You searched for:"Cíntia Johnston"
We found (8) results for your search.-
Original Article
Performance and labor conditions of physiotherapists in Brazilian intensive care units during the COVID-19 pandemic. What did we learn?
Crit Care Sci. 2023;35(3):273-280
Abstract
Original ArticlePerformance and labor conditions of physiotherapists in Brazilian intensive care units during the COVID-19 pandemic. What did we learn?
Crit Care Sci. 2023;35(3):273-280
DOI 10.5935/2965-2774.20230359-pt
Views5ABSTRACT
Objective:
To describe the role of physiotherapists in assisting patients suspected to have or diagnosed with COVID-19 hospitalized in intensive care units in Brazil regarding technical training, working time, care practice, labor conditions and remuneration.
Methods:
An analytical cross-sectional survey was carried out through an electronic questionnaire distributed to physiotherapists who worked in the care of patients with COVID-19 in Brazilian intensive care units.
Results:
A total of 657 questionnaires were completed by physiotherapists from the five regions of the country, with 85.3% working in adult, 5.4% in neonatal, 5.3% in pediatric and 3.8% in mixed intensive care units (pediatric and neonatal). In intensive care units with a physiotherapists available 24 hours/day, physiotherapists worked more frequently (90.6%) in the assembly, titration, and monitoring of noninvasive ventilation (p = 0.001). Most intensive care units with 12-hour/day physiotherapists (25.8%) did not apply any protocol compared to intensive care units with 18-hour/day physiotherapy (9.9%) versus 24 hours/day (10.2%) (p = 0.032). Most of the respondents (51.0%) received remuneration 2 or 3 times the minimum wage, and only 25.1% received an additional payment for working with patients suspected to have or diagnosed with COVID-19; 85.7% of them did not experience a lack of personal protective equipment.
Conclusion:
Intensive care units with 24-hour/day physiotherapists had higher percentages of protocols and noninvasive ventilation for patients with COVID-19. The use of specific resources varied between the types of intensive care units and hospitals and in relation to the physiotherapists’ labor conditions. This study showed that most professionals had little experience in intensive care and low wages.
Keywords:COVID-19Intensive care unitsOccupational risksPhysiotherapistsProfessional trainingRemunerationSurvey and questionnairesWork hoursSee more -
Special Article
First Brazilian recommendation on physiotherapy with sensory motor stimulation in newborns and infants in the intensive care unit
Rev Bras Ter Intensiva. 2021;33(1):12-30
Abstract
Special ArticleFirst Brazilian recommendation on physiotherapy with sensory motor stimulation in newborns and infants in the intensive care unit
Rev Bras Ter Intensiva. 2021;33(1):12-30
DOI 10.5935/0103-507X.20210002
Views2Abstract
Objective:
To present guidelines on sensory motor stimulation for newborns and infants in the intensive care unit.
Methods:
We employed a mixed methods design with a systematic review of the literature and recommendations based on scientific evidence and the opinions of physiotherapists with neonatal expertise. The research included studies published between 2010 and 2018 in the MEDLINE® and Cochrane databases that included newborns (preterm and term) and infants (between 28 days and 6 months of age) hospitalized in the intensive care unit and submitted to sensory motor stimulation methods. The studies found were classified according to the GRADE score by five physiotherapists in different regions of Brazil and presented at eight Scientific Congresses held to discuss the clinical practice guidelines.
Results:
We included 89 articles to construct the clinical practice guidelines. Auditory, gustatory and skin-to-skin stimulation stand out for enhancing vital signs, and tactile-kinesthetic massage and multisensory stimulation stand out for improving weight or sucking.
Conclusion:
Although all modalities have good ratings for pain or stress control, it is recommended that sensory motor stimulation procedures be tailored to the infant’s specific needs and that interventions and be carried out by expert professionals.
Keywords:Child developmentInfantInfant, newbornIntensive care units, neonatalNeuropsychomotor developmentPsychomotor performanceSensory motor stimulationSee more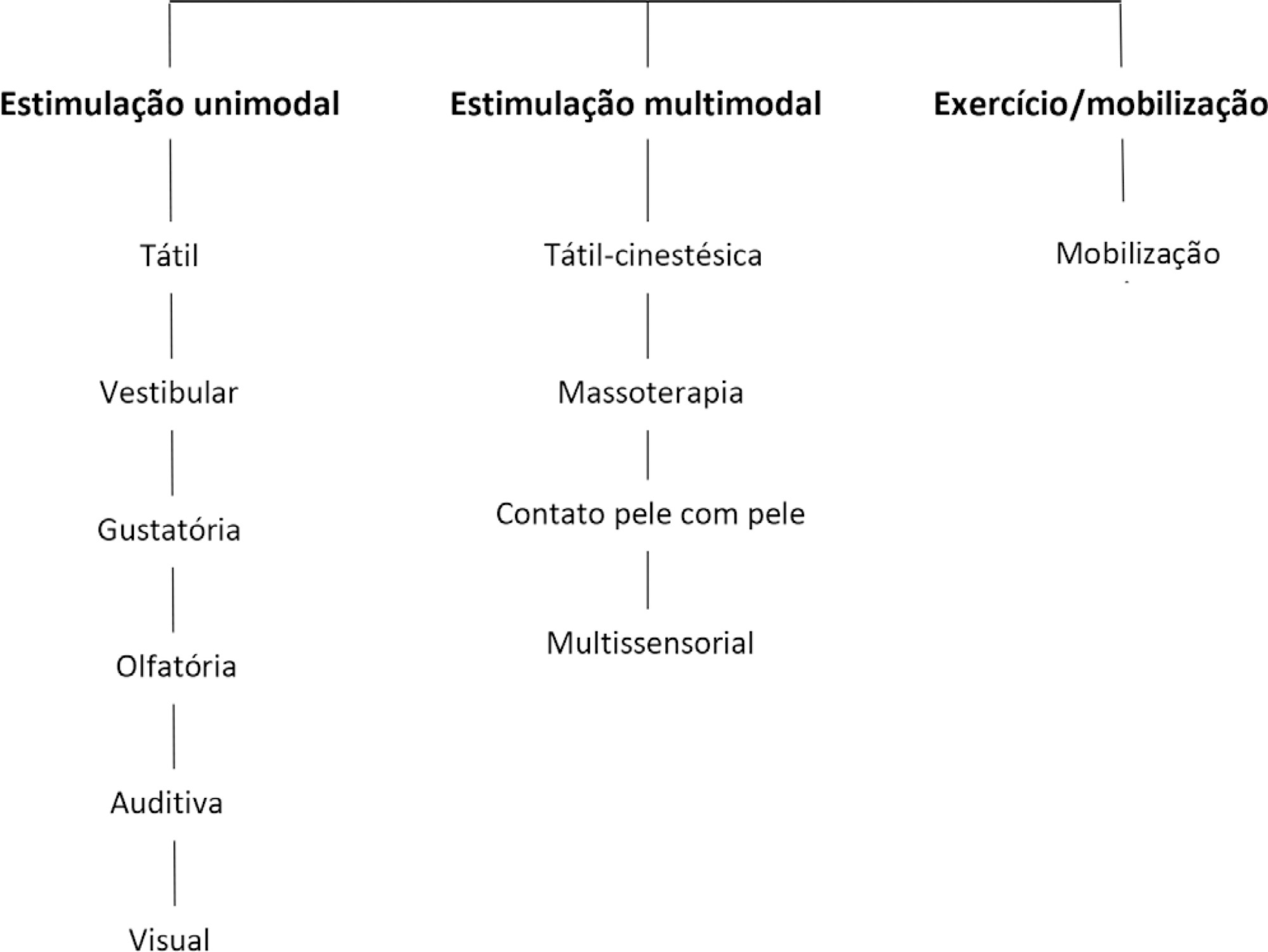
-
Original Article
Frequency and characterization of the use of cuffed tracheal tubes in neonatal and pediatric intensive care units in Brazil
Rev Bras Ter Intensiva. 2020;32(2):235-243
Abstract
Original ArticleFrequency and characterization of the use of cuffed tracheal tubes in neonatal and pediatric intensive care units in Brazil
Rev Bras Ter Intensiva. 2020;32(2):235-243
DOI 10.5935/0103-507X.20200038
Views0ABSTRACT
Objective:
To identify the neonatal, pediatric and mixed (neonatal and pediatric) intensive care units in Brazil that use cuffed tracheal tubes in clinical practice and to describe the characteristics related to the use of protocols and monitoring.
Methods:
To identify the intensive care units in Brazil, the Ministry of Health’s National Registry of Health Facilities was accessed, and information was collected on 693 registered intensive care units. This was an analytical cross-sectional survey conducted through electronic questionnaires sent to 298 neonatal, pediatric and mixed intensive care units in Brazil.
Results:
This study analyzed 146 questionnaires (49.3% from neonatal intensive care units, 35.6% from pediatric intensive care units and 15.1% from mixed pediatric intensive care units). Most of the participating units (78/146) used cuffed tracheal tubes, with a predominance of use in pediatric intensive care units (52/78). Most of the units that used cuffed tracheal tubes applied a cuff pressure monitoring protocol (45/78). The use of cuff monitoring protocols was observed in intensive care units with a physical therapy service exclusive to the unit (38/61) and in those with a physical therapist present 24 hours/day (25/45). The most frequent cause of extubation failure related to the use of cuffed tracheal tubes in pediatric intensive care units was upper airway obstruction.
Conclusion:
In this survey, the use of cuffed tracheal tubes and the application of a cuff pressure monitoring protocol was predominant in pediatric intensive care units. The use of a monitoring protocol was more common in intensive care units that had a physical therapist who was exclusive to the unit and was present 24 hours/day.
Keywords:CannulaInfantIntensive care units, neonatalIntensive care units, pediatricIntubation, intratracheal/instrumentationNewbornTracheaSee more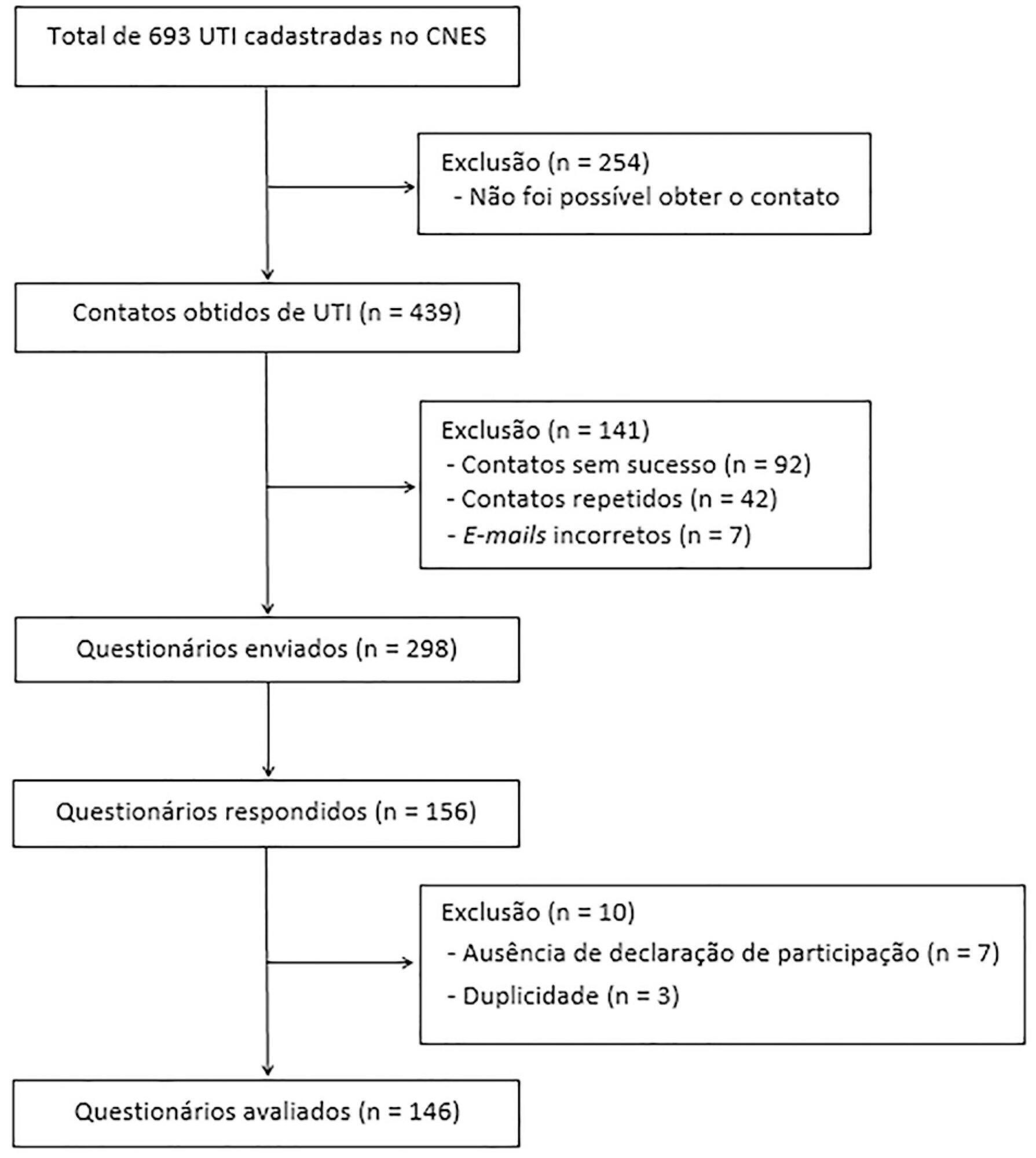
-
Review Articles
Manual hyperinflation in airway clearance in pediatric patients: a systematic review
Rev Bras Ter Intensiva. 2013;25(3):258-262
Abstract
Review ArticlesManual hyperinflation in airway clearance in pediatric patients: a systematic review
Rev Bras Ter Intensiva. 2013;25(3):258-262
DOI 10.5935/0103-507X.20130043
Views0See moreOBJECTIVE:
To perform an assessment of the available literature on manual hyperinflation as a respiratory physical therapy technique used in pediatric patients, with the main outcome of achieving airway clearance.
METHODS:
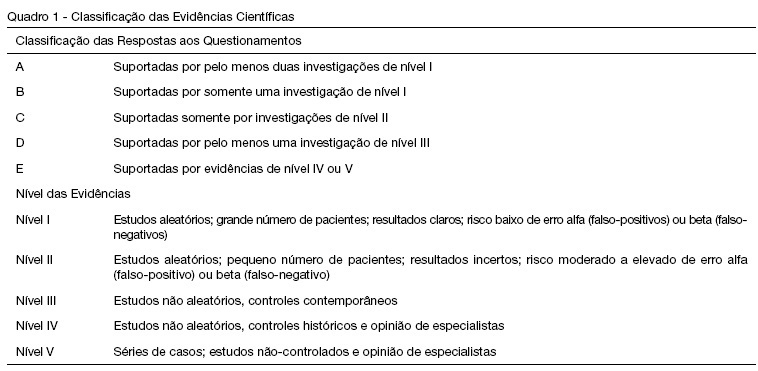
We reviewed articles included in the Lilacs (Latin American and Caribbean Literature on Health Sciences/Literatura Latino Americana e do Caribe em Ciências da Saúde), Cochrane Library, Medline (via Virtual Health Library and PubMed), SciELO (Scientific Electronic Library), and PEDro (Physiotherapy Evidence Database) databases from 2002 to 2013 using the following search terms: “physiotherapy (techniques)”, “respiratory therapy”, “intensive care”, and “airway clearance”. The selected studies were classified according to the level of evidence and grades of recommendation (method of the Oxford Centre for Evidence-Based Medicine) by two examiners, while a third examiner repeated the search and analysis and checked the classification of the articles.
RESULTS:
Three articles were included for analysis, comprising 250 children (aged 0 to 16 years). The main diagnoses were acute respiratory failure, recovery following heart congenital disease and upper abdominal surgery, bone marrow transplantation, asthma, tracheal reconstruction, brain injury, airway injury, and heterogeneous lung diseases. The studies were classified as having a level of evidence 2C and grade of recommendation C.
CONCLUSIONS:
Manual hyperinflation appeared useful for airway clearance in the investigated population, although the evidence available in the literature remains insufficient. Therefore, controlled randomized studies are needed to establish the safety and efficacy of manual hyperinflation in pediatric patients. However, manual hyperinflation must be performed by trained physical therapists only.
-
Special Article
I Brazilian guidelines for respiratory physiotherapy in pediatric and neonatal intensive care units
Rev Bras Ter Intensiva. 2012;24(2):119-129
Abstract
Special ArticleI Brazilian guidelines for respiratory physiotherapy in pediatric and neonatal intensive care units
Rev Bras Ter Intensiva. 2012;24(2):119-129
DOI 10.1590/S0103-507X2012000200005
Views0Developing guidelines for the role of the physiotherapist in neonatal and pediatric intensive care units is essential because these professionals are responsible for the rehabilitation of critically ill patients. Rehabilitation includes the evaluation and prevention of functional kinetic alterations, application of treatment interventions (respiratory and/or motor physiotherapy), control and application of medical gases, care of mechanical ventilation, weaning and extubation, tracheal gas insufflation, inflation/deflation of the endotracheal cuff protocol, and surfactant application, aiming to allow patients to have a full recovery and return to their functional activities. In this article, we present guidelines that are intended to guide the physiotherapist in some of the prevention/treatment interventions in respiratory therapy (airway clearance, lung expansion, position in bed, airway suction, drug inhalation, and cough assist), which help in the rehabilitation process of newborns and children in intensive care units during mechanical ventilation and up to 12 hours following extubation.
Keywords:ChildIntensive care, neonatalPhysical therapy modalitiesRehabilitationRespiration, artificialRespiratory therapySee more -
Cardiorespiratory repercussions of the peritoneal dialysis in critically ill children
Rev Bras Ter Intensiva. 2008;20(1):31-36
Abstract
Cardiorespiratory repercussions of the peritoneal dialysis in critically ill children
Rev Bras Ter Intensiva. 2008;20(1):31-36
DOI 10.1590/S0103-507X2008000100005
Views0See moreBACKGROUND AND OBJECTIVES: Peritoneal dialysis (PD) is frequently used to replace glomerular filtration and to control acid-base, electrolyte and fluid disturbances in critically ill children with acute renal failure. However, cardiorespiratory changes can happen during this procedure. The objective of this review is to describe the PD cardio-respiratory repercutions in the pediatric patient and the evidence level of the studies that approach these repercutions. METHODS: Bibliographic revision about PD cardio-respiratory repercutions in the pediatric patient. Medline, Ovid e Lilacs databases were searched for articles from 1990 to 2007 with the following key words in Portuguese, English and Spanish: diálise peritoneal, efeitos hemodinâmicos, complicações respiratórias, complicações cardíacas, Pediatria; peritoneal dialysis, hemodynamic effects, respiratory complications, cardiac complications, Pediatric; peritoneal diálisis, efecto hemodinámico, complicaciones respiratorias, complicaciones cardiacas, Pediatria. The retrieved articles were classified according to Cook et al. 1992. RESULTS: Thirteen articles were retrieved, 8 of them were about cardiorespiratory repercussions and five approached respiratory repercussions of PD. These studies evaluated 178 critically ill patients, from newborns to adolescents. Among the respiratory repercutions during PD the most frequent ones were decrease of the pulmonary compliance and arterial oxygen partial pressure and increase of airway resistance and carbon dioxide partial pressure; after the infusion of PD fluid the studies pointed out an increased arterial oxygen partial pressure/ inspired oxygen fraction relation and diminution of the alveolar-arterial difference and oxygenation index. Increase of the mean arterial pressure, pulmonary artery pressure, right and left atrial pressure and systemic vascular resistance and, reduction of the central venous pressure were the described cardio-circulatory repercutions during PD. CONCLUSIONS: Pulmonary volumes, gas exchange and cardio-circulatory alterations are the most frequent complications during and after PD in the pediatric patient. Therefore critically ill pediatric patients with acute renal failure needing PD should be monitored during and after this procedure to avoid clinical deterioration and to educate the multi-professional team.
-
Post cardiac surgery In children: extubation failure predictor’s
Rev Bras Ter Intensiva. 2008;20(1):57-62
Abstract
Post cardiac surgery In children: extubation failure predictor’s
Rev Bras Ter Intensiva. 2008;20(1):57-62
DOI 10.1590/S0103-507X2008000100009
Views0See moreBACKGROUND AND OBJECTIVES: It is important to know the risk factors for extubation failure (EF) in children submitted to cardiac surgery in order to avoid inherent events due to reintubation (airways injury, usage of medications, cardiovascular changes) and because of prolonged ventilatory support (pneumonias, reduction of the ventilatory muscles strength). The objective of this study is to evaluate mechanical ventilation (MV) parameters, ventilatory mechanics [rapid shallow breathing index (RSBI), ventilatory muscles force [the maximum inspiratory pressure (MIP), the maximum expiratory pressure (MEP) and the load/force balance (LFB)] and blood gases before and after extubation in pediatric patients undergoing cardiac surgery. METHODS: Prospective (March 2004 to March 2006) observational cross sectional study, enrolling children submitted to cardiac surgery admitted to an university PICU hospital and considered able to be extubated. With the tracheal tube in situ and maintaining the children spontaneously breathing we evaluate: expiratory minute volume (V E), MIP and MEP. We calculated the RSBI [(RR/VT)/Weight)], LFB [15x [(3xMAP)/MIP] + 0.03 x RSBI-5], the mean airway pressure (MAP) [MAP={(PIP-PEEP)x[Ti/(Te+Ti)]}+PEEP] and the oxygenation index (OI) [OI=(FiO2 x MAP/PaO2)x100]. Arterial blood gas was collected one hour before extubation. If after 48 hours there was no need to reintubate the patient the extubation was considered successful (SE). RESULTS: 59 children were included. EF was observed in 19% (11/59). Median (QI25%-75%) for age, weight, MAP, OI, duration of MV after cardiac surgery (DMV) were respectively, 36 (12-82) months, 12 (8-20) kg, 8 (6-9), 2 (2-5), 1 (1-3) days. Median (QI25-75%) of EF in relation to SE for OI, LFB and DMV were respectively 5(3-8) versus 2(2-4), p = 0.005; [8(6-11) versus 5(4-6), p =0.002 and 3(2-5) versus 1(1-2) days, p = 0.026. Mean ± SD of EF in relation to SE for V E, PaO2 and MIP were respectively 1.7 ± 0.82 versus 3 ± 2.7 mL/kg/min, p = 0.003); 64 ± 34 versus 111 ± 50 mmHg, p = 0.002 and 53 ± 18 versus 78 ± 28 cmH2O; p=0.002. Concerning the risk factors for EF: OI > 2 (area under the ROC 0.74, p = 0.017) and LFB > 4 (area under the ROC 0.80, p = 0.002), achieved a sensibility of 100% and specificity of 80%; MIP < -35 cmH2O (area under the ROC 0.23; p= 0.004) achieved a sensibility of 80% and specificity of 60%. CONCLUSIONS: EF in children submitted to cardiac surgery is related to OI > 2, LFB > 4, DMV > 3 days; V E < 1.7 mL/kg/min, PaO2 < 64 mmHg and MIP < - 53 cmH2O. The kind of cardiac defect, MAP, RSBI and arterial blood gas were not related to EF.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




