Quality of Dying and Death caregiver and multidisciplinary team versions were considered culturally adapted, with both groups having a good understanding of the items. The questionnaires include relevant items to evaluate the process of death and dying in the intensive care setting, and suggest changes in care centered on patients and especially family caregivers, given the finitude of their children.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):616-623
DOI 10.5935/0103-507X.20210071
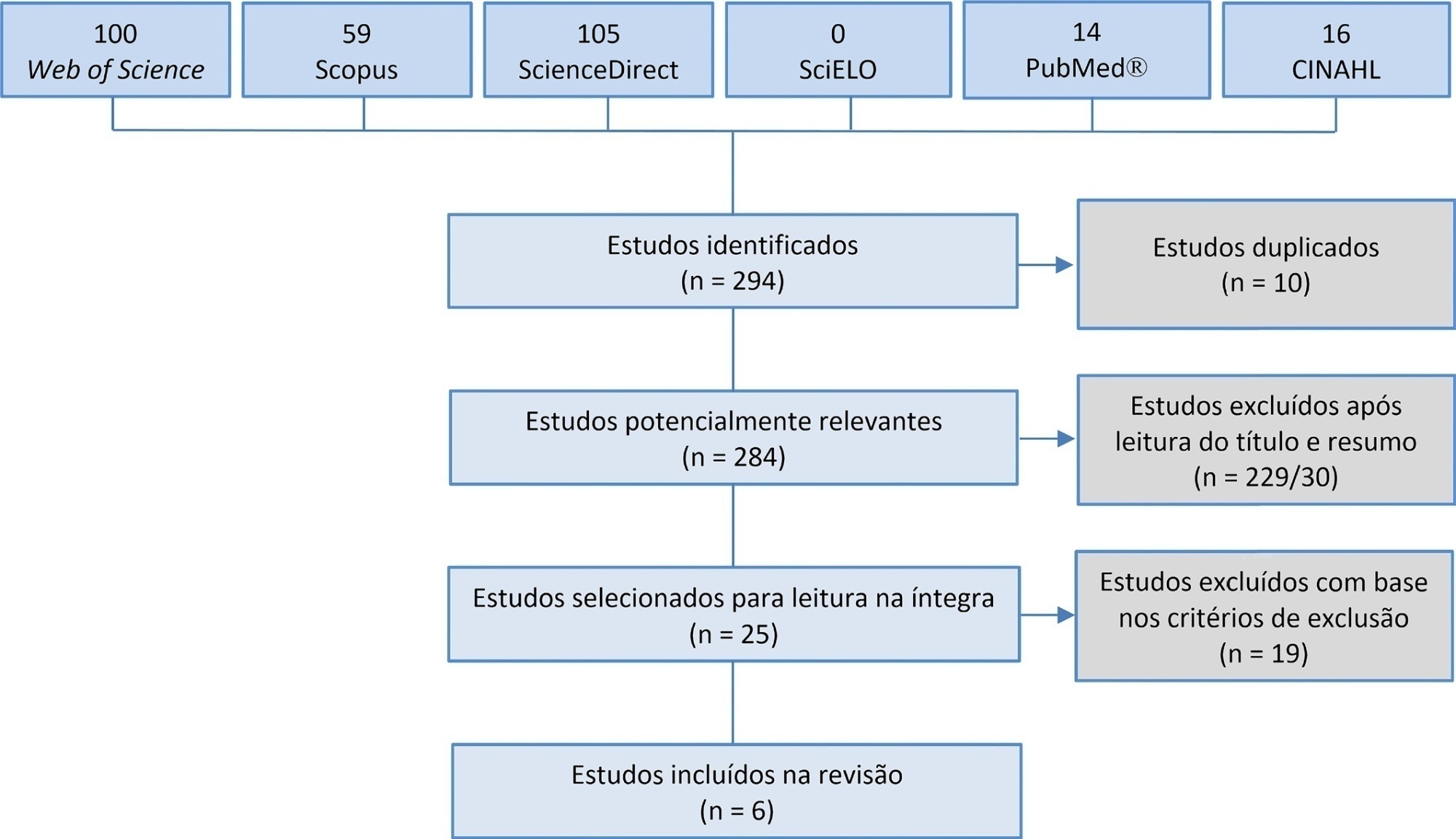
Manual hyperinflation is used in neonatal and pediatric intensive care units to promote expiratory flow bias, but there is no consensus on the benefits of the technique. Thus, a review that presents supporting evidence is necessary. This study aims to review the literature on the manual hyperinflation maneuver in neonatal and pediatric intensive care units to analyze the evidence for this technique in terms of the forms of application (associated with other techniques or not), its safety, the performance of manual resuscitators and the influence of the physical therapist’s experience, in addition to evaluating the methodological quality of the identified articles. A search was performed in the following databases: Web of Science, ScienceDirect, PubMedⓇ, Scopus, CINAHL and SciELO. Two researchers independently selected the articles. Duplicate studies were assessed, evaluated by title and abstract and then read in full. The quality of the articles was analyzed using the PEDro scale. Six articles were included, two of which had high methodological quality. The main results provided information on the contribution of the positive end-expiratory pressure valve to increasing lung volumes and the use of chest compressions to optimize expiratory flow bias, the negative influence of operator experience on the increase in peak inspiratory flow, the performance of different manual resuscitators when used with the technique and the safety of application in terms of maintaining hemodynamic stability and increasing peripheral oxygen saturation. The available studies point to a positive effect of the manual hyperinflation maneuver in children who are admitted to intensive care units.
Registration PROSPERO: CRD42018108056.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)