Abstract
Rev Bras Ter Intensiva. 2021;33(4):616-623
DOI 10.5935/0103-507X.20210071
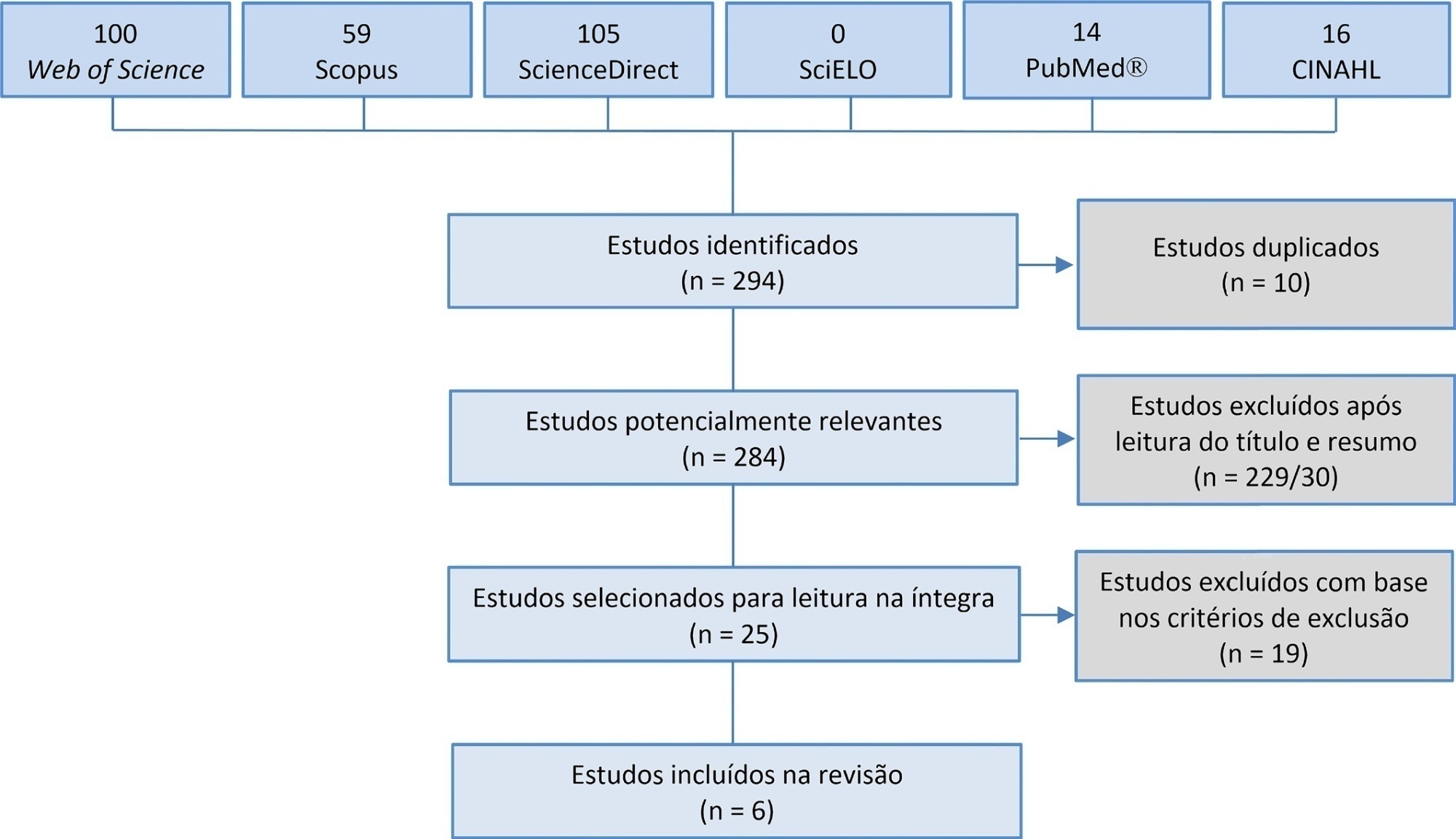
Manual hyperinflation is used in neonatal and pediatric intensive care units to promote expiratory flow bias, but there is no consensus on the benefits of the technique. Thus, a review that presents supporting evidence is necessary. This study aims to review the literature on the manual hyperinflation maneuver in neonatal and pediatric intensive care units to analyze the evidence for this technique in terms of the forms of application (associated with other techniques or not), its safety, the performance of manual resuscitators and the influence of the physical therapist’s experience, in addition to evaluating the methodological quality of the identified articles. A search was performed in the following databases: Web of Science, ScienceDirect, PubMedⓇ, Scopus, CINAHL and SciELO. Two researchers independently selected the articles. Duplicate studies were assessed, evaluated by title and abstract and then read in full. The quality of the articles was analyzed using the PEDro scale. Six articles were included, two of which had high methodological quality. The main results provided information on the contribution of the positive end-expiratory pressure valve to increasing lung volumes and the use of chest compressions to optimize expiratory flow bias, the negative influence of operator experience on the increase in peak inspiratory flow, the performance of different manual resuscitators when used with the technique and the safety of application in terms of maintaining hemodynamic stability and increasing peripheral oxygen saturation. The available studies point to a positive effect of the manual hyperinflation maneuver in children who are admitted to intensive care units.
Registration PROSPERO: CRD42018108056.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):235-243
DOI 10.5935/0103-507X.20200038
To identify the neonatal, pediatric and mixed (neonatal and pediatric) intensive care units in Brazil that use cuffed tracheal tubes in clinical practice and to describe the characteristics related to the use of protocols and monitoring.
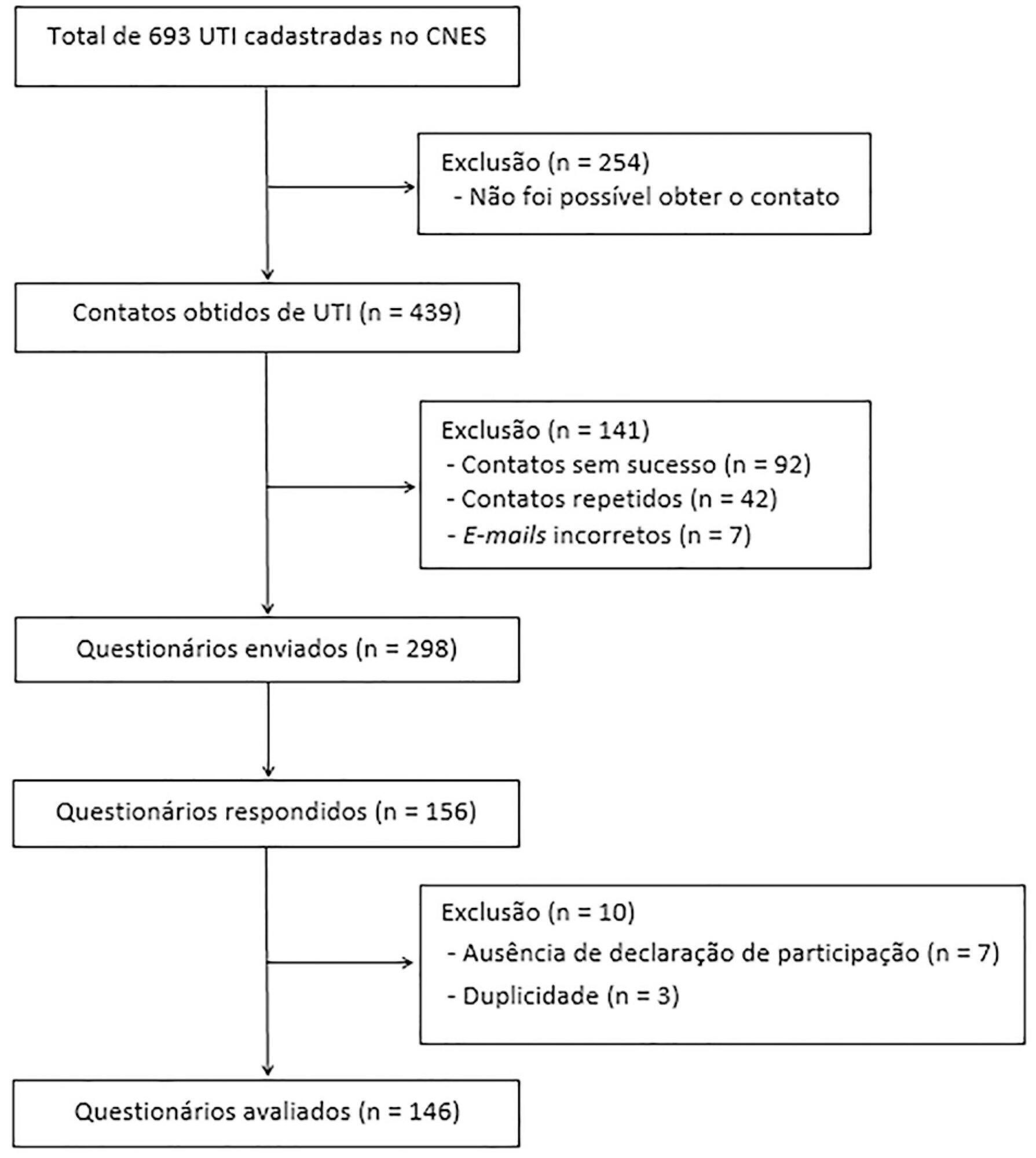
To identify the intensive care units in Brazil, the Ministry of Health’s National Registry of Health Facilities was accessed, and information was collected on 693 registered intensive care units. This was an analytical cross-sectional survey conducted through electronic questionnaires sent to 298 neonatal, pediatric and mixed intensive care units in Brazil.
This study analyzed 146 questionnaires (49.3% from neonatal intensive care units, 35.6% from pediatric intensive care units and 15.1% from mixed pediatric intensive care units). Most of the participating units (78/146) used cuffed tracheal tubes, with a predominance of use in pediatric intensive care units (52/78). Most of the units that used cuffed tracheal tubes applied a cuff pressure monitoring protocol (45/78). The use of cuff monitoring protocols was observed in intensive care units with a physical therapy service exclusive to the unit (38/61) and in those with a physical therapist present 24 hours/day (25/45). The most frequent cause of extubation failure related to the use of cuffed tracheal tubes in pediatric intensive care units was upper airway obstruction.
In this survey, the use of cuffed tracheal tubes and the application of a cuff pressure monitoring protocol was predominant in pediatric intensive care units. The use of a monitoring protocol was more common in intensive care units that had a physical therapist who was exclusive to the unit and was present 24 hours/day.
Abstract
Rev Bras Ter Intensiva. 2006;18(4):418-422
DOI 10.1590/S0103-507X2006000400017
BACKGROUND AND OBJECTIVES: Severe sepsis represents the systemic inflammatory response resulting from an infection, associated with one of the following: cardiovascular organ dysfunction, acute respiratory distress syndrome or two or more organ dysfunctions. Although the mortality rate from sepsis in children has steadily decreased in the last decades, the mortality rate in newborns remains high (20% to 40%) despite the development in intensive care. The authors describe a newborn who suffered from sepsis, shock and multiple organ dysfunction syndromes (MODS) that recovered after the administration of activated C protein. CASE REPORT: A premature newborn underwent cesarean section because of a premature rupture of membranes and acute fetal distress. The newborn developed acute respiratory distress due to intrauterine pneumonia and was taken to the Neonatal Intensive Care Unit. The patient was given mechanical ventilation, exogenous pulmonary surfactant and antibiotics early in the treatment. Nevertheless, he developed persistent pulmonary hypertension and shock. The control of the infection was difficult, despite the adjustment of the antibiotics, resulting in the development of MODS. On the 28th day, activated C protein was given to the patient. The administration of the drug was successful and the patient recovered from the organ dysfunction without bleeding. CONCLUSIONS: The activated C protein can't be recommended as a routine in the treatment of newborns with severe sepsis. However, in this case, it contributed to the recovery of the organ dysfunctions presented by the patient.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):322-326
DOI 10.1590/S0103-507X2007000300009
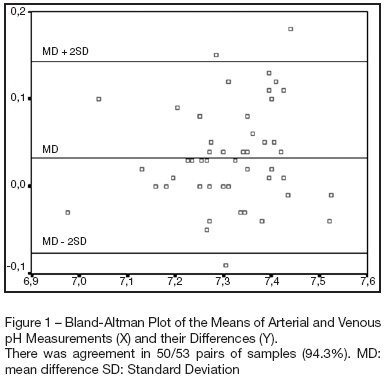
BACKGROUND AND OBJECTIVES: Determine the extent of agreement and correlation between arterial samples and venous (obtained from a venous umbilical catheter), with respect to measurements of pH, bicarbonate, base excess and lactate, in critically ill term and premature newborns. METHODS: Arterial blood samples (0.5-1 mL) were obtained for gas analysis by radial artery puncture, and, within the limit of 5 minutes, samples were obtained from venous umbilical catheters. Bland-Altman plots were used to depict agreement between arterial and venous measurements. Limits of agreement were defined as the mean difference ± 2SD (Standard Deviation). Correlation was assessed by Pearson's method. RESULTS: A hundred and six samples (53 pairs) were taken from 53 patients for analysis of bicarbonate, pH and base excess. Lactate was analyzed in 49 pairs of samples. Differences were within the limits of agreement in 94.3% of pairs of samples for pH, and the same percentage was observed for bicarbonate. There was agreement in 96.2% of pairs for base excess, and in 91.8% for lactate. Mean differences were 0.03 units for pH, -1.2 mmol/L for bicarbonate, -0.24 mmol/L for base excess and 0.33 mmol/L for lactate. Pearson's correlation coefficients (r) were 0.87 for pH, 0.76 for bicarbonate, 0.86 for base excess and 0.95 for lactate. CONCLUSIONS: Although single venous values cannot be used as equivalent to arterial for assessing acid base status in newborns, venous blood samples can be used serially for monitoring trends over time.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)